Nationwide Statistical Analysis of Lymphoid Malignancies in Korea
- Affiliations
-
- 1Center for Hematologic Malignancy, Research Institute and Hospital, National Cancer Center, Goyang, Korea. hseom@ncc.re.kr
- 2Center for Pediatric Oncology, Research Institute and Hospital, National Cancer Center, Goyang, Korea.
- 3Cancer Registration and Statistics Branch, National Cancer Center, Goyang, Korea. astra67@ncc.re.kr
- 4Department of System Cancer Science Graduate School of Cancer Science and Policy, National Cancer Center, Goyang, Korea.
- 5Department of Cancer Control and Policy, Graduate School of Cancer Science and Policy, National Cancer Center, Goyang, Korea.
- KMID: 2403492
- DOI: http://doi.org/10.4143/crt.2017.093
Abstract
- PURPOSE
Regional differences in the incidence of lymphoid malignancies have been reported worldwide, but there has been no large-scale epidemiologic analysis in Korea. The aim of this study was to provide a nationwide population-based statistical analysis of Korean patients with lymphoid malignancies.
MATERIALS AND METHODS
The Korea Central Cancer Registry analyzed the incidence and survival of patients with lymphoid malignancies from the Korean National Cancer Incidence Database. Diseases were grouped by clinically relevant categories based on the 2008 World Health Organization classification.
RESULTS
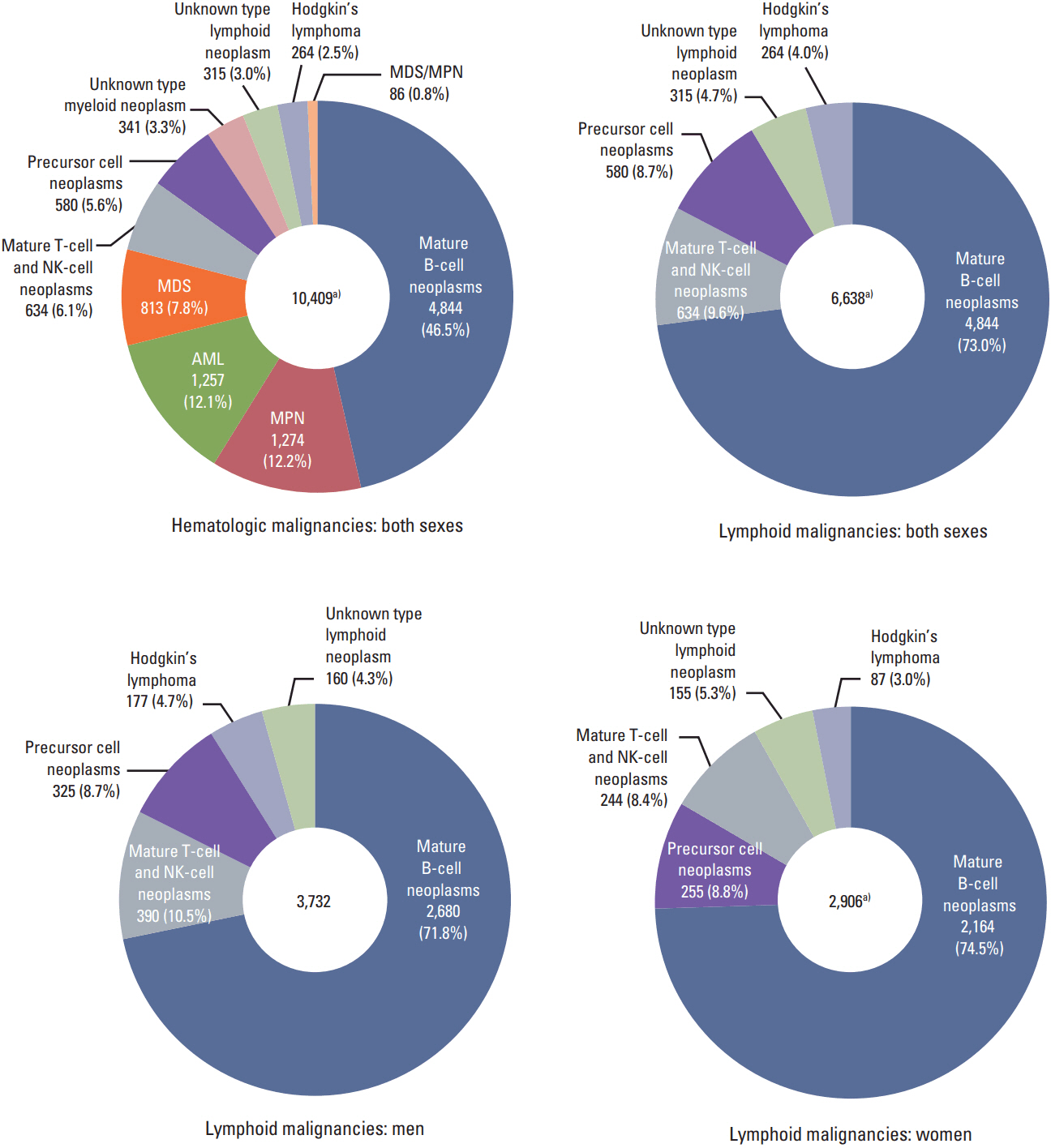
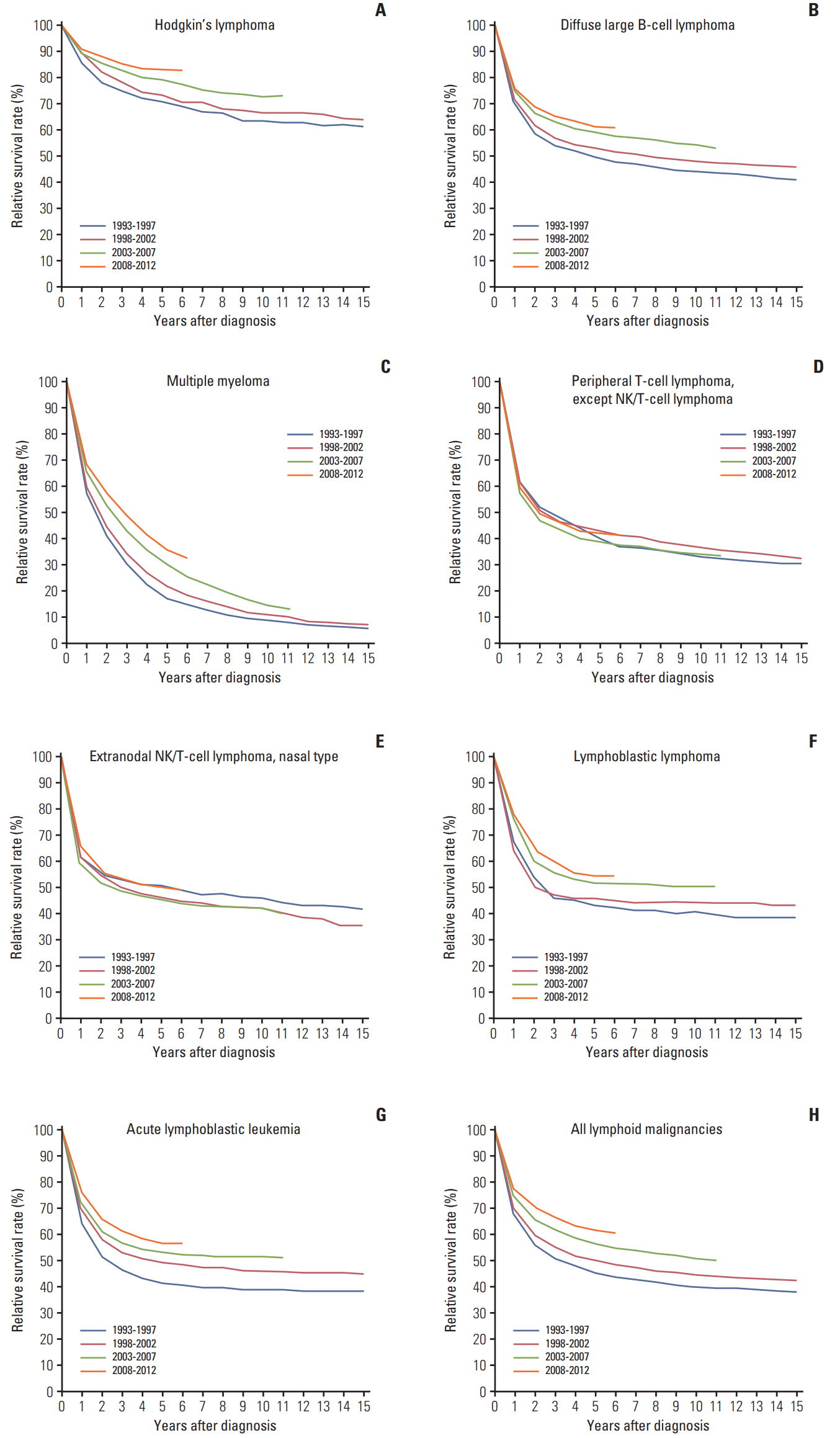
Overall 65,948 lymphoid diseases were identified between 1999 and 2012. The incidence of most subtypes increased with age, except for precursor cell neoplasms. Male predominance (male:female ratio=1.28:1) was observed. In 2012, annual age-standardized incidence rates per 100,000 persons of Hodgkin's lymphoma, mature