J Korean Ophthalmol Soc.
2018 Mar;59(3):209-216. 10.3341/jkos.2018.59.3.209.
Clinical Aspects and Treatment Outcomes of Moraxella keratitis
- Affiliations
-
- 1Department of Ophthalmology, Chonbuk National University Medical School, Jeonju, Korea. you2ic@daum.net
- 2Research Institute of Clinical Medicine, Chonbuk National University, Jeonju, Korea.
- 3Biomedical Research Institute, Chonbuk National University Hospital, Jeonju, Korea.
- 4Pureun Eye Center, Jeonju, Korea.
- KMID: 2406954
- DOI: http://doi.org/10.3341/jkos.2018.59.3.209
Abstract
- PURPOSE
To analyze the clinical presentation, predisposing risk factors, and evaluate the treatment outcomes of Moraxella keratitis.
METHODS
A retrospective analysis was conducted of 12 culture positive cases of Moraxella keratitis from hospital records between March 2001 and November 2015 at a tertiary hospital to identify and analyze its risk factors, causative microbial organisms, clinical features, and therapeutic outcomes.
RESULTS
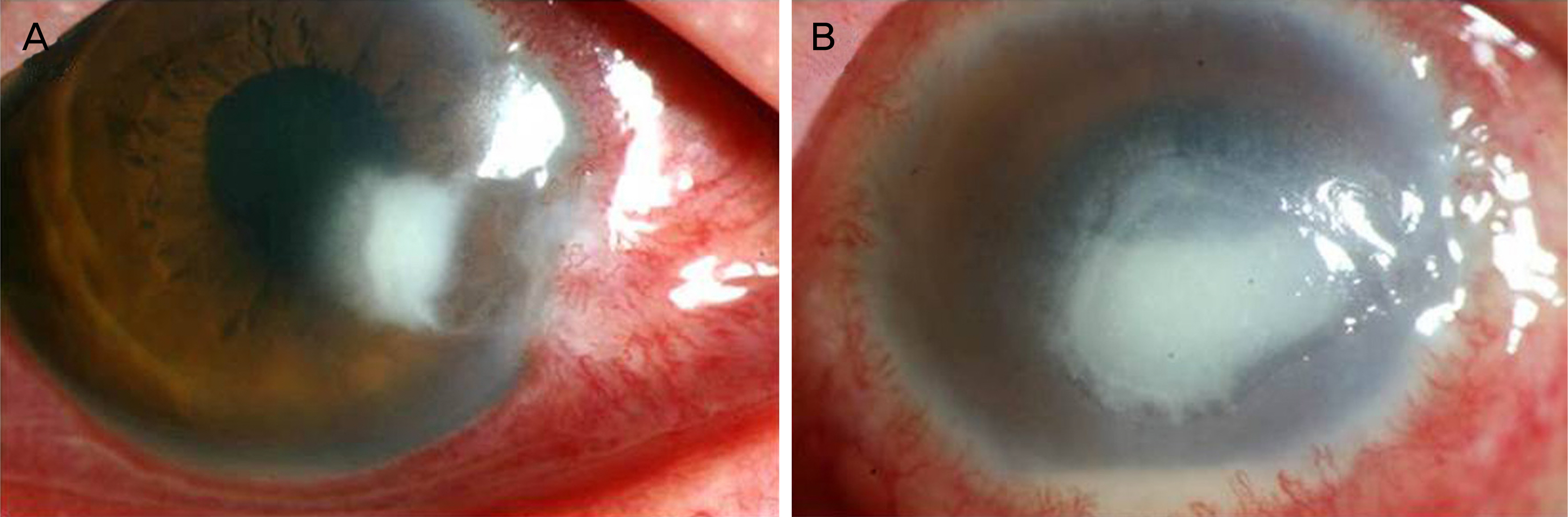
The mean patient age was 68 years (range, 46-86). The most common cause of keratitis was trauma (six eyes, 50.0%), and half of these patients had diabetes mellitus (three patients, 25.0%). Two patients (16.6%) were previously treated with penetrating keratoplasty. The locations of keratitis involved the central (50.0%) and paracentral (50.0%) regions. Round-shaped corneal infiltration was found in seven eyes (58.3%), and irregular-shaped infiltration was found in five eyes (41.7%). Hypopyon was observed in five eyes (41.7%). All Moraxella isolates were susceptible to aminoglycosides and fluoroquinolones. The isolates from three patients were resistant to trimethoprim/sulfamethoxazole. The mean complete epithelial healing time was 32.4 days. The final visual acuity was 20/1,000 or less in seven eyes (58.3%). Three eyes developed corneal perforations and eventually underwent evisceration.
CONCLUSIONS
In the Republic of Korea, Moraxella keratitis frequently occurs in eyes with trauma. The treatment response is very slow and has a poor visual outcome; thus, a long period of antibiotic therapy is necessary.
