Imaging Sci Dent.
2018 Mar;48(1):51-57. 10.5624/isd.2018.48.1.51.
Quantitative evaluation of palatal bone thickness in patients with normal and open vertical skeletal configurations using cone-beam computed tomography
- Affiliations
-
- 1Department of Orthodontics and Pediatric Dentistry, Faculty of Dentistry, Chiang Mai University, Chiang Mai, Thailand. dhirawat.j@gmail.com
- 2Department of Oral Biology and Diagnostic Sciences, Faculty of Dentistry, Chiang Mai University, Chiang Mai, Thailand.
- KMID: 2406983
- DOI: http://doi.org/10.5624/isd.2018.48.1.51
Abstract
- PURPOSE
To perform a comparative analysis of the palatal bone thickness in Thai patients exhibiting class I malocclusion according to whether they exhibited a normal or open vertical skeletal configuration using cone-beam computed tomography (CBCT).
MATERIALS AND METHODS
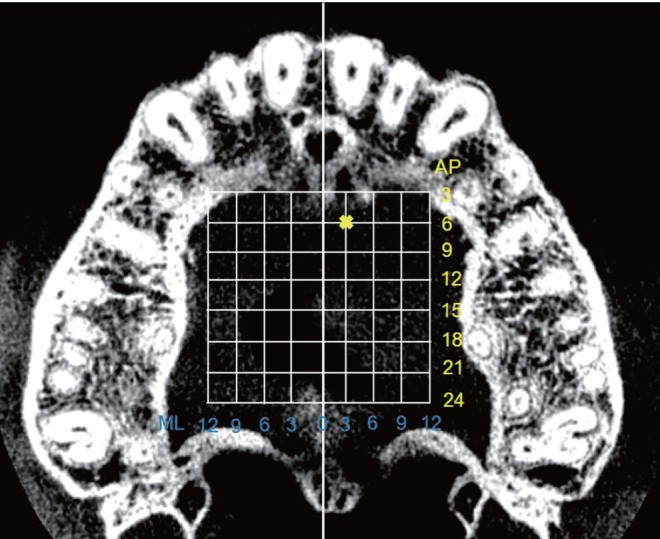
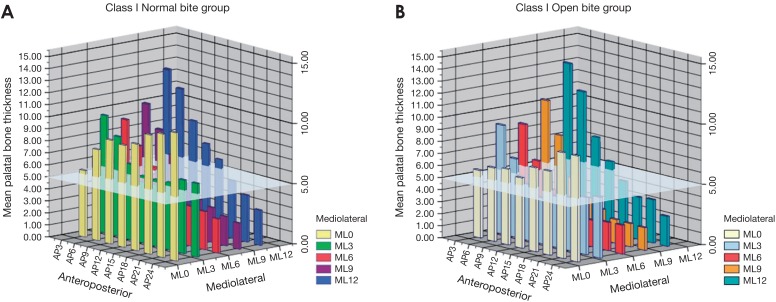
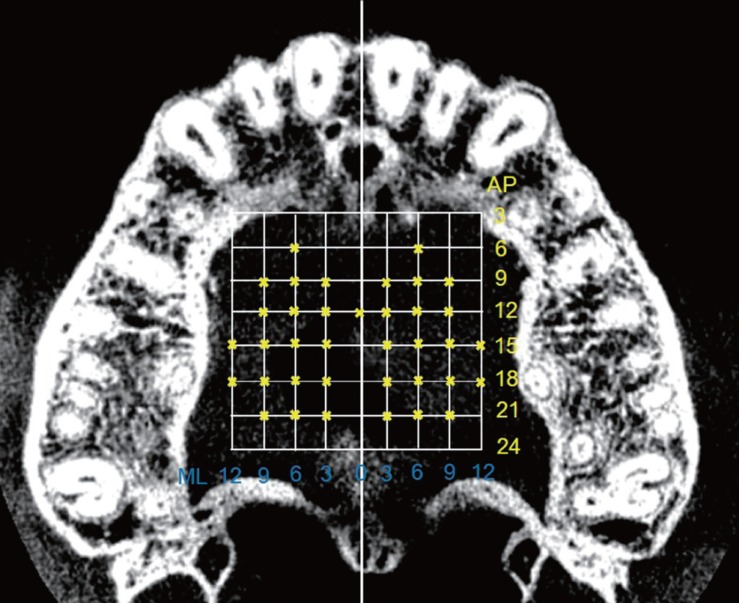
Thirty CBCT images of Thai orthodontic patients (15-30 years of age) exhibiting class I malocclusion with a normal or open vertical skeletal configuration were selected. Palatal bone thickness was measured in a 3.0-mm grid pattern on both the right and left sides. The palatal bone thickness of the normal-bite and open-bite groups was compared using the independent t-test. The level of significance was established at P < .05.