B-cell neoplasm, mature T/natural killer (NK)-cell neoplasm, and precursor cell neoplasm were 0.46, 6.60, 0.95, and 1.50, respectively, and they increased yearly from 1999. Composite Hodgkin's and non-Hodgkin's lymphomas were extremely rare. Survival improvement estimated using 5-year relative survival rate was observed in patients with Hodgkin's lymphoma (71.1%-83.0%), diffuse large B-cell lymphoma (49.5%-61.5%), plasma cell neoplasms (20.2%-36.9%), and lymphoblastic lymphoma/leukemia (41.5%-56.3%) between 1993 and 2012. However, survival rates of T/NK-cell lymphoma (excluding cutaneous T-cell lymphoma) ranged from 40.5%-43.5% during the study period. Survival rates decreased with age in most subtypes.
CONCLUSION
This report presented the subtype-specific statistical analysis of lymphoid malignancies in the Korean population, showing increasing incidences and survival rates in most subtypes.
MeSH Terms
Figure
Cited by 10 articles
-
국내 혈액암 질환의 증가 양상: 2005년부터 2015년까지 국민건강보험 빅데이터에 근거하여
Yujin Han, Young Jin Kim, Min Jin Kim, Ja Min Byun, Taemi Youk, Hoi Soo Yoon, Jae Hee Lee, Woo-In Lee, Tae Sung Park, Jongha Yoo
Lab Med Online. 2020;10(2):144-151. doi: 10.3343/lmo.2020.10.2.144.Recent advances in chronic lymphocytic leukemia therapy
Jieun Uhm
Blood Res. 2020;55(Supplement):S72-S82. doi: 10.5045/br.2020.S012.Recent advances in chronic lymphocytic leukemia therapy
Jieun Uhm
Blood Res. 2020;55(S1):S72-S82. doi: 10.5045/br.2020.S012.Trends of Incidence and Survival Rates of Mucosa-associated Lymphoid Tissue Lymphoma in the Korean Population: Analysis of the Korea Central Cancer Registry Database
Seok-Hoo Jeong, Shin Young Hyun, Ja Sung Choi, Hee Man Kim
