Epidemiology of Intracranial Metastases in Korea: A National Cohort Investigation
- Affiliations
-
- 1Department of Neurosurgery, Seoul National University Bundang Hospital, Seongnam, Korea. chaeyong@snu.ac.kr
- 2Seoul National University College of Medicine, Seoul, Korea.
- 3Department of Radiation Oncology, Seoul National University Bundang Hospital, Seongnam, Korea.
- 4Division of Hematology and Medical Oncology, Department of Internal Medicine, Seoul National University Bundang Hospital, Seongnam, Korea.
- KMID: 2403486
- DOI: http://doi.org/10.4143/crt.2017.072
Abstract
- PURPOSE
To investigate the epidemiologic features of intracranial metastases (ICMET) in Korea, we performed a cohort study using the National Health Insurance Service-National Sample Cohort database, which comprised healthcare usage information of approximately 1 million Korean individuals over 12 years.
MATERIALS AND METHODS
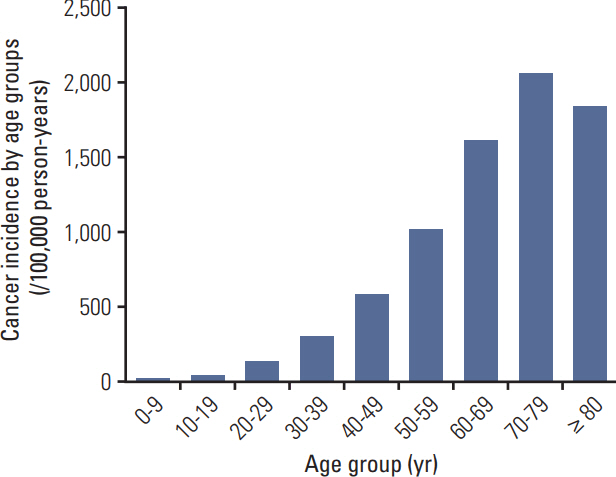
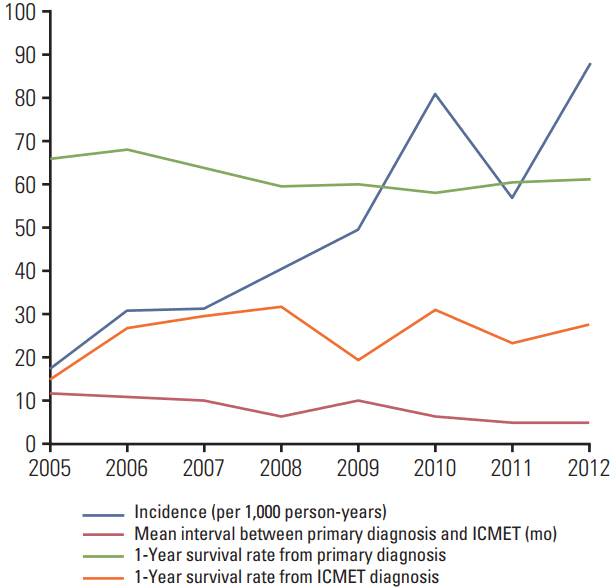
We enrolled 998,602 subjects, after excluding 18,218 subjects diagnosed with any cancer during the washout period (2002-2004). The observation period was 9 years (2005-2013; 8,725,438 person-years). The initial diagnosis date of ICMET and the primary cancer was recorded. The incidence was determined based on the number of incident cases and observation size, whereas survival was estimated using death statistics from the database.
