Anesth Pain Med.
2017 Oct;12(4):363-370. 10.17085/apm.2017.12.4.363.
The effects of epidural versus intravenous patient-controlled analgesia on postoperative outcomes in elderly patients who have undergone gastrectomy: a retrospective trial
- Affiliations
-
- 1Department of Anesthesiology and Pain Medicine, Korea Cancer Center Hospital, Seoul, Korea. jiheui0255@naver.com
- KMID: 2405856
- DOI: http://doi.org/10.17085/apm.2017.12.4.363
Abstract
- BACKGROUND
Efforts for improving surgical outcomes in elderly patients should include the prevention of perioperative complications and proper postoperative pain management. Epidural analgesia is effective in decreasing perioperative stress and postoperative complications, and in improving recovery. Recently, it has been suggested that epidural analgesia may attenuate immune suppression during the perioperative period and lead to reductions in cancer recurrence and improvements in overall survival. Assuming that these effects of epidural analgesia are present in vulnerable elderly patients, we compared the efficacy of epidural patient-controlled analgesia and intravenous patientcontrolled analgesia on postoperative outcomes in elderly patients who had undergone gastrectomy.
METHODS
We evaluated 214 elderly patients who had undergone elective open gastrectomy for gastric cancer from 2011 to 2014. The demographic characteristics, analgesic efficacy, complications within the first 30 postoperative days, hospital stay, 24-month postoperative morbidity, cancer recurrence, and mortality were studied retrospectively.
RESULTS
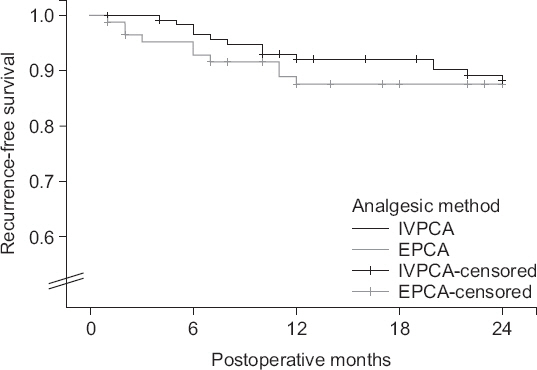
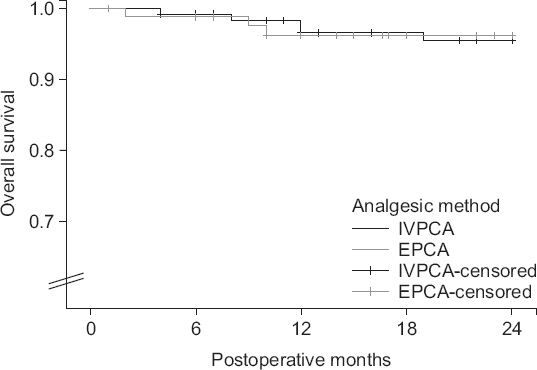
Two-hundred and five patients were analyzed. Eighty-five patients received epidural patient-controlled analgesia (EPCA group) and 120 patients received intravenous patient- controlled analgesia (IVPCA group). The maximum pain scores were decreased to a greater extent in the EPCA group on the day of the operation (P < 0.001) and on the first postoperative day (P = 0.001) when compared to the IVPCA group. The patients in the EPCA group also required less analgesics on the day of the operation (P = 0.033) than those in the IVPCA group. The effect of EPCA on complications within the first 30 postoperative days, 24-month postoperative morbidity, cancer recurrence, and mortality were negligible in our study.
CONCLUSIONS
EPCA provided more effective pain control than IVPCA in elderly patients who had undergone elective gastric cancer surgery, but did not affect postoperative outcomes.