J Korean Med Sci. 2020;35(36):e294. doi: 10.3346/jkms.2020.35.e294.Multicenter retrospective analysis of patients with chronic lymphocytic leukemia in Korea
Jun Ho Yi, Gyeong-Won Lee, Ji Hyun Lee, Kwai Han Yoo, Chul Won Jung, Dae Sik Kim, Jeong-Ok Lee, Hyeon Seok Eom, Ja Min Byun, Youngil Koh, Sung Soo Yoon, Jin Seok Kim, Jee Hyun Kong, Ho-Young Yhim, Deok-Hwan Yang, Dok Hyun Yoon, Do Hyoung Lim, Won-Sik Lee, Ho-Jin Shin
Blood Res. 2021;56(4):243-251. doi: 10.5045/br.2021.2021102.Twenty-year incidence trend of hematologic malignancies in the Republic of Korea: 1999‒2018
Won-Ju Park, Joo-Heon Park, Seunghyeon Cho, Myung Geun Shin
Blood Res. 2021;56(4):301-314. doi: 10.5045/br.2021.2021187.Upward trend in follicular lymphoma among the Korean population: 10-year experience at a large tertiary institution
Meejeong Kim, Hee Sang Hwang, Hyungwoo Cho, Dok Hyun Yoon, Cheolwon Suh, Chan Sik Park, Heounjeong Go, Jooryung Huh
J Pathol Transl Med. 2021;55(5):330-337. doi: 10.4132/jptm.2021.07.25.Increasing Incidence of B-Cell Non-Hodgkin Lymphoma and Occurrence of Second Primary Malignancies in South Korea: 10-Year Follow-up Using the Korean National Health Information Database
Jin Seok Kim, Yanfang Liu, Kyoung Hwa Ha, Hong Qiu, Lee Anne Rothwell, Hyeon Chang Kim
Cancer Res Treat. 2020;52(4):1262-1272. doi: 10.4143/crt.2020.089.Role of Roflumilast Combined with ESHAP Chemotherapy in Relapsed/Refractory Patients with Diffuse Large B-Cell Lymphoma
Do Young Kim, Jehyun Nam, Joo-seop Chung, Sang-Woo Kim, Ho-Jin Shin
Cancer Res Treat. 2022;54(1):301-313. doi: 10.4143/crt.2020.1371.Secondary Malignancies in Multiple Myeloma in Korean Patients: A Nationwide Population-Based Study
Boyoung Park, Eunyoung Lee, Junghyun Yoon, YoungJu Park, Hyeon-Seok Eom
Cancer Res Treat. 2024;56(3):936-944. doi: 10.4143/crt.2023.843.