RESULTS
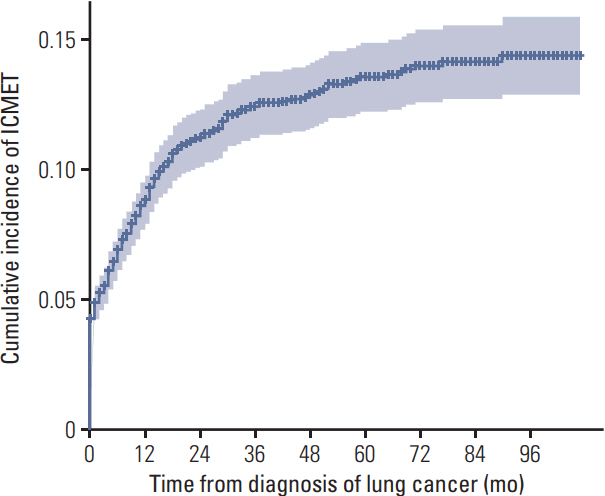
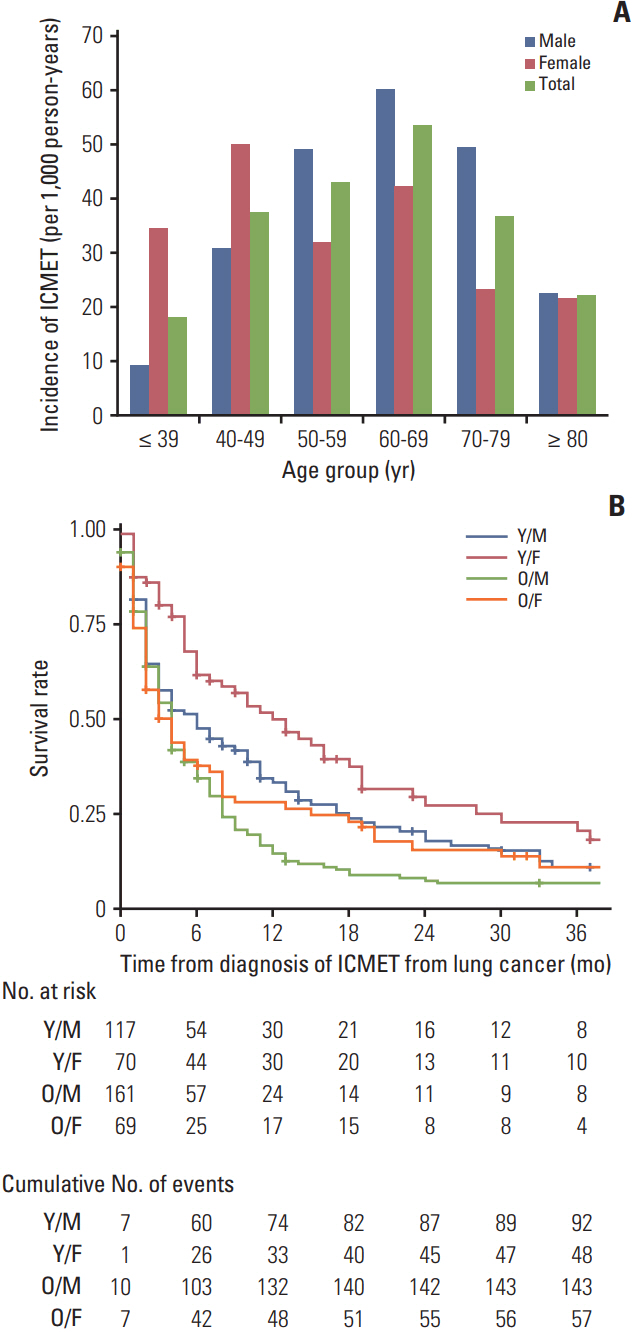
Through observation period, a total 776 subjects developed ICMET. The age-standardized incidence of ICMET was 8.2 per 100,000 person-years. The mean interval between the initial diagnosis date of the primary cancer and ICMET was 13.1 months. Patients with ICMET had shorter survival than those without ICMET (30.9 months vs. 81.4 months, p < 0.001). The ICMET incidence among the cancer patients was 5.0 per 1,000 person-years; it was highest in lung cancer cases, followed by breast and liver cancer cases. Moreover, ICMET from lung cancer was the most common metastasis type, followed by ICMET from liver and breast cancer.
CONCLUSION
The incidence of ICMET was 8.2 per 100,000 person-years among the Korean population and 5.0 per 1,000 person-years among cancer patients. Most of the ICMET cases arose from lung cancer. ICMET also critically influenced survival in cancer patients.
Keyword
MeSH Terms
Figure
Cited by 4 articles
-
Verification of Low Risk for Perihippocampal Recurrence in Patients with Brain Metastases Who Received Whole-Brain Radiotherapy with Hippocampal Avoidance
Youngkyong Kim, Sung Hwan Kim, Jong Hoon Lee, Dae Gyu Kang
Cancer Res Treat. 2019;51(2):568-575. doi: 10.4143/crt.2018.206.Non–coplanar whole brain radiotherapy is an effective modality for parotid sparing
Jaehyeon Park, Jae Won Park, Ji Woon Yea
Yeungnam Univ J Med. 2019;36(1):36-42. doi: 10.12701/yujm.2019.00087.Treatment Outcome of the Brain Metastases in Peri-Rolandic Area: Comparison Between Surgery and Stereotactic Radiosurgery
Jun Hyeok Jung, Kawngwoo Park, Eun Young Kim, Chan-Jong Yoo, Gi-Taek Yee, Woo-Kyung Kim, Dong-Won Shin
Brain Tumor Res Treat. 2023;11(4):246-253. doi: 10.14791/btrt.2023.0032.Dural Metastasis in Breast Cancer: MRI-Based Morphological Subtypes and Their Clinical Implications
Sung Jun Ahn, Bio Joo, Mina Park, Hun Ho Park, Sang Hyun Suh, Sung Gwe Ahn, Jihwan Yoo
Cancer Res Treat. 2024;56(4):1105-1112. doi: 10.4143/crt.2024.138.
