Cancer Res Treat.
2015 Oct;47(4):943-948. 10.4143/crt.2014.016.
An Unusual Presentation of Pulmonary Mucosa-Associated Lymphoid Tissue Lymphoma as Diffuse Pulmonary Infiltrates with Spontaneous Regression
- Affiliations
-
- 1Division of Pulmonology, Allergy and Critical Care Medicine, Department of Internal Medicine, The Catholic University of Korea College of Medicine, Seoul, Korea. rkdwldud@catholic.ac.kr
- 2Department of Pathology, The Catholic University of Korea College of Medicine, Seoul, Korea.
- 3Department of Radiology, The Catholic University of Korea College of Medicine, Seoul, Korea.
- KMID: 2403416
- DOI: http://doi.org/10.4143/crt.2014.016
Abstract
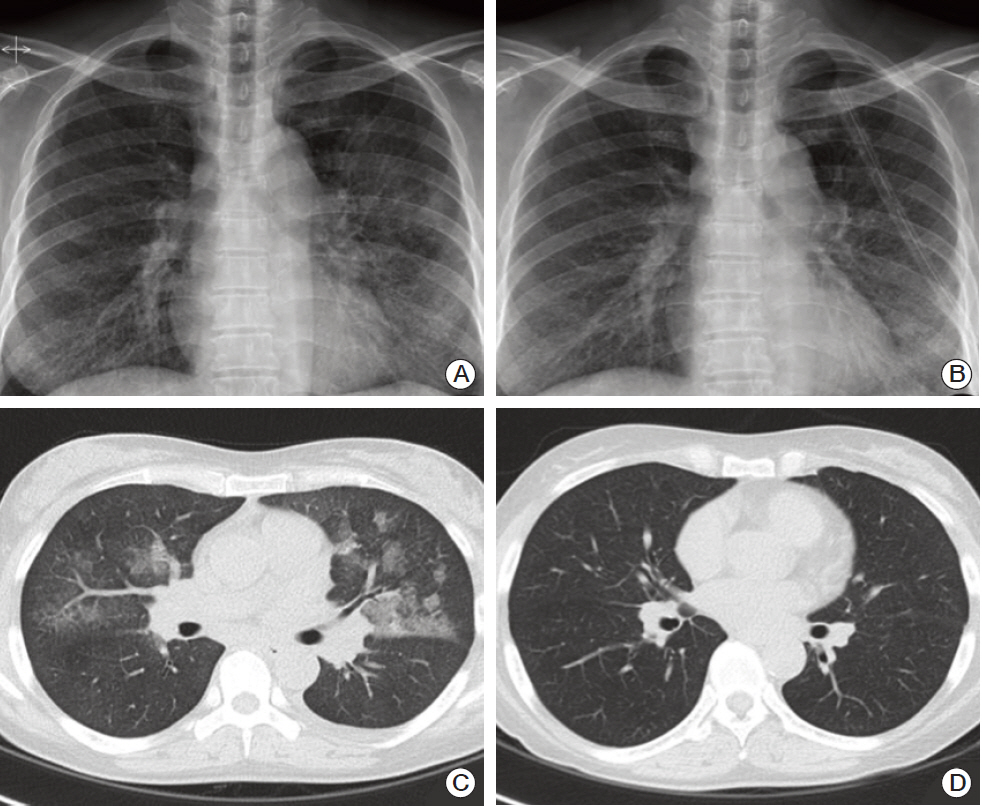
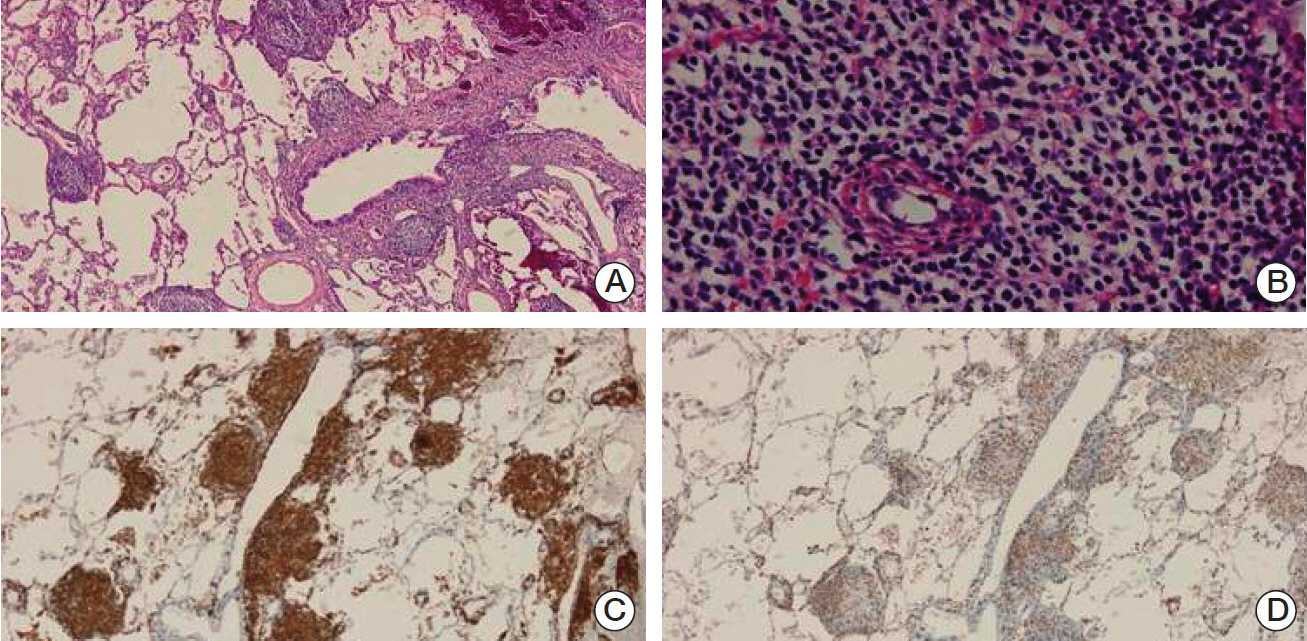
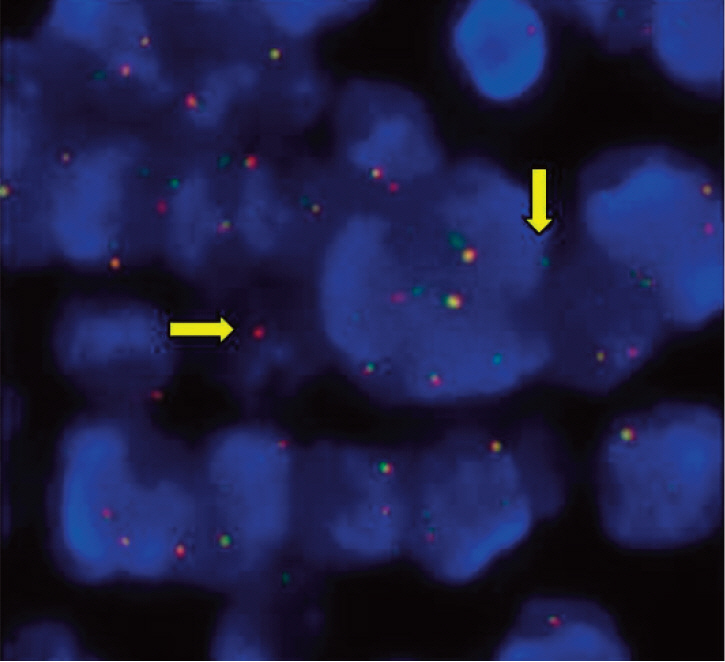
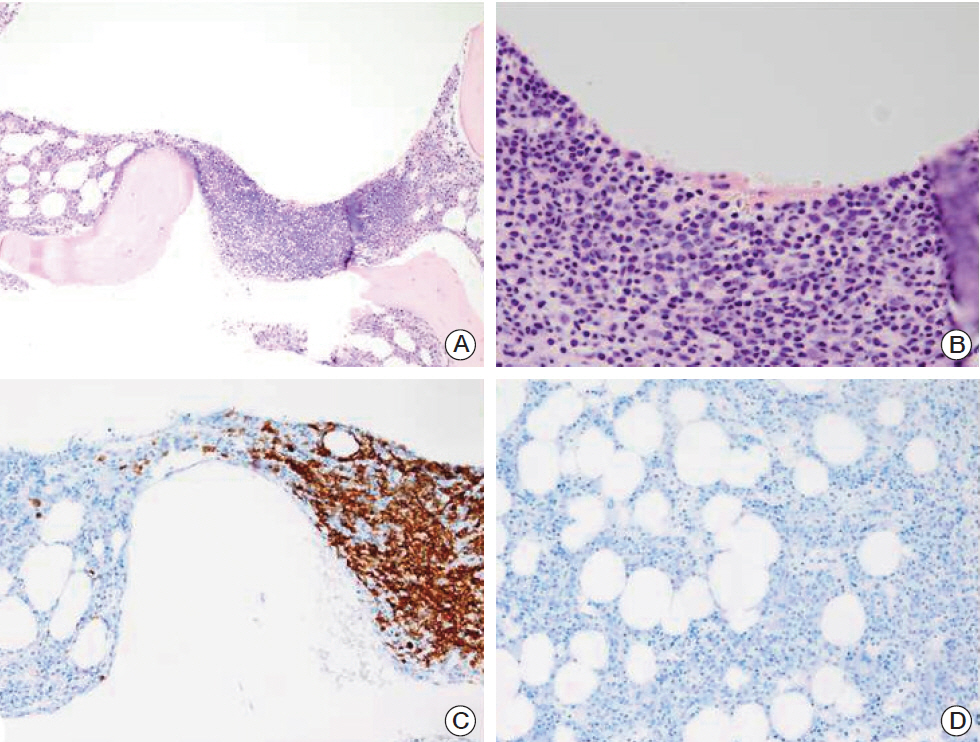
- A 57-year-old woman presented with cough and dyspnea for 2 months. Computed tomography of the chest showed diffuse ground-glass opacities in both lungs. Histologic examination via thoracoscopic lung biopsy revealed atypical lymphoproliferative lesion. Her symptoms and radiologic findings of the chest improved just after lung biopsy without any treatment. Therefore, she was discharged and monitored at an outpatient clinic. Two months later, pulmonary mucosa-associated lymphoid tissue (MALT) lymphoma was confirmed by the detection of API2-MALT1 translocation in fluorescent in situ hybridization analysis. Although the lung lesions resolved spontaneously, she received chemotherapy due to bone marrow involvement in her staging workup. Pulmonary MALT lymphoma is rare. Nodular or consolidative patterns are the most frequent radiologic findings. Although the disease has an indolent growth, it rarely resolves without treatment. We report an unusual case of pulmonary MALT lymphoma with diffuse interstitial abnormalities on image and spontaneous regression on clinical course.
