J Educ Eval Health Prof.
2017;14:22. 10.3352/jeehp.2017.14.22.
Unmet needs in health training among nurses in rural Chinese township health centers: a cross-sectional hospital-based study
- Affiliations
-
- 1First Affiliated Hospital of Guangxi Medical University, Guangxi, China. 12466303@qq.com
- 2The Maternal and Child Hospital of Guangxi Zhuang Autonomous Region, Guangxi, China.
- 3Department of Plastic and Aesthetic Surgery, Nan Fang Hospital, Southern Medical University, Guangdong, China.
- KMID: 2406685
- DOI: http://doi.org/10.3352/jeehp.2017.14.22
Abstract
- PURPOSE
Maintaining a sufficient and competent rural nursing workforce is an important goal of the Chinese health delivery system. However, few studies have investigated the health training status or conducted a needs assessment of rural Chinese nurses during this time of great transformations in health policy. This study was conducted to explore the current health training status of nurses working in rural Chinese township health centers (THCs) and to ascertain their perceived needs.
METHODS
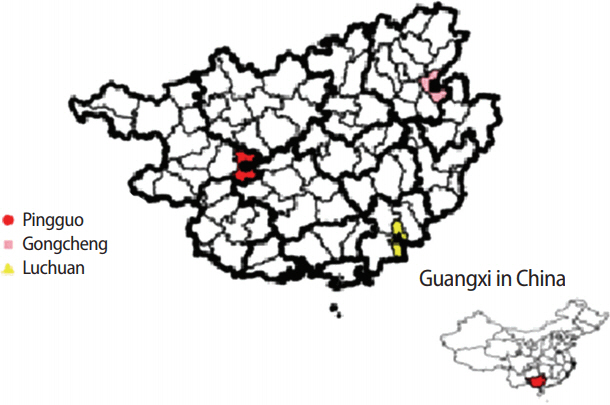
A cross-sectional survey using a self-administered structured questionnaire was conducted among 240 THC nurses in Guangxi Zhuang Autonomous Region, China from March 2014 to August 2014. The survey questionnaire was adapted from the Second Chinese Survey of Demographic Data and Training Demand for Health Professionals in THCs developed by the Ministry of Education.
RESULTS
The nurses in THCs were young, with a low educational level. Their perceived needs for health training included further clinical studies at city-level hospitals to improve their skills and theoretical studies at medical universities in emergency medicine and general practice. Overall, 71.9% of the nurses with a secondary technical school background expected to pursue junior college studies, and 68.5% of the nurses with a junior college education expected to pursue a bachelor's degree. A decentralized program with theoretical studies at medical universities and practical studies at county hospitals was regarded as feasible by 66.9% of the respondents.
CONCLUSION
Health-training programs for nurses in Chinese THCs must be improved in terms of coverage, delivery mode, and content. A decentralized degree-linked training program in which medical universities and city hospitals collaborate would be an appropriate mode of delivery.
Keyword
MeSH Terms
Figure
Reference
-
References
1. Gao LL, Chan SW, Cheng BS. The past, present and future of nursing education in the People’s Republic of China: a discussion paper. J Adv Nurs. 2012; 68:1429–1438. https://doi.org/10.1111/j.1365-2648.2011.05828.x.
Article2. Li X, Chongsuvivatwong V, Xia X, Sangsupawanich P, Zheng W, Ma K. Revisiting current “barefoot doctors” in border areas of China: system of services, financial issue and clinical practice prior to introducing integrated management of childhood illness (IMCI). BMC Public Health. 2012; 12:620. https://doi.org/10.1186/1471-2458-12-620.
Article3. Song K, Scott A, Sivey P, Meng Q. Improving Chinese primary care providers’ recruitment and retention: a discrete choice experiment. Health Policy Plan. 2015; 30:68–77. https://doi.org/10.1093/heapol/czt098.
Article4. Yi Y, Chongsuvivatwong V, Sriplung H, Hu G, McNeil E, Feng Q, Zhou H, Wei B. Unmet needs in continuing medical education programs for rural Chinese township health professionals. J Educ Eval Health Prof. 2015; 12:25. https://doi.org/10.3352/jeehp.2015.12.25.
Article5. Huang L, Yang D, Yao L, Liu Z, Wu W. Guangxi’s rural health insurance scheme: evidence from an ethnic minority region in China. Rural Remote Health. 2013; 13:2454.
Article6. You LM, Ke YY, Zheng J, Wan LH. The development and issues of nursing education in China: a national data analysis. Nurse Educ Today. 2015; 35:310–314. https://doi.org/10.1016/j.nedt.2014.10.004.
Article7. Li X, Liu J, Huang J, Qian Y, Che L. An analysis of the current educational status and future training needs of China’s rural doctors in 2011. Postgrad Med J. 2013; 89:202–208. https://doi.org/10.1136/postgradmedj-2012-131094.
Article8. R Core Team. R: a language and environment for statistical computing [Internet]. Vienna: R Foundation for Statistical Computing;2015. [cited 2016 June 21]. Available from: http://www.R-project.org/.9. Virasakdi Chongsuvivatwong. Epicalc: epidemiological calculator: R package version 2.15.1.0 [Internet]. Vienna: R Foundation for Statistical Computing;2012. [cited 2015 May 12]. Available from: http://cran.R-project.Org/package=epicalc.10. Hu G, Yi Y. Is a decentralized continuing medical education program feasible for Chinese rural health professionals? J Educ Eval Health Prof. 2016; 13:18. https://doi.org/10.3352/jeehp.2016.13.18.
Article11. Qing Y, Hu G, Chen Q, Peng H, Li K, Wei J, Yi Y. Factors that influence the choice to work in rural township health centers among 4,669 clinical medical students from five medical universities in Guangxi, China. J Educ Eval Health Prof. 2015; 12:40. https://doi.org/10.3352/jeehp.2015.12.40.
Article12. Skaalvik MW, Gaski M, Norbye B. Decentralized nursing education in northern Norway: a basis for continuing education to meet competence needs in rural Arctic healthcare services. Int J Circumpolar Health. 2014; 73:25328. https://doi.org/10.3402/ijch.v73.25328.
Article13. Oliveira KD, North S, Beck B, Hopp J. Promoting collaboration and cultural competence for physician assistant and physical therapist students: a cross-cultural decentralized interprofessional education (IPE) model. J Educ Eval Health Prof. 2015; 12:20. https://doi.org/10.3352/jeehp.2015.12.20.
Article14. Gong P, Liang S, Carlton EJ, Jiang Q, Wu J, Wang L, Remais JV. Urbanisation and health in China. Lancet. 2012; 379:843–852. https://doi.org/10.1016/S0140-6736(11)61878-3.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Effect of Workplace Violence on Depressive Symptoms and the Mediating Role of Psychological Capital in Chinese Township General Practitioners and Nurses: A Cross-Sectional Study
- Unmet needs in continuing medical education programs for rural Chinese township health professionals
- Is a decentralized continuing medical education program feasible for Chinese rural health professionals?
- Factors that influence the choice to work in rural township health centers among 4,669 clinical medical students from five medical universities in Guangxi, China
- Factors Associated with Nurse Self-Leadership: A Cross-Sectional Study of Nurses Working at Public Health Centers and Primary Healthcare Posts