Korean J Radiol.
2018 Apr;19(2):334-341. 10.3348/kjr.2018.19.2.334.
Endovascular Treatment of Bilateral Cavernous Sinus Dural Arteriovenous Fistula: Therapeutic Strategy and Follow-Up Outcomes
- Affiliations
-
- 1Department of Neurosurgery, Jeju National University College of Medicine, Jeju 63241, Korea.
- 2Department of Radiology, Seoul National University Hospital, Seoul National University College of Medicine, Seoul 03080, Korea. aronnn@naver.com
- 3Department of Neurosurgery, Seoul National University Hospital, Seoul National University College of Medicine, Seoul 03080, Korea.
- 4Department of Neurosurgery, Seoul National University Bundang Hospital, Seoul National University College of Medicine, Seongnam 13620, Korea.
- KMID: 2404931
- DOI: http://doi.org/10.3348/kjr.2018.19.2.334
Abstract
OBJECTIVE
Bilateral cavernous sinus dural arteriovenous fistula (CSdAVF) is very rare, even in Asian countries. The research intended to present clinical and radiologic outcomes of treating such fistulas through endovascular embolization.
MATERIALS AND METHODS
Data was obtained from 220 consecutive patients, with CSdAVF, who were treated from January 2004 to December 2015. Bilateral CSdAVF was identified in 17 patients (7.7%). The clinical and radiologic outcomes of the fistulas were assessed with an emphasis on the technical aspects of treatment.
RESULTS
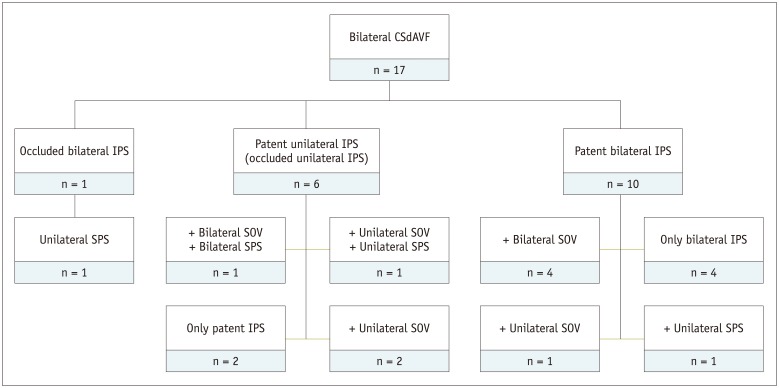
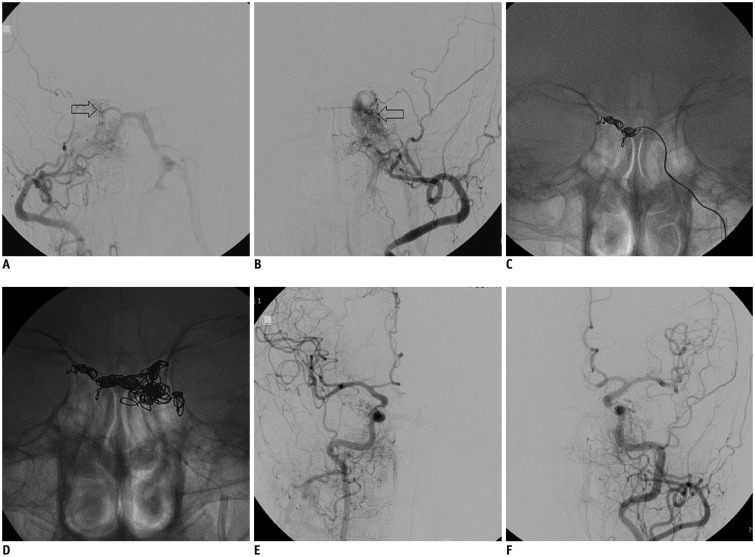
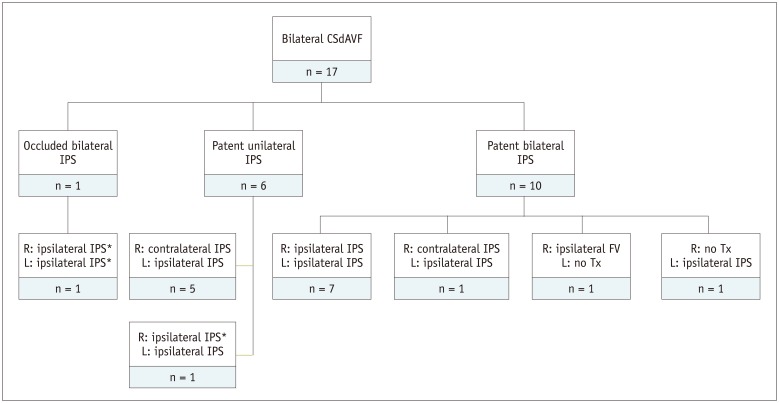
At the time of treatment, 7 and 10 patients presented with bilateral and unilateral symptoms, respectively. In the former cases, 4 patients had progressed from unilateral to bilateral symptoms. Bilateral fistulas were treated with a single-stage transvenous embolization (TVE) in 15 patients, via bilateral inferior petrosal sinuses (IPS) (n = 9) and unilateral IPS (n = 6). In the other 2 patients with one-sided dominance of shunting, only dominant fistula was treated. Two untreated lesions were found on follow-up to have spontaneously resolved after treatment of the dominant contralateral fistula. Of the 34 CSdAVF lesions, complete occlusion was achieved in 32 lesions after TVE. Seven patients (41.2%) developed worsening of cranial nerve palsy after TVE. During the follow-up period, 4 patients obtained complete recovery, whereas the other 3 remained with deficits.