Reference
-
References
1. Torre LA, Bray F, Siegel RL, Ferlay J, Lortet-Tieulent J, Jemal A. Global cancer statistics, 2012. CA Cancer J Clin. 2015; 65:87–108.
Article2. Swerdlow SH, Campo E, Harris NL, Jaffe ES, Pileri SA, Stein H, et al. WHO classification of tumours of haematopoietic and lymphoid tissues. 4th ed. Lyon: IARC Press;2008.3. Muller AM, Ihorst G, Mertelsmann R, Engelhardt M. Epidemiology of non-Hodgkin's lymphoma (NHL): trends, geographic distribution, and etiology. Ann Hematol. 2005; 84:1–12.
Article4. Rudiger T, Weisenburger DD, Anderson JR, Armitage JO, Diebold J, MacLennan KA, et al. Peripheral T-cell lymphoma (excluding anaplastic large-cell lymphoma): results from the Non-Hodgkin's Lymphoma Classification Project. Ann Oncol. 2002; 13:140–9.5. Ohshima K, Suzumiya J, Kikuchi M. The World Health Organization classification of malignant lymphoma: incidence and clinical prognosis in HTLV-1-endemic area of Fukuoka. Pathol Int. 2002; 52:1–12.
Article6. Harris NL, Jaffe ES, Stein H, Banks PM, Chan JK, Cleary ML, et al. A revised European-American classification of lymphoid neoplasms: a proposal from the International Lymphoma Study Group. Blood. 1994; 84:1361–92.7. Bennett JM, Catovsky D, Daniel MT, Flandrin G, Galton DA, Gralnick HR, et al. Proposals for the classification of chronic (mature) B and T lymphoid leukaemias. French-AmericanBritish (FAB) Cooperative Group. J Clin Pathol. 1989; 42:567–84.
Article8. Bennett JM, Catovsky D, Daniel MT, Flandrin G, Galton DA, Gralnick HR, et al. Proposals for the classification of the acute leukaemias. French-American-British (FAB) co-operative group. Br J Haematol. 1976; 33:451–8.
Article9. Percy C, Fritz A, Jack A, Shanmugarathan S, Sobin L, Parkin DM, et al. International classification of diseases for oncology (ICD-O). 3rd ed. Geneva: World Health Organization;2000.10. Marcos-Gragera R, Allemani C, Tereanu C, De Angelis R, Capocaccia R, Maynadie M, et al. Survival of European patients diagnosed with lymphoid neoplasms in 2000-2002: results of the HAEMACARE project. Haematologica. 2011; 96:720–8.
Article11. Sant M, Allemani C, Tereanu C, De Angelis R, Capocaccia R, Visser O, et al. Incidence of hematologic malignancies in Europe by morphologic subtype: results of the HAEMACARE project. Blood. 2010; 116:3724–34.
Article12. Park HJ, Park EH, Jung KW, Kong HJ, Won YJ, Lee JY, et al. Statistics of hematologic malignancies in Korea: incidence, prevalence and survival rates from 1999 to 2008. Korean J Hematol. 2012; 47:28–38.