RESULTS
The palatal bone thickness in the normal-bite group ranged from 2.2±1.0 mm to 12.6±4.1 mm. The palatal bone thickness in the open-bite group ranged from 1.9±1.1 mm to 13.2±2.3 mm. The palatal bone thickness was lower at almost all sites in patients with open bite than in those with normal bite. Significant differences were found at almost all anteroposterior sites along the 3 most medial sections (3.0, 6.0, and 9.0 mm lateral to the midsagittal plane) (P < .05).
CONCLUSION
Class I malocclusion with open vertical skeletal configuration may affect palatal bone thickness, so the placement of temporary anchorage devices or miniscrew implants in the palatal area in such patients should be performed with caution.
MeSH Terms
Figure
Cited by 1 articles
-
Osteometric Analysis of Palatal Bone Thickness for Orthodontic Miniscrew Placement
Sun-Kyoung Yu, Yonghwa Cho, Heung-Joong Kim, Jin Woong Lim
Anat Biol Anthropol. 2019;32(3):93-99. doi: 10.11637/aba.2019.32.3.93.
Reference
-
1. Lin LH, Huang GW, Chen CS. Etiology and treatment modalities of anterior open bite malocclusion. J Exp Clin Med. 2013; 5:1–4.
Article2. Antoszewska J, Papadopoulos MA, Park HS, Ludwig B. Five-year experience with orthodontic miniscrew implants: a retrospective investigation of factors influencing success rates. Am J Orthod Dentofacial Orthop. 2009; 136:158.e1–158.e10. PMID: 19651342.
Article3. Manni A, Cozzani M, Tamborrino F, De Rinaldis S, Menini A. Factors influencing the stability of miniscrews. A retrospective study on 300 miniscrews. Eur J Orthod. 2011; 33:388–395. PMID: 20926556.
Article4. Moon CH, Park HK, Nam JS, Im JS, Baek SH. Relationship between vertical skeletal pattern and success rate of orthodontic mini-implants. Am J Orthod Dentofacial Orthop. 2010; 138:51–57. PMID: 20620833.
Article5. Ozdemir F, Tozlu M, Germec Cakan D. Quantitative evaluation of alveolar cortical bone density in adults with different vertical facial types using cone-beam computed tomography. Korean J Orthod. 2014; 44:36–43. PMID: 24511514.
Article6. Ozdemir F, Tozlu M, Germec-Cakan D. Cortical bone thickness of the alveolar process measured with cone-beam computed tomography in patients with different facial types. Am J Orthod Dentofacial Orthop. 2013; 143:190–196. PMID: 23374925.
Article7. Ludwig B, Glasl B, Bowman SJ, Wilmes B, Kinzinger GS, Lisson JA. Anatomical guidelines for miniscrew insertion: palatal sites. J Clin Orthod. 2011; 45:433–441. PMID: 22094724.8. Baumgaertel S. Quantitative investigation of palatal bone depth and cortical bone thickness for mini-implant placement in adults. Am J Orthod Dentofacial Orthop. 2009; 136:104–108. PMID: 19577156.
Article9. Kang S, Lee SJ, Ahn SJ, Heo MS, Kim TW. Bone thickness of the palate for orthodontic mini-implant anchorage in adults. Am J Orthod Dentofacial Orthop. 2007; 131:S74–S81. PMID: 17448390.
Article10. Gracco A, Lombardo L, Cozzani M, Siciliani G. Quantitative cone-beam computed tomography evaluation of palatal bone thickness for orthodontic miniscrew placement. Am J Orthod Dentofacial Orthop. 2008; 134:361–369. PMID: 18774082.
Article11. Nakahara K, Matsunaga S, Abe S, Tamatsu Y, Kageyama I, Hashimoto M, et al. Evaluation of the palatal bone for placement of orthodontic mini-implants in Japanese adults. Cranio. 2012; 30:72–79. PMID: 22435178.