CONCLUSION
With adjustments of endovascular procedures to accommodate distinct anatomical configurations, endovascular treatment for bilateral CSdAVF can achieve excellent angiographic occlusion results. However, aggravation of symptoms after TVE may occur frequently in bilateral CSdAVF. In the patients with one-sided dominance of shunt, treatment of only dominant fistula might be an alternative option.
Keyword
MeSH Terms
Figure
Cited by 2 articles
-
Coil-Protected Technique for Liquid Embolization in Neurovascular Malformations
Keun Young Park, Jin Woo Kim, Byung Moon Kim, Dong Joon Kim, Joonho Chung, Chang Ki Jang, Jun-Hwee Kim
Korean J Radiol. 2019;20(8):1285-1292. doi: 10.3348/kjr.2019.0127.Role of surgery in management of intracranial dural arteriovenous fistulas
Young Sill Kang, Won-Sang Cho, Sung Ho Lee, Kangmin Kim, Hyun-Seung Kang, Jeong Eun Kim
J Cerebrovasc Endovasc Neurosurg. 2023;25(2):117-131. doi: 10.7461/jcen.2023.E2022.10.006.
Reference
-
1. Cawley CM, Barrow DL, Dion JE. Treatment of lateral-sigmoid and sagittal sinus dural arteriovenous malformations. In : Winn HR, Youmans JR, editors. Youmans neurological surgery Volume 2. 5th ed. Philadelphia, PA: WB Saunders;2004. p. 2283–2291.2. Collice M, D'Aliberti G, Talamonti G, Branca V, Boccardi E, Scialfa G, et al. Surgical interruption of leptomeningeal drainage as treatment for intracranial dural arteriovenous fistulas without dural sinus drainage. J Neurosurg. 1996; 84:810–817. PMID: 8622155.
Article3. Hwang H, La YK, Baek MS, Baik K, Suh SH, Kim WJ. Dural arteriovenous fistula manifested as rapid progressive dementia successfully treated by endovascular embolization only. Neurointervention. 2017; 12:50–53. PMID: 28316870.
Article4. Barnwell SL, Halbach VV, Dowd CF, Higashida RT, Hieshima GB, Wilson CB. A variant of arteriovenous fistulas within the wall of dural sinuses. Results of combined surgical and endovascular therapy. J Neurosurg. 1991; 74:199–204. PMID: 1988588.
Article5. Kikuchi K, Kowada M. Anterior fossa dural arteriovenous malformation supplied by bilateral ethmoidal arteries. Surg Neurol. 1994; 41:56–64. PMID: 8310389.
Article6. Cho YD, Rhim JK, Yoo DH, Kang HS, Kim JE, Cho WS, et al. Transvenous microguidewire looping technique for breach of ipsilateral inferior petrosal sinus occlusions en route to cavernous sinus dural arteriovenous fistulas. Interv Neuroradiol. 2016; 22:590–595. PMID: 27298011.
Article7. Rhim JK, Cho YD, Park JJ, Jeon JP, Kang HS, Kim JE, et al. Endovascular treatment of cavernous sinus dural arteriovenous fistula with ipsilateral inferior petrosal sinus occlusion: a single-center experience. Neurosurgery. 2015; 77:192–199. discussion 199. PMID: 25830601.8. Suh DC, Lee JH, Kim SJ, Chung SJ, Choi CG, Kim HJ, et al. New concept in cavernous sinus dural arteriovenous fistula: correlation with presenting symptom and venous drainage patterns. Stroke. 2005; 36:1134–1139. PMID: 15890994.9. Cognard C, Gobin YP, Pierot L, Bailly AL, Houdart E, Casasco A, et al. Cerebral dural arteriovenous fistulas: clinical and angiographic correlation with a revised classification of venous drainage. Radiology. 1995; 194:671–680. PMID: 7862961.
Article10. Newton TH, Cronqvist S. Involvement of dural arteries in intracranial arteriovenous malformations. Radiology. 1969; 93:1071–1078. PMID: 5350675.
Article11. van Dijk JM, TerBrugge KG, Willinsky RA, Wallace MC. Multiplicity of dural arteriovenous fistulas. J Neurosurg. 2002; 96:76–78. PMID: 11795255.