Article13. Segi M. Cancer mortality for selected sites in 24 countrues (1950-1957). Sendai: Tohoku University School of Medicine;1960.14. Howlader N, Noone AM, Krapcho M, Miller D, Bishop K, Altekruse SF, et al. SEER Cancer Statistics Review, 1975-2013 [Internet]. Bethesda, MD: National Cancer Institute;2015. [cited 2016 Apr 1]. Available from: http://seer.cancer.gov/csr/1975_2013/.15. Ederer F, Axtell LM, Cutler SJ. The relative survival rate: a statistical methodology. Natl Cancer Inst Monogr. 1961; 6:101–21.16. Dickman PW, Sloggett A, Hills M, Hakulinen T. Regression models for relative survival. Stat Med. 2004; 23:51–64.
Article17. Ederer F, Heise H. Instructions to IBM 650 programmers in processing survival computations. Methodological note No. 10. End results evaluation section. Bethesda, MD: National Cancer Institute;1959.18. Bassig BA, Au WY, Mang O, Ngan R, Morton LM, Ip DK, et al. Subtype-specific incidence rates of lymphoid malignancies in Hong Kong compared to the United States, 2001-2010. Cancer Epidemiol. 2016; 42:15–23.
Article19. Chihara D, Ito H, Matsuda T, Shibata A, Katsumi A, Nakamura S, et al. Differences in incidence and trends of haematological malignancies in Japan and the United States. Br J Haematol. 2014; 164:536–45.20. Jung KW, Won YJ, Kong HJ, Oh CM, Cho H, Lee DH, et al. Cancer statistics in Korea: incidence, mortality, survival, and prevalence in 2012. Cancer Res Treat. 2015; 47:127–41.
Article21. Won YW, Kwon JH, Lee SI, Oh SY, Kim WS, Kim SJ, et al. Clinical features and outcomes of Hodgkin's lymphoma in Korea: Consortium for Improving Survival of Lymphoma (CISL). Ann Hematol. 2012; 91:223–33.
Article22. Jarrett RF, Stark GL, White J, Angus B, Alexander FE, Krajewski AS, et al. Impact of tumor Epstein-Barr virus status on presenting features and outcome in age-defined subgroups of patients with classic Hodgkin lymphoma: a population-based study. Blood. 2005; 106:2444–51.
Article23. Engert A, Ballova V, Haverkamp H, Pfistner B, Josting A, Duhmke E, et al. Hodgkin’s lymphoma in elderly patients: a comprehensive retrospective analysis from the German Hodgkin’s Study Group. J Clin Oncol. 2005; 23:5052–60.
Article24. Flowers CR, Fedewa SA, Chen AY, Nastoupil LJ, Lipscomb J, Brawley OW, et al. Disparities in the early adoption of chemoimmunotherapy for diffuse large B-cell lymphoma in the United States. Cancer Epidemiol Biomarkers Prev. 2012; 21:1520–30.
Article25. Bruce CJ. Rituxan anniversary: 10 years of progress. Oncol Bus Rev. 2007; 18–9.26. Kim SJ, Kim K, Kim BS, Kim CY, Suh C, Huh J, et al. Phase II trial of concurrent radiation and weekly cisplatin followed by VIPD chemotherapy in newly diagnosed, stage IE to IIE, nasal, extranodal NK/T-Cell Lymphoma: Consortium for Improving Survival of Lymphoma study. J Clin Oncol. 2009; 27:6027–32.
Article27. Kwong YL, Kim WS, Lim ST, Kim SJ, Tang T, Tse E, et al. SMILE for natural killer/T-cell lymphoma: analysis of safety and efficacy from the Asia Lymphoma Study Group. Blood. 2012; 120:2973–80.
Article28. Moorman AV, Chilton L, Wilkinson J, Ensor HM, Bown N, Proctor SJ. A population-based cytogenetic study of adults with acute lymphoblastic leukemia. Blood. 2010; 115:206–14.
Article29. Veal GJ, Hartford CM, Stewart CF. Clinical pharmacology in the adolescent oncology patient. J Clin Oncol. 2010; 28:4790–9.
Article30. Bleyer A, Budd T, Montello M. Adolescents and young adults with cancer: the scope of the problem and criticality of clinical trials. Cancer. 2006; 107(7 Suppl):1645–55.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Recent advances in cellular immunotherapy for lymphoid malignancies
- Statistics of hematologic malignancies in Korea: incidence, prevalence and survival rates from 1999 to 2008
- Nationwide statistical analysis of myeloid malignancies in Korea: incidence and survival rate from 1999 to 2012
- Neoplastic Diseases of the Hematopoietic and Lymphoid Tissues: New World Health Organization Classification
- Current Challenges in Chimeric Antigen Receptor T-cell Therapy in Patients With B-cell Lymphoid Malignancies