Article12. Gahleitner A, Podesser B, Schick S, Watzek G, Imhof H. Dental CT and orthodontic implants: imaging technique and assessment of available bone volume in the hard palate. Eur J Radiol. 2004; 51:257–262. PMID: 15294334.
Article13. Stockmann P, Schlegel KA, Srour S, Neukam FW, Fenner M, Felszeghy E. Which region of the median palate is a suitable location of temporary orthodontic anchorage devices? A histomorphometric study on human cadavers aged 15–20 years. Clin Oral Implants Res. 2009; 20:306–312. PMID: 19397643.
Article14. Henriksen B, Bavitz B, Kelly B, Harn SD. Evaluation of bone thickness in the anterior hard palate relative to midsagittal orthodontic implants. Int J Oral Maxillofac Implants. 2003; 18:578–581. PMID: 12939012.15. Jung BA, Wehrbein H, Heuser L, Kunkel M. Vertical palatal bone dimensions on lateral cephalometry and cone-beam computed tomography: implications for palatal implant placement. Clin Oral Implants Res. 2011; 22:664–668. PMID: 21044170.
Article16. Wehrbein H, Merz BR, Diedrich P. Palatal bone support for orthodontic implant anchorage-a clinical and radiological study. Eur J Orthod. 1999; 21:65–70. PMID: 10191579.17. Winsauer H, Vlachojannis C, Bumann A, Vlachojannis J, Chrubasik S. Paramedian vertical palatal bone height for mini-implant insertion: a systematic review. Eur J Orthod. 2014; 36:541–549. PMID: 23221896.
Article18. Bernhart T, Vollgruber A, Gahleitner A, Dörtbudak O, Haas R. Alternative to the median region of the palate for placement of an orthodontic implant. Clin Oral Implants Res. 2000; 11:595–601. PMID: 11168253.
Article19. Frost HM. The mechanostat: a proposed pathogenic mechanism of osteoporoses and the bone mass effects of the mechanical and nonmechanical agents. Bone Miner. 1987; 2:73–85. PMID: 3333019.20. Horner KA, Behrents RG, Kim KB, Buschang PH. Cortical bone and ridge thickness of hyperdivergent and hypodivergent adults. Am J Orthod Dentofacial Orthop. 2012; 142:170–178. PMID: 22858325.
Article21. Janovic A, Milovanovic P, Saveljic I, Nikolic D, Hahn M, Rakocevic Z, et al. Microstructural properties of the mid-facial bones in relation to the distribution of occlusal loading. Bone. 2014; 68:108–114. PMID: 25093265.
Article22. Strait DS, Richmond BG, Spencer MA, Ross CF, Dechow PC, Wood BA. Masticatory biomechanics and its relevance to early hominid phylogeny: an examination of palatal thickness using finite-element analysis. J Hum Evol. 2007; 52:585–599. PMID: 17386938.
Article23. Menegaz RA, Sublett SV, Figueroa SD, Hoffman TJ, Ravosa MJ. Phenotypic plasticity and function of the hard palate in growing rabbits. Anat Rec (Hoboken). 2009; 292:277–284. PMID: 19089904.
Article24. Janovic A, Saveljic I, Vukicevic A, Nikolic D, Rakocevic Z, Jovicic G, et al. Occlusal load distribution through the cortical and trabecular bone of the human mid-facial skeleton in natural dentition: a three-dimensional finite element study. Ann Anat. 2015; 197:16–23. PMID: 25458179.
Article25. Toro-Ibacache V, Zapata Muñoz V, O'Higgins P. The relationship between skull morphology, masticatory muscle force and cranial skeletal deformation during biting. Ann Anat. 2016; 203:59–68. PMID: 25829126.
Article26. Johari M, Kaviani F, Saeedi A. Relationship between the thickness of cortical bone at maxillary mid-palatal area and facial height using CBCT. Open Dent J. 2015; 9:287–291. PMID: 26464597.
Article27. Kyung SH. A study on the bone thickness of midpalatal suture area for miniscrew insertion. Korean J Orthod. 2004; 34:63–70.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Detection of maxillary second molar with two palatal roots using cone beam computed tomography: a case report
- Quantitative evaluation of alveolar cortical bone density in adults with different vertical facial types using cone-beam computed tomography
- Assessment of the relationship between the maxillary molars and adjacent structures using cone beam computed tomography
- Stability of dental, alveolar, and skeletal changes after miniscrew-assisted rapid palatal expansion
- A cone-beam computed tomography evaluation of buccal bone thickness following maxillary expansion