Yonsei Med J.
2014 Jul;55(4):1106-1114. 10.3349/ymj.2014.55.4.1106.
Efficacy of Intrathecal Morphine Combined with Intravenous Analgesia versus Thoracic Epidural Analgesia after Gastrectomy
- Affiliations
-
- 1Department of Anesthesiology and Pain Medicine, Severance Hospital, Anesthesia and Pain Research Institute, Yonsei University College of Medicine, Seoul, Korea. koobn@yuhs.ac
- 2Department of Surgery, Severance Hospital, Yonsei University College of Medicine, Seoul, Korea.
- KMID: 2130840
- DOI: http://doi.org/10.3349/ymj.2014.55.4.1106
Abstract
- PURPOSE
Epidural analgesia has been the preferred analgesic technique after major abdominal surgery. On the other hand, the combined use of intrathecal morphine (ITM) and intravenous patient controlled analgesia (IVPCA) has been shown to be a viable alternative approach for analgesia. We hypothesized that ITM combined with IVPCA is as effective as patient controlled thoracic epidural analgesia (PCTEA) with respect to postoperative pain control after conventional open gastrectomy.
MATERIALS AND METHODS
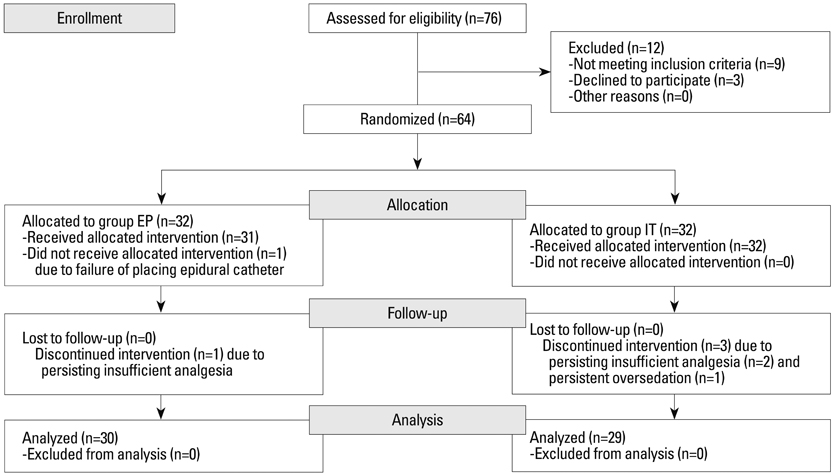
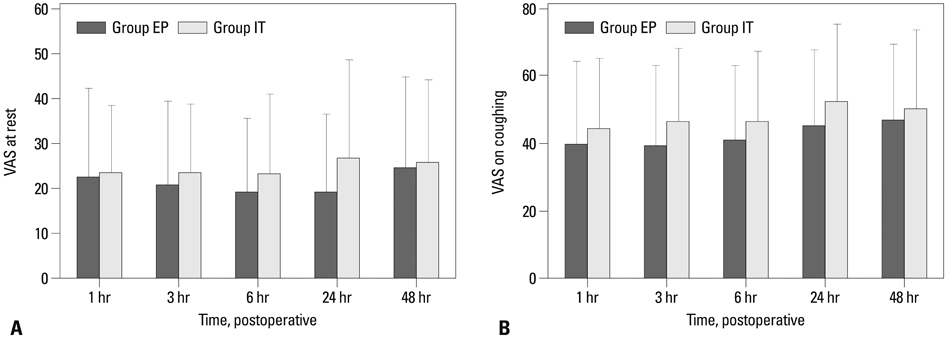
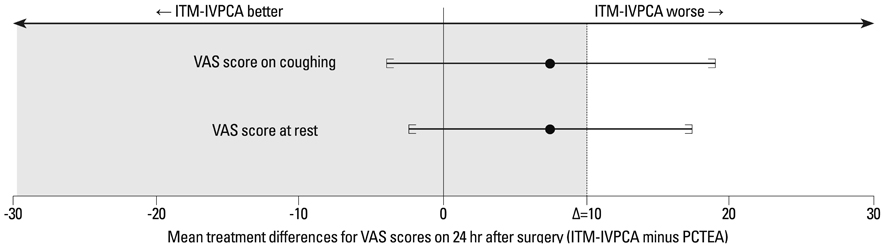
Sixty-four patients undergoing conventional open gastrectomy due to gastric cancer were randomly allocated into the intrathecal morphine combined with intravenous patient-controlled analgesia (IT) group or patient-controlled thoracic epidural analgesia (EP) group. The IT group received preoperative 0.3 mg of ITM, followed by postoperative IVPCA. The EP group preoperatively underwent epidural catheterization, followed by postoperative PCTEA. Visual analog scale (VAS) scores were assessed until 48 hrs after surgery. Adverse effects related to analgesia, profiles associated with recovery from surgery, and postoperative complications within 30 days after surgery were also evaluated.
