Clin Endosc.
2017 Nov;50(6):530-536. 10.5946/ce.2017.134.
Diagnosis and Management of Rectal Neuroendocrine Tumors
- Affiliations
-
- 1Division of Gastroenterology, Icahn School of Medicine at Mount Sinai, New York, NY, USA. Nikhil.Kumta@mountsinai.org
- KMID: 2398303
- DOI: http://doi.org/10.5946/ce.2017.134
Abstract
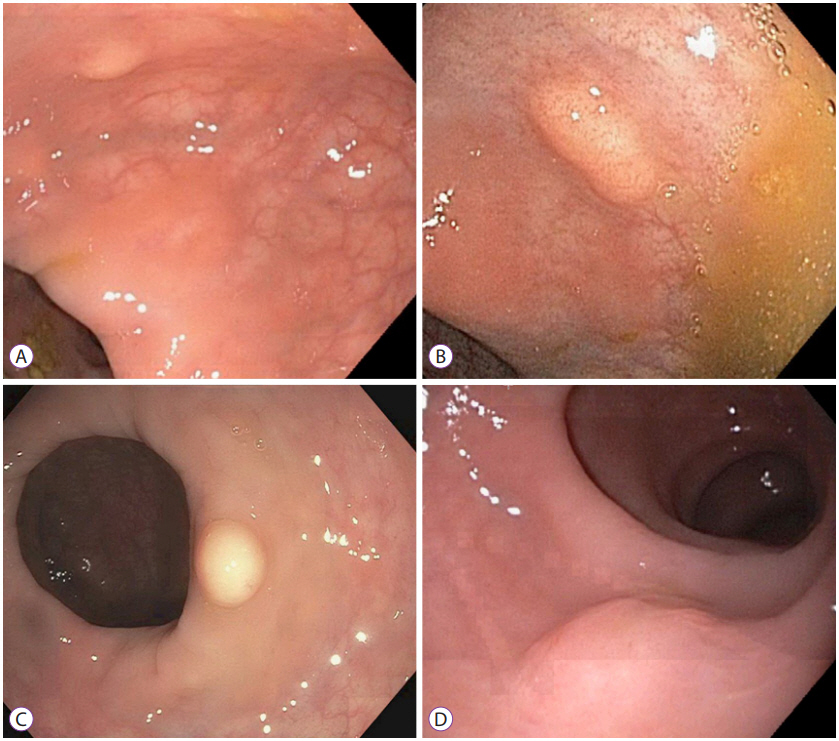
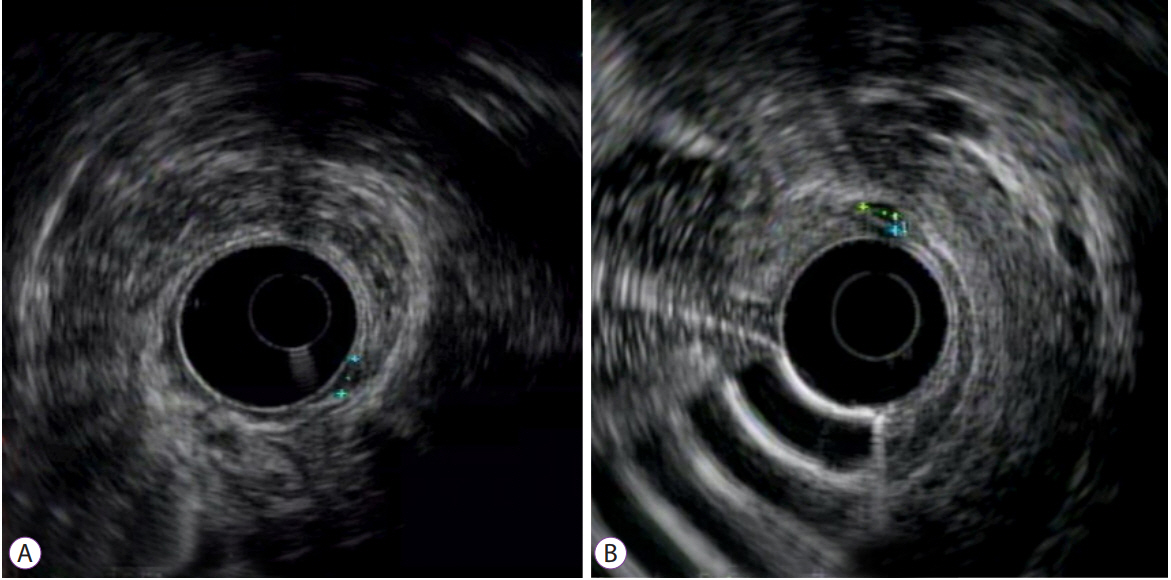
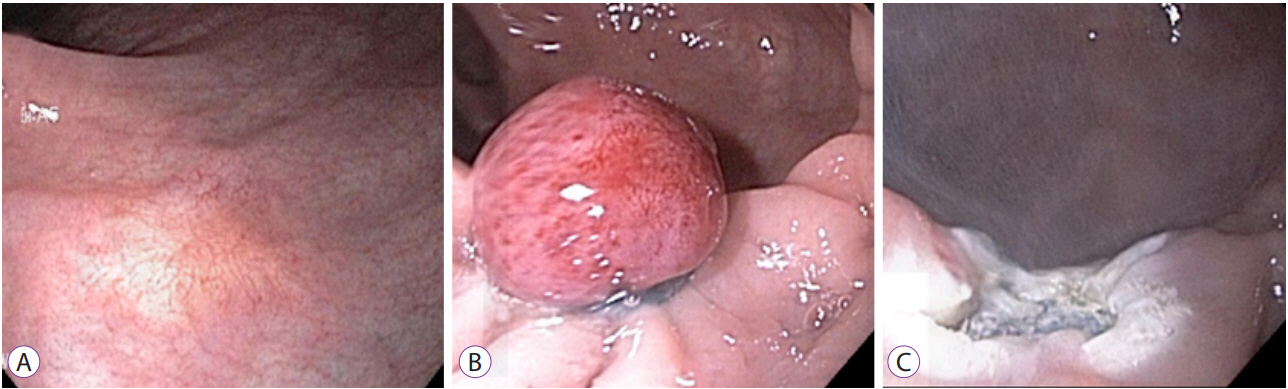
- The incidence of rectal neuroendocrine tumors (NETs) has increased by almost ten-fold over the past 30 years. There has been a heightened awareness of the malignant potential of rectal NETs. Fortunately, many rectal NETs are discovered at earlier stages due to colon cancer screening programs. Endoscopic ultrasound is useful in assessing both residual tumor burden after retrospective diagnosis and tumor characteristics to help guide subsequent management. Current guidelines suggest endoscopic resection of rectal NETs ≤10 mm as a safe therapeutic option given their low risk of metastasis. Although a number of endoscopic interventions exist, the best technique for resection has not been identified. Endoscopic submucosal dissection (ESD) has high complete and en-bloc resection rates, but also an increased risk of complications including perforation. In addition, ESD is only performed at tertiary centers by experienced advanced endoscopists. Endoscopic mucosal resection has