MeSH Terms
Figure
Cited by 1 articles
-
Corneal Collagen Cross-linking for Corneal Ulcer from Moraxella Group
Sang Earn Woo, Si Hyung Lee
J Korean Ophthalmol Soc. 2020;61(2):200-204. doi: 10.3341/jkos.2020.61.2.200.
Reference
-
1). Srinivasan M, Mascarenhas J, Rajaraman R, et al. The steroids for corneal ulcers trial: study design and baseline characteristics. Arch Ophthalmol. 2012; 130:151–7.2). National Surveillance of Infectious Keratitis in Japan. National Surveillance of Infectious Keratitis in Japan–current status of isolates, patient background, and treatment. Nippon Ganka Gakkai Zasshi. 2006; 110:961–72.3). Das S, Constantinou M, Daniell M, Taylor HR. Moraxella keratitis: predisposing factors and clinical review of 95 cases. Br J Ophthalmol. 2006; 90:1236–8.
Article4). Garg P, Mathur U, Athmanathan S, Rao GN. Treatment outcome of Moraxella keratitis: our experience with 18 cases–a retrospective review. Cornea. 1999; 18:176–81.5). Inoue H, Suzuki T, Inoue T, et al. Clinical characteristics and bacteriological profile of Moraxella keratitis. Cornea. 2015; 34:1105–9.
Article6). Musch DC, Sugar A, Meyer RF. Demographic and predisposing factors in corneal ulceration. Arch Ophthalmol. 1983; 101:1545–8.
Article7). Benson WH, Lanier JD. Current diagnosis and treatment of corneal ulcers. Curr Opin Ophthalmol. 1998; 9:45–9.
Article8). Marioneaux SJ, Cohen EJ, Arentsen JJ, Laibson PR. Moraxella keratitis. Cornea. 1991; 10:21–4.
Article9). Baum J, Fedukowicz HB, Jordan A. A survey of Moraxella corneal ulcers in a derelict population. Am J Ophthalmol. 1980; 90:476–80.
Article10). Heidemann DG, Alfonso E, Forster RK, et al. Branhamella catarrhalis keratitis. Am J Ophthalmol. 1987; 103:576–81.
Article11). Mian SI, Malta JB. Moraxella keratitis: risk factors, presentation, and management. Acta Ophthalmol. 2011; 89:e208–9.
Article12). Varaprasathan G, Miller K, Lietman T, et al. Trends in the etiology of infectious corneal ulcers at the F. I. Proctor Foundation. Cornea. 2004; 23:360–4.
Article13). Cho EY, Lee SB. Gram-negative bacterial keratitis: a 15-year review of clinical aspects. J Korean Ophthalmol Soc. 2015; 56:1479–88.
Article14). Hahn YH, Hahn TW, Tchah H, et al. Epidemiology of infectious Keratitis(II): a multi-center study. J Korean Ophthalmol Soc. 2001; 42:247–65.15). Van Bijsterveld OP. Host-parasite relationship and taxonomic position of Moraxella and morphologically related organisms. Am J Ophthalmol. 1973; 76:545–54.
Article16). Cobo LM, Coster DJ, Peacock J. Moraxella keratitis in a nonalcoholic population. Br J Ophthalmol. 1981; 65:683–6.
Article17). Suzuki T, Ohashi Y. Combination effect of antibiotics against bacteria isolated from keratitis using fractional inhibitory concentration index. Cornea. 2013; 32:e156–60.
Article18). Kowalski RP, Kowalski TA, Shanks RM, et al. In vitro comparison of combination-and monotherapy for the empiric and optimal coverage of bacterial keratitis based on incidence of infection. Cornea. 2013; 32:830–4.19). Loh RS, Chan CM, Ti SE, et al. Emerging prevalence of micro-sporidial keratitis in Singapore: epidemiology, clinical features, and management. Ophthalmology. 2009; 116:2348–53.20). Ly CN, Pham JN, Badenoch PR, et al. Bacteria commonly isolated from keratitis specimens retain antibiotic susceptibility to fluoroquinolones and gentamicin plus cephalothin. Clin Exp Ophthalmol. 2006; 34:44–50.
Article21). Stern GA. Moraxella corneal ulcers: poor response to medical treatment. Ann Ophthalmol. 1982; 14:295–8.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Moraxella Keratitis
- Moraxella Meningoencephalitis: Case Report and Review of the Literature
- Analysis on Inpatients With Infectious Keratitis: Causative Organisms, Clinical Aspects and Risk Factors
- The Effect of Subconjunctival Injection of Tathion on Some Keratitis
- Analysis on Elderly Inpatients with Infectious Keratitis: Causative Organisms, Clinical Aspects, and Risk Factors