MeSH Terms
Figure
Reference
-
References
1. Thieblemont C, de la Fouchardiere A, Coiffier B. Nongastric mucosa-associated lymphoid tissue lymphomas. Clin Lymphoma. 2003; 3:212–24.
Article2. Borie R, Wislez M, Thabut G, Antoine M, Rabbat A, Couderc LJ, et al. Clinical characteristics and prognostic factors of pulmonary MALT lymphoma. Eur Respir J. 2009; 34:1408–16.
Article3. Li AW, Xu JF, Zhou CC, Wu CY, Wang YL. Clinical characteristics and diagnosis of pulmonary mucosa-associated lymphoid tissue-derived (MALT) lymphoma: a retrospective analysis of 29 cases. Zhonghua Zhong Liu Za Zhi. 2012; 34:390–3.4. Ahmed S, Kussick SJ, Siddiqui AK, Bhuiya TA, Khan A, Sarewitz S, et al. Bronchial-associated lymphoid tissue lymphoma: a clinical study of a rare disease. Eur J Cancer. 2004; 40:1320–6.5. Randall TD. Bronchus-associated lymphoid tissue (BALT) structure and function. Adv Immunol. 2010; 107:187–241.6. Zhang WD, Guan YB, Li CX, Huang XB, Zhang FJ. Pulmonary mucosa-associated lymphoid tissue lymphoma: computed tomography and 18F fluorodeoxyglucose-positron emission tomography/computed tomography imaging findings and follow-up. J Comput Assist Tomogr. 2011; 35:608–13.7. Bae YA, Lee KS, Han J, Ko YH, Kim BT, Chung MJ, et al. Marginal zone B-cell lymphoma of bronchus-associated lymphoid tissue: imaging findings in 21 patients. Chest. 2008; 133:433–40.8. Koss MN. Malignant and benign lymphoid lesions of the lung. Ann Diagn Pathol. 2004; 8:167–87.
Article9. Cadranel J, Wislez M, Antoine M. Primary pulmonary lymphoma. Eur Respir J. 2002; 20:750–62.
Article10. Inagaki H, Li C, Okabe M, Nishikawa M, Nishikawa AM, Iida S, et al. Detection of API2-MALT1 fusion transcripts in cytologic specimens of patients with pulmonary mucosa-associated lymphoid tissue lymphoma. Int J Hematol. 2005; 82:59–62.
Article11. Troch M, Streubel B, Petkov V, Turetschek K, Chott A, Raderer M. Does MALT lymphoma of the lung require immediate treatment? An analysis of 11 untreated cases with long-term follow-up. Anticancer Res. 2007; 27:3633–7.12. Sato C, Suzuki H, Watanabe M, Kojima K, Tsuchida F, Takeda H. Spontaneous regression of mucosa-associated lymphoid tissue lymphoma of the lung. Nihon Kokyuki Gakkai Zasshi. 2010; 48:677–82.13. Ishimatsu Y, Kadota J, Iwashita T, Nagata T, Ishii H, Shikuwa C, et al. Macrolide antibiotics induce apoptosis of human peripheral lymphocytes in vitro. Int J Antimicrob Agents. 2004; 24:247–53.
Article14. Ishimatsu Y, Mukae H, Matsumoto K, Harada T, Hara A, Hara S, et al. Two cases with pulmonary mucosa-associated lymphoid tissue lymphoma successfully treated with clarithromycin. Chest. 2010; 138:730–3.
Article15. Arcaini L, Burcheri S, Rossi A, Passamonti F, Paulli M, Boveri E, et al. Nongastric marginal-zone B-cell MALT lymphoma: prognostic value of disease dissemination. Oncologist. 2006; 11:285–91.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Primary Pulmonary Extranodal Marginal Zone B-Cell Lymphoma of the MALT Type
- A Rare Radiological Presentation of Pulmonary Mucosa-Associated Lymphoid Tissue Lymphoma as Bronchovascular Thickening and Ground Glass Opacities with Concurrent Pancreas Involvement
- Malignant Lymphoma of Mucosa-associated Lymphoid Tissue Arising in the Conjunctiva
- A case report of the Pulmonary Malignant Lymphomaof the mucosa-associated lymphoid tissue(MALT)
- Cases of the Pulmonary Malignant Lymphoma of the Bronchus-Associated Lymphoid Tissue (BALT)