Kosin Med J.
2017 Dec;32(2):258-262. 10.7180/kmj.2017.32.2.258.
A Case of Primary Tracheal Schwannoma
- Affiliations
-
- 1Department of Internal Medicine, Yonsei University College of Medicine, Gangnam Severance Hospital, Seoul, Korea. gomdanism@yuhs.ac.kr
- KMID: 2400271
- DOI: http://doi.org/10.7180/kmj.2017.32.2.258
Abstract
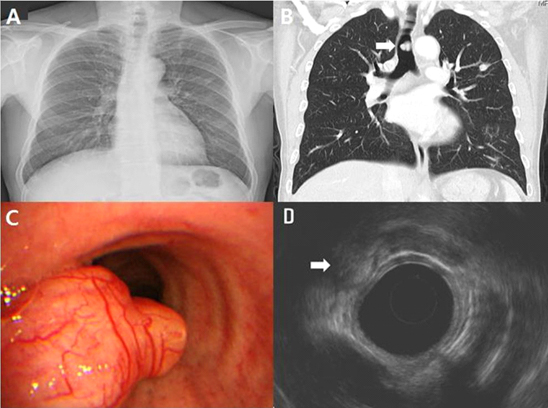
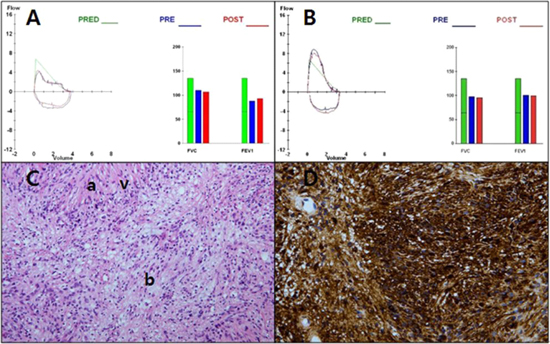
- Although benign nerve sheath tumors have been described, primary tracheal schwannomas are extremely rare. We report a case of primary tracheal schwannoma, a rare benign nerve sheath tumor in a 58-year-old man with atypical symptoms of chronic cough, sputum and dyspnea for 2 months. Chest computerized tomography showed a 1.7 cm polypoid lesion in posterior wall of mid trachea. The results of bronchoscopic biopsy and immuno-histo-chemical studies were consistent with schwannoma. A surgical treatment of tumor resection and tracheal reconstruction by end-to-end anastomosis was performed.
Keyword
MeSH Terms
Figure
Reference
-
1. Isaac BT, Christopher DJ, Thangakunam B, Gupta M. Tracheal schwannoma: Completely resected with therapeutic bronchoscopic techniques. Lung India. 2015; 32:271–273.
Article2. Ge X, Han F, Guan W, Sun J, Guo X. Optimal treatment for primary benign intratracheal schwannoma: A case report and review of the literature. Oncol Lett. 2015; 10:2273–2276.
Article3. Jung YY, Hong ME, Han J, Kim TS, Kim J, Shim YM, et al. Bronchial schwannomas: clinicopathologic analysis of 7 cases. Korean J Pathol. 2013; 47:326–331.
Article4. Rusch VW, Schmidt RA. Tracheal schwannoma: management by endoscopic laser resection. Thorax. 1994; 49:85–86.
Article5. Righini CA, Lequeux T, Laverierre MH, Reyt E. Primary tracheal schwannoma: one case report and a literature review. Eur Arch Otorhinolaryngol. 2005; 262:157–160.
Article6. Takeda K, Horiuchi M, Nakaya M, Yamaguchi K, Fujikawa A. Schwannoma of the trachea; a new resection technique. Auris Nasus Larynx. 2003; 30:425–427.
Article7. Kasahara K, Fukuoka K, Konishi M, Hamada K, Maeda K, Mikasa K, et al. Two cases of endobronchial neurilemmoma and review of the literature in Japan. Intern Med. 2003; 42:1215–1218.
Article8. Horovitz AG, Khalil KG, Verani RR, Guthrie AM, Cowan DF. Primary intratracheal neurilemoma. J Thorac Cardiovasc Surg. 1983; 85:313–317.
Article