MeSH Terms
Figure
Reference
-
1. Bentrem DJ, Cohen ME, Hynes DM, Ko CY, Bilimoria KY. Identification of specific quality improvement opportunities for the elderly undergoing gastrointestinal surgery. Arch Surg. 2009; 144:1013–20. DOI: 10.1001/archsurg.2009.114. PMID: 19917937.2. Park WY, Thompson JS, Lee KK. Effect of epidural anesthesia and analgesia on perioperative outcome:a randomized, controlled Veterans Affairs cooperative study. Ann Surg. 2001; 234:560–9. DOI: 10.1097/00000658-200110000-00015. PMID: 11573049.3. Rodgers A, Walker N, Schug S, McKee A, Kehlet H, van Zundert A, et al. Reduction of postoperative mortality and morbidity with epidural or spinal anaesthesia:results from overview of randomised trials. BMJ. 2000; 321:1493. DOI: 10.1136/bmj.321.7275.1493. PMID: 11118174. PMCID: PMC27550.4. Gottschalk A, Ford JG, Regelin CC, You J, Mascha EJ, Sessler DI, et al. Association between epidural analgesia and cancer recurrence after colorectal cancer surgery. Anesthesiology. 2010; 113:27–34. DOI: 10.1097/ALN.0b013e3181de6d0d. PMID: 20508494.5. Cata JP, Chavez-MacGregor M, Valero V, Black W, Black DM, Goravanchi F, et al. Impact of paravertebral block analgesia on breast cancer survival after surgery. Reg Anesth Pain Med. 2016; 41:696–703. DOI: 10.1097/AAP.0000000000000479. PMID: 27685344.6. Rigg JR, Jamrozik K, Myles PS, Silbert BS, Peyton PJ, Parsons RW, et al. Epidural anaesthesia and analgesia and outcome of major surgery:a randomised trial. Lancet. 2002; 359:1276–82. DOI: 10.1016/S0140-6736(02)08266-1.7. American Thoracic Society;Infectious Diseases Society of America. Guidelines for the management of adults with hospital-acquired, ventilator-associated, and healthcare-associated pneumonia. Am J Respir Crit Care Med. 2005; 171:388–416. DOI: 10.1164/rccm.200405-644ST. PMID: 15699079.8. Huang DD, Zhuang CL, Wang SL, Pang WY, Lou N, Zhou CJ, et al. Prediction of prolonged postoperative ileus after radical gastrectomy for gastric cancer:a scoring system obtained from a prospective study. Medicine (Baltimore). 2015; 94:e2242. DOI: 10.1097/MD.0000000000002242. PMID: 26705206. PMCID: PMC4697972.9. Marret E, Remy C, Bonnet F. Meta-analysis of epidural analgesia versus parenteral opioid analgesia after colorectal surgery. Br J Surg. 2007; 94:665–73. DOI: 10.1002/bjs.5825. PMID: 17514701.10. Liu SS, Wu CL. Effect of postoperative analgesia on major postoperative complications:a systematic update of the evidence. Anesth Analg. 2007; 104:689–702. DOI: 10.1213/01.ane.0000255040.71600.41. PMID: 17312231.11. Shin HS, Oh SJ, Suh BJ. Factors related to morbidity in elderly gastric cancer patients undergoing gastrectomies. J Gastric Cancer. 2014; 14:173–9. DOI: 10.5230/jgc.2014.14.3.173. PMID: 25328762. PMCID: PMC4199884.12. Jørgensen H, Wetterslev J, Møiniche S, Dahl JB. Epidural local anaesthetics versus opioid-based analgesic regimens on postoperative gastrointestinal paralysis, PONV and pain after abdominal surgery. Cochrane Database Syst Rev. 2000; (4):CD001893. PMID: 11034732.13. Kooij FO, Schlack WS, Preckel B, Hollmann MW. Does regional analgesia for major surgery improve outcome? Focus on epidural analgesia. Anesth Analg. 2014; 119:740–4. DOI: 10.1213/ANE.0000000000000245. PMID: 25137006.14. Kampe S, Weinreich G, Darr C, Eicker K, Stamatis G, Hachenberg T. The impact of epidural analgesia compared to systemic opioid-based analgesia with regard to length of hospital stay and recovery of bowel function:retrospective evaluation of 1555 patients undergoing thoracotomy. J Cardiothorac Surg. 2014; 9:175. DOI: 10.1186/s13019-014-0175-8. PMID: 25417134. PMCID: PMC4246432.15. Gibson SJ, Helme RD. Age-related differences in pain perception and report. Clin Geriatr Med. 2001; 17:433–56. DOI: 10.1016/S0749-0690(05)70079-3.16. Huang HW, Wang WC, Lin CC. Influence of age on thermal thresholds, thermal pain thresholds, and reaction time. J Clin Neurosci. 