RESULTS
This study failed to demonstrate the non-inferiority of ITM-IVPCA (n=29) to PCTEA (n=30) with respect to VAS 24 hrs after surgery. Furthermore, the IT group consumed more fentanyl than the EP group did (1247.2+/-263.7 microg vs. 1048.9+/-71.7 microg, p<0.001). The IT group took a longer time to ambulate than the EP group (p=0.021) and had higher incidences of postoperative ileus (p=0.012) and pulmonary complications (p=0.05) compared with the EP group.
CONCLUSION
ITM-IVPCA is not as effective as PCTEA in patients undergoing gastrectomy, with respect to pain control, ambulation, postoperative ileus and pulmonary complications.
Keyword
MeSH Terms
-
Adult
Analgesia, Epidural/*methods
Analgesia, Patient-Controlled/methods
Analgesics, Opioid/administration & dosage/therapeutic use
Female
Gastrectomy/*methods
Humans
Male
Middle Aged
Morphine/*administration & dosage/*therapeutic use
Pain Management/methods
Pain, Postoperative/*drug therapy
Analgesics, Opioid
Morphine
Figure
Reference
-
1. Devys JM, Mora A, Plaud B, Jayr C, Laplanche A, Raynard B, et al. Intrathecal + PCA morphine improves analgesia during the first 24 hr after major abdominal surgery compared to PCA alone. Can J Anaesth. 2003; 50:355–361.
Article2. Beaussier M, Weickmans H, Parc Y, Delpierre E, Camus Y, Funck-Brentano C, et al. Postoperative analgesia and recovery course after major colorectal surgery in elderly patients: a randomized comparison between intrathecal morphine and intravenous PCA morphine. Reg Anesth Pain Med. 2006; 31:531–538.
Article3. Sakowska M, Docherty E, Linscott D, Connor S. A change in practice from epidural to intrathecal morphine analgesia for hepato-pancreato-biliary surgery. World J Surg. 2009; 33:1802–1808.
Article4. Virlos I, Clements D, Beynon J, Ratnalikar V, Khot U. Short-term outcomes with intrathecal versus epidural analgesia in laparoscopic colorectal surgery. Br J Surg. 2010; 97:1401–1406.
Article5. Levy BF, Scott MJ, Fawcett W, Fry C, Rockall TA. Randomized clinical trial of epidural, spinal or patient-controlled analgesia for patients undergoing laparoscopic colorectal surgery. Br J Surg. 2011; 98:1068–1078.
Article6. Werawatganon T, Charuluxananan S. WITHDRAWN: Patient controlled intravenous opioid analgesia versus continuous epidural analgesia for pain after intra-abdominal surgery. Cochrane Database Syst Rev. 2013; 3:CD004088.7. Rodgers A, Walker N, Schug S, McKee A, Kehlet H, van Zundert A, et al. Reduction of postoperative mortality and morbidity with epidural or spinal anaesthesia: results from overview of randomised trials. BMJ. 2000; 321:1493.
Article8. Rigg JR, Jamrozik K, Myles PS, Silbert BS, Peyton PJ, Parsons RW, et al. Epidural anaesthesia and analgesia and outcome of major surgery: a randomised trial. Lancet. 2002; 359:1276–1282.
Article9. Manion SC, Brennan TJ. Thoracic epidural analgesia and acute pain management. Anesthesiology. 2011; 115:181–188.
Article10. Moen V, Dahlgren N, Irestedt L. Severe neurological complications after central neuraxial blockades in Sweden 1990-1999. Anesthesiology. 2004; 101:950–959.