Article12. Dabus G, Batjer HH, Hurley MC, Nimmagadda A, Russell EJ. Endovascular treatment of a bilateral dural carotid-cavernous fistula using an unusual unilateral approach through the basilar plexus. World Neurosurg. 2012; 77:201.e5–201.e8.
Article13. Chaloupka JC, Goller D, Goldberg RA, Duckwiler GR, Martin NA, Viñuela F. True anatomical compartmentalization of the cavernous sinus in a patient with bilateral cavernous dural arteriovenous fistulae. Case report. J Neurosurg. 1993; 79:592–595. PMID: 8410230.14. Courtheoux P, Labbe D, Hamel C, Lecoq PJ, Jahara M, Théron J. Treatment of bilateral spontaneous dural carotid-cavernous fistulas by coils and sclerotherapy. Case report. J Neurosurg. 1987; 66:468–470. PMID: 3819844.15. Diez Lobato R, Escudero L, Lamas E. Bilateral dural arteriovenous fistula in the region of the cavernous sinus. Neuroradiology. 1978; 15:39–43. PMID: 643172.
Article16. Hacein-Bey L, Konstas AA, Pile-Spellman J. Natural history, current concepts, classification, factors impacting endovascular therapy, and pathophysiology of cerebral and spinal dural arteriovenous fistulas. Clin Neurol Neurosurg. 2014; 121:64–75. PMID: 24636717.
Article17. Chung SJ, Kim JS, Kim JC, Lee SK, Kwon SU, Lee MC, et al. Intracranial dural arteriovenous fistulas: analysis of 60 patients. Cerebrovasc Dis. 2002; 13:79–88. PMID: 11867880.
Article18. Kojima T, Miyachi S, Sahara Y, Nakai K, Okamoto T, Hattori K, et al. The relationship between venous hypertension and expression of vascular endothelial growth factor: hemodynamic and immunohistochemical examinations in a rat venous hypertension model. Surg Neurol. 2007; 68:277–284. discussion 284. PMID: 17719966.
Article19. Ha SY, Kwon YS, Kim BM, Kim DI, Kim DJ. Clinical and angiographic characteristics of multiple dural arteriovenous shunts. AJNR Am J Neuroradiol. 2012; 33:1691–1695. PMID: 22538077.
Article20. Barrow DL, Spector RH, Braun IF, Landman JA, Tindall SC, Tindall GT. Classification and treatment of spontaneous carotid-cavernous sinus fistulas. J Neurosurg. 1985; 62:248–256. PMID: 3968564.
Article21. Viñuela F, Fox AJ, Debrun GM, Peerless SJ, Drake CG. Spontaneous carotid-cavernous fistulas: clinical, radiological, and therapeutic considerations. Experience with 20 cases. J Neurosurg. 1984; 60:976–984. PMID: 6716167.22. Benndorf G, Bender A, Lehmann R, Lanksch W. Transvenous occlusion of dural cavernous sinus fistulas through the thrombosed inferior petrosal sinus: report of four cases and review of the literature. Surg Neurol. 2000; 54:42–54. PMID: 11024506.
Article23. Jung KH, Kwon BJ, Chu K, Noh Y, Lee ST, Cho YD, et al. Clinical and angiographic factors related to the prognosis of cavernous sinus dural arteriovenous fistula. Neuroradiology. 2011; 53:983–992. PMID: 21161199.
Article24. Kim DJ, Kim DI, Suh SH, Kim J, Lee SK, Kim EY, et al. Results of transvenous embolization of cavernous dural arteriovenous fistula: a single-center experience with emphasis on complications and management. AJNR Am J Neuroradiol. 2006; 27:2078–2082. PMID: 17110671.25. Lewis AI, Tomsick TA, Tew JM Jr. Management of 100 consecutive direct carotid-cavernous fistulas: results of treatment with detachable balloons. Neurosurgery. 1995; 36:239–244. discussion 244-245. PMID: 7731502.26. Debrun G, Lacour P, Vinuela F, Fox A, Drake CG, Caron JP. Treatment of 54 traumatic carotid-cavernous fistulas. J Neurosurg. 1981; 55:678–692. PMID: 6458669.
Article27. Sergott RC, Grossman RI, Savino PJ, Bosley TM, Schatz NJ. The syndrome of paradoxical worsening of dural-cavernous sinus arteriovenous malformations. Ophthalmology. 1987; 94:205–212. PMID: 3587894.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Endovascular management of cavernous sinus dural arteriovenous fistulas: Overall review and considerations
- Transvenous Embolization of Cavernous Sinus Dural Arteriovenous Fistula Using the Direct Superior Ophthalmic Vein Approach: A Case Report
- Endovascular Treatment of Cavernous Sinus Dural Arteriovenous Fistula via Radial Artery and Median Cubital Vein
- Cranial Nerve Palsy in Patients with Cavernous Sinus Dural Arteriovenous Fistula Treated with Embolization: A Single Institution Retrospective Analysis
- A Case of Dural Carotid-Cavernous Sinus Fistula Associated with Ophthalmic Manifestations