J Korean Med Sci.
2017 Oct;32(10):1702-1707. 10.3346/jkms.2017.32.10.1702.
Clinical Considerations When Applying Vital Signs in Pediatric Korean Triage and Acuity Scale
- Affiliations
-
- 1Department of Emergency Medicine, Seoul National University Hospital, Seoul, Korea. yhkwak@snuh.org
- 2Department of Pediatrics, Seoul National University College of Medicine, Seoul, Korea.
- 3Department of Emergency Medicine, Seoul National University College of Medicine, Seoul, Korea.
- KMID: 2400445
- DOI: http://doi.org/10.3346/jkms.2017.32.10.1702
Abstract
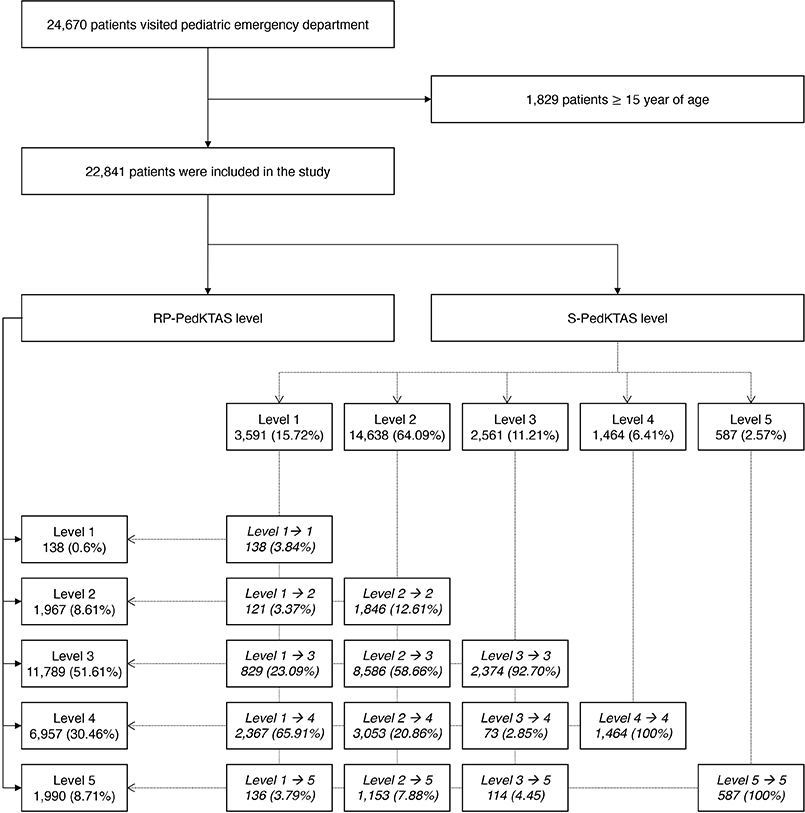
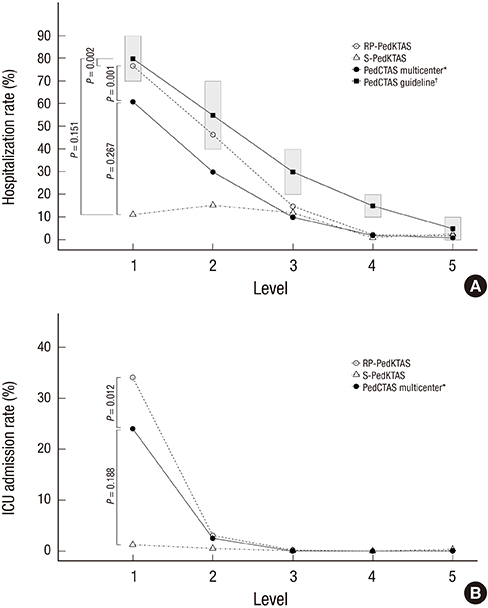
- Initial vital signs of children at the emergency department may be abnormal because of anxiety and irritability, resulting in unrealistic triage levels. This study aimed to evaluate the effectiveness of pediatric triage by clinical decision based on the patient's general condition. The Pediatric Korean Triage and Acuity Scale (PedKTAS) has been used nationwide for triage since 2016. The triage level, as assessed by an experienced triage nurse and based on the patient's clinical condition, was defined as the "˜real practice (RP)-level,' while the re-calculated triage level, as assessed by the direct application of initial vital signs, was defined as the "˜simulation (S)-level.' A total of 22,841 patients were triaged during the study period. The hospitalization rate according to RP-PedKTAS levels exhibited a significant correlation with the expected hospitalization rate suggested by the Pediatric Canadian Triage and Acuity Scale (CTAS) (P = 0.002), whereas the S-PedKTAS levels did not (P = 0.151). Compared with the previously reported pediatric CTAS level-specific hospitalization rate and intensive care unit (ICU) admission rate, RP-PedKTAS was significantly correlated with both hospitalization rate and ICU admission rate (P = 0.001 and P = 0.012, respectively). However, S-PedKTAS showed no significant correlation in both (P = 0.267 and P = 0.188, respectively). The determination of triage levels based on clinical decision rather than the direct application of abnormal initial vital signs to PedKTAS is more accurate in predicting the hospitalization rate and ICU admission rate.