Reference
-
References
1. Nayak L, Lee EQ, Wen PY. Epidemiology of brain metastases. Curr Oncol Rep. 2012; 14:48–54.
Article2. Barker FG 2nd. Craniotomy for the resection of metastatic brain tumors in the U.S., 1988-2000: decreasing mortality and the effect of provider caseload. Cancer. 2004; 100:999–1007.3. Barnholtz-Sloan JS, Sloan AE, Davis FG, Vigneau FD, Lai P, Sawaya RE. Incidence proportions of brain metastases in patients diagnosed (1973 to 2001) in the Metropolitan Detroit Cancer Surveillance System. J Clin Oncol. 2004; 22:2865–72.
Article4. Counsell CE, Collie DA, Grant R. Incidence of intracranial tumours in the Lothian region of Scotland, 1989-90. J Neurol Neurosurg Psychiatry. 1996; 61:143–50.
Article5. Materljan E, Materljan B, Sepcic J, Tuskan-Mohar L, Zamolo G, Erman-Baldini I. Epidemiology of central nervous system tumors in Labin area, Croatia, 1974-2001. Croat Med J. 2004; 45:206–12.6. Schouten LJ, Rutten J, Huveneers HA, Twijnstra A. Incidence of brain metastases in a cohort of patients with carcinoma of the breast, colon, kidney, and lung and melanoma. Cancer. 2002; 94:2698–705.
Article7. Smedby KE, Brandt L, Backlund ML, Blomqvist P. Brain metastases admissions in Sweden between 1987 and 2006. Br J Cancer. 2009; 101:1919–24.
Article8. Oh CM, Won YJ, Jung KW, Kong HJ, Cho H, Lee JK, et al. Cancer statistics in Korea: incidence, mortality, survival, and prevalence in 2013. Cancer Res Treat. 2016; 48:436–50.
Article9. Jung KW, Won YJ, Oh CM, Kong HJ, Cho H, Lee JK, et al. Prediction of cancer incidence and mortality in Korea, 2016. Cancer Res Treat. 2016; 48:451–7.
Article10. Lee J, Lee JS, Park SH, Shin SA, Kim K. Cohort profile: The National Health Insurance Service-National Sample Cohort (NHIS-NSC), South Korea. Int J Epidemiol. 2017; 46:e15.
Article11. Rothman KJ, Greenland S. Modern epidemiology. 2nd ed. Philadelphia, PA: Lippincott Williams & Wilkins;1998.12. Ahmad OB, Boschi-Pinto C, Lopez AD, Murray CJ, Lozano R, Inoue M. Age standardization of rates: a new WHO standard. Geneva: World Health Organization;2001.13. Scheaffer RL, Mendenhall W 3rd, Ott L, Gerow KG. Elementary survey sampling. Boston, MA: Cengage Learning;2011.14. Tabouret E, Chinot O, Metellus P, Tallet A, Viens P, Goncalves A. Recent trends in epidemiology of brain metastases: an overview. Anticancer Res. 2012; 32:4655–62.15. Kim M, Na DL, Park SH, Jeon BS, Roh JK. Nervous system involvement by metastatic hepatocellular carcinoma. J Neurooncol. 1998; 36:85–90.16. Shao YY, Lu LC, Cheng AL, Hsu CH. Increasing incidence of brain metastasis in patients with advanced hepatocellular carcinoma in the era of antiangiogenic targeted therapy. Oncologist. 2011; 16:82–6.
Article17. Murakami K, Nawano S, Moriyama N, Sekiguchi R, Satake M, Fujimoto H, et al. Intracranial metastases of hepatocellular carcinoma: CT and MRI. Neuroradiology. 1996; 38 Suppl 1:S31–5.
Article18. Park Y, Kim KS, Kim K, Chie EK, Kim JH, Kim JS, et al. Nomogram prediction of survival in patients with brain metastases from hepatocellular carcinoma treated with whole-brain radiotherapy: a multicenter retrospective study. J Neurooncol. 2015; 125:377–83.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Primary Intracranial Malignant Melanoma with Extracranial Metastasis
- Reliability of Covariates in Baseline Survey of a Cohort Study: Epidemiological Investigation on Cancer Risk Among Residents Who Reside Near the Nuclear Power Plants in Korea
- Stroke Epidemiology in Thailand
- Stereotactic Radiosurgery for Metastatic Brain Tumor
- Post-treatment intracranial hemorrhage of brain metastases from hepatocellular carcinoma