2010; 17:722–6. DOI: 10.1016/j.jocn.2009.10.003. PMID: 20356747.17. Revie EJ, Massie LJ, McNally SJ, McKeown DW, Garden OJ, Wigmore SJ. Effectiveness of epidural analgesia following open liver resection. HPB (Oxford). 2011; 13:206–11. DOI: 10.1111/j.1477-2574.2010.00274.x. PMID: 21309939. PMCID: PMC3048973.18. Kim SH, Shin YS, Oh YJ, Park IH, Choi YS. Postoperative patient controlled analgesia in elderly Koreans:epidural versus intravenous administration. Korean J Anesthesiol. 2013; 65:365–7. DOI: 10.4097/kjae.2013.65.4.365. PMID: 24228157. PMCID: PMC3822036.19. Nam K, Seo JH, Bahk JH. Unsuspected intravascular migration of a thoracic epidural catheter in a thoracotomy patient:A case report. Anesth Pain Med. 2013; 8:184–6.20. Ready LB. Acute pain:lessons learned from 25,000 patients. Reg Anesth Pain Med. 1999; 24:499–505. DOI: 10.1097/00115550-199924060-00004.21. McLeod G, Davies H, Munnoch N, Bannister J, MacRae W. Postoperative pain relief using thoracic epidural analgesia:outstanding success and disappointing failures. Anaesthesia. 2001; 56:75–81. DOI: 10.1046/j.1365-2044.2001.01763-7.x. PMID: 11167441.22. Kamiński JP, Pai A, Ailabouni L, Park JJ, Marecik SJ, Prasad LM, et al. Role of epidural and patient-controlled analgesia in site-specific laparoscopic colorectal surgery. JSLS. 2014; 18:e2014.00207.23. Loran DB, Hyde BR, Zwischenberger JB. Perioperative management of special populations:the geriatric patient. Surg Clin North Am. 2005; 85:1259–66. DOI: 10.1016/j.suc.2005.09.004. PMID: 16326206.24. Brown CH 4th, LaFlam A, Max L, Wyrobek J, Neufeld KJ, Kebaish KM, et al. Delirium after spine surgery in older adults:incidence, risk factors, and outcomes. J Am Geriatr Soc. 2016; 64:2101–8. DOI: 10.1111/jgs.14434. PMID: 27696373. PMCID: PMC5407286.25. Exadaktylos AK, Buggy DJ, Moriarty DC, Mascha E, Sessler DI. Can anesthetic technique for primary breast cancer surgery affect recurrence or metastasis? Anesthesiology. 2006; 105:660–4. DOI: 10.1097/00000542-200610000-00008. PMID: 17006061. PMCID: PMC1615712.26. Cummings KC 3rd, Xu F, Cummings LC, Cooper GS. A comparison of epidural analgesia and traditional pain management effects on survival and cancer recurrence after colectomy:a population-based study. Anesthesiology. 2012; 116:797–806. DOI: 10.1097/ALN.0b013e31824674f6. PMID: 22273991.27. Myles PS, Peyton P, Silbert B, Hunt J, Rigg JR, Sessler DI. Perioperative epidural analgesia for major abdominal surgery for cancer and recurrence-free survival:randomised trial. BMJ. 2011; 342:d1491. DOI: 10.1136/bmj.d1491. PMID: 21447587.28. Sadurní M, Beltrán de Heredia S, Dürsteler C, Pérez-Ramos A, Langohr K, Escolano F, et al. Epidural vs. intravenous fentanyl during colorectal surgery using a double-blind, double-dummy design. Acta Anaesthesiol Scand. 2013; 57:1103–10. DOI: 10.1111/aas.12118. PMID: 23560884.29. Privado MS, Issy AM, Lanchote VL, Garcia JB, Sakata RK. Epidural versus intravenous fentanyl for postoperative analgesia following orthopedic surgery:randomized controlled trial. Sao Paulo Med J. 2010; 128:5–9. DOI: 10.1590/S1516-31802010000100002. PMID: 20512273.30. Christopherson R, James KE, Tableman M, Marshall P, Johnson FE. Long-term survival after colon cancer surgery:a variation associated with choice of anesthesia. Anesth Analg. 2008; 107:325–32. DOI: 10.1213/ane.0b013e3181770f55. PMID: 18635504.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Comparison of Postoperative Analgesia and Side Effects by Patient-Controlled Epidural and Intravenous Analgesia after Cesarean Section
- Can Different Analgesic Methods Affect Open Thoracotomy Outcomes?
- Optimal Concentration of Sufentanil for Patient Controlled Epidural Analgesia in Gastrectomy
- Efficacy of Intrathecal Morphine Combined with Intravenous Analgesia versus Thoracic Epidural Analgesia after Gastrectomy
- Comparison of Continuous Epidural Analgesia with Fentanyl-Bupivacaine Versus Intravenous Patient-Controlled Analgesia with Morphine for Postoperative Pain Control