MeSH Terms
Figure
Cited by 2 articles
-
Factors Associated with Triage Modifications Using Vital Signs in Pediatric Triage: a Nationwide Cross-Sectional Study in Korea
Bongjin Lee, Ikwan Chang, Do Kyun Kim, June Dong Park,
J Korean Med Sci. 2020;35(16):e102. doi: 10.3346/jkms.2020.35.e102.Transient and Adult Patients with Neurologic Diseases in the Pediatric Emergency Department: Trends and Characteristics
Ji-Hoon Na, Young-Mock Lee
J Clin Neurol. 2019;15(2):191-204. doi: 10.3988/jcn.2019.15.2.191.
Reference
-
1. Kim JH, Kim JW, Kim SY, Hong DY, Park SO, Baek KJ, Lee KR. Validation of the Korean Triage and Acuity Scale compare to triage by emergency severity index for emergency adult patient: preliminary study in a tertiary hospital emergency medical center. J Korean Soc Emerg Med. 2016; 27:436–441.2. Lim T, Park J, Je S. Pediatric Korean Triage and Acuity Scale. Pediatr Emerg Med J. 2015; 2:53–58.3. Fleming S, Thompson M, Stevens R, Heneghan C, Plüddemann A, Maconochie I, Tarassenko L, Mant D. Normal ranges of heart rate and respiratory rate in children from birth to 18 years of age: a systematic review of observational studies. Lancet. 2011; 377:1011–1018.4. Takahashi T, Inoue N, Shimizu N, Terakawa T, Goldman RD. ‘Down-triage’ for children with abnormal vital signs: evaluation of a new triage practice at a paediatric emergency department in Japan. Emerg Med J. 2016; 33:533–537.5. Warren DW, Jarvis A, LeBlanc L, Gravel J; CTAS National Working Group. Canadian Association of Emergency Physicians; National Emergency Nurses Affiliation; Association des Médecins d’Urgence du Québec; Canadian Paediatric Society; Society of Rural Physicians of Canada. Revisions to the Canadian Triage and Acuity Scale paediatric guidelines (PaedCTAS). CJEM. 2008; 10:224–243.6. Gouin S, Gravel J, Amre DK, Bergeron S. Evaluation of the Paediatric Canadian Triage and Acuity Scale in a pediatric ED. Am J Emerg Med. 2005; 23:243–247.7. Sprivulis PC, Da Silva JA, Jacobs IG, Frazer AR, Jelinek GA. The association between hospital overcrowding and mortality among patients admitted via Western Australian emergency departments. Med J Aust. 2006; 184:208–212.8. Bullard MJ, Chan T, Brayman C, Warren D, Musgrave E, Unger B; Members of the CTAS National Working Group. Revisions to the Canadian Emergency Department Triage and Acuity Scale (CTAS) guidelines. CJEM. 2014; 16:485–489.9. Gravel J, Manzano S, Arsenault M. Safety of a modification of the triage level for febrile children 6 to 36 months old using the Paediatric Canadian Triage and Acuity Scale. CJEM. 2008; 10:32–37.10. Gravel J, Fitzpatrick E, Gouin S, Millar K, Curtis S, Joubert G, Boutis K, Guimont C, Goldman RD, Dubrovsky AS, et al. Performance of the Canadian Triage and Acuity Scale for children: a multicenter database study. Ann Emerg Med. 2013; 61:27–32.e3.11. Mirhaghi A, Heydari A, Mazlom R, Ebrahimi M. The reliability of the Canadian Triage and Acuity Scale: meta-analysis. N Am J Med Sci. 2015; 7:299–305.12. Nijman RG, Thompson M, van Veen M, Perera R, Moll HA, Oostenbrink R. Derivation and validation of age and temperature specific reference values and centile charts to predict lower respiratory tract infection in children with fever: prospective observational study. BMJ. 2012; 345:e4224.13. O'Leary F, Hayen A, Lockie F, Peat J. Defining normal ranges and centiles for heart and respiratory rates in infants and children: a cross-sectional study of patients attending an Australian tertiary hospital paediatric emergency department. Arch Dis Child. 2015; 100:733–737.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Consideration in Korean Triage and Acuity Scale for febrile pediatric patients: symptom duration
- Abuse of the Korean Triage and Acuity Scale in the assessment of emergency medical facilities
- Inter-rater agreement of Korean Triage and Acuity Scale between emergency physicians and nurses
- Factors Associated with Triage Modifications Using Vital Signs in Pediatric Triage: a NationwideCross-Sectional Study in Korea
- A Delphi study for the application of Korean Triage and Acuity Scale to children