Article11. Oh SJ, Choi WB, Song J, Hyung WJ, Choi SH, Noh SH, et al. Complications requiring reoperation after gastrectomy for gastric cancer: 17 years experience in a single institute. J Gastrointest Surg. 2009; 13:239–245.
Article12. Powell CV, Kelly AM, Williams A. Determining the minimum clinically significant difference in visual analog pain score for children. Ann Emerg Med. 2001; 37:28–31.
Article13. Bodian CA, Freedman G, Hossain S, Eisenkraft JB, Beilin Y. The visual analog scale for pain: clinical significance in postoperative patients. Anesthesiology. 2001; 95:1356–1361.14. Komatsu H, Matsumoto S, Mitsuhata H, Abe K, Toriyabe S. Comparison of patient-controlled epidural analgesia with and without background infusion after gastrectomy. Anesth Analg. 1998; 87:907–910.
Article15. Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987; 40:373–383.
Article16. Meylan N, Elia N, Lysakowski C, Tramèr MR. Benefit and risk of intrathecal morphine without local anaesthetic in patients undergoing major surgery: meta-analysis of randomized trials. Br J Anaesth. 2009; 102:156–167.
Article17. De Pietri L, Siniscalchi A, Reggiani A, Masetti M, Begliomini B, Gazzi M, et al. The use of intrathecal morphine for postoperative pain relief after liver resection: a comparison with epidural analgesia. Anesth Analg. 2006; 102:1157–1163.
Article18. Zhu Z, Wang C, Xu C, Cai Q. Influence of patient-controlled epidural analgesia versus patient-controlled intravenous analgesia on postoperative pain control and recovery after gastrectomy for gastric cancer: a prospective randomized trial. Gastric Cancer. 2013; 16:193–200.
Article19. Boonmak S, Boonmak P, Bunsaengjaroen P, Srichaipanha S, Thincheelong V. Comparison of intrathecal morphine plus PCA and PCA alone for post-operative analgesia after kidney surgery. J Med Assoc Thai. 2007; 90:1143–1149.20. Kehlet H, Holte K. Review of postoperative ileus. Am J Surg. 2001; 182:5A Suppl. 3S–10S.
Article21. Holte K, Kehlet H. Epidural analgesia and risk of anastomotic leakage. Reg Anesth Pain Med. 2001; 26:111–117.
Article22. van Lier F, van der Geest PJ, Hoeks SE, van Gestel YR, Hol JW, Sin DD, et al. Epidural analgesia is associated with improved health outcomes of surgical patients with chronic obstructive pulmonary disease. Anesthesiology. 2011; 115:315–321.
Article23. Meierhenrich R, Hock D, Kühn S, Baltes E, Muehling B, Muche R, et al. Analgesia and pulmonary function after lung surgery: is a single intercostal nerve block plus patient-controlled intravenous morphine as effective as patient-controlled epidural anaesthesia? A randomized non-inferiority clinical trial. Br J Anaesth. 2011; 106:580–589.
Article24. Bauer C, Hentz JG, Ducrocq X, Meyer N, Oswald-Mammosser M, Steib A, et al. Lung function after lobectomy: a randomized, double-blinded trial comparing thoracic epidural ropivacaine/sufentanil and intravenous morphine for patient-controlled analgesia. Anesth Analg. 2007; 105:238–244.
Article25. Holte K, Sharrock NE, Kehlet H. Pathophysiology and clinical implications of perioperative fluid excess. Br J Anaesth. 2002; 89:622–632.
Article26. Olsén MF, Wennberg E. Fast-track concepts in major open upper abdominal and thoracoabdominal surgery: a review. World J Surg. 2011; 35:2586–2593.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Post-thoracotomy Analgesia & ICU Length of Stay: Comparison of Thoracic Epidrual Morphine Infusion and Lumbar Epidural Plus Intravenous Morphine Infusion
- Comparison between Epidural Analgesia and Combined Spinal-Epidural Analgesia for Labor and Delivery
- The Comparison of Epidural Morphine and Epidural Morphine-Ketamine for Postoperative Pain Relief after Subtotal Gastrectomy
- Comparison of Intrathecal Injection with Epidural Injection of Opioids and Local Anesthetics for Labor Analgesia
- Postoperative Analgesic Effect of Combined Low Dose Intrathecal Morphine and Continuous Epidural Opioid Local Anesthetic Mixture after Lumbar Laminectomy