been shown to have variable complete resection rates, but modifications to the technique such as the addition of band ligation have improved outcomes. Prospective studies are needed to further compare the available endoscopic interventions, and to elucidate the most appropriate course of management of rectal NETs.
Keyword
MeSH Terms
Figure
Cited by 2 articles
-
내시경 완전 절제 후 다발성 간전이로 재발한 저등급 직장 신경내분비종양
Ik Hyun Jo, Kang-Moon Lee, Dae Bum Kim, Ji Min Lee
Korean J Gastroenterol. 2020;76(5):251-255. doi: 10.4166/kjg.2020.096.Proper Treatment Option for Small Rectal Neuroendocrine Tumors Using Precut Endoscopic Mucosal Resection
Seun Ja Park
Clin Endosc. 2017;50(6):516-517. doi: 10.5946/ce.2017.182.
Reference
-
1. Yao JC, Hassan M, Phan A, et al. One hundred years after “carcinoid”: epidemiology of and prognostic factors for neuroendocrine tumors in 35,825 cases in the United States. J Clin Oncol. 2008; 26:3063–3072.
Article2. Fraenkel M, Kim M, Faggiano A, de Herder WW, Valk GD. Incidence of gastroenteropancreatic neuroendocrine tumours: a systematic review of the literature. Endocr Relat Cancer. 2014; 21:R153–R163.
Article3. Caplin M, Sundin A, Nillson O, et al. ENETS consensus guidelines for the management of patients with digestive neuroendocrine neoplasms: colorectal neuroendocrine neoplasms. Neuroendocrinology. 2012; 95:88–97.
Article4. Modlin IM, Lye KD, Kidd M. A 5-decade analysis of 13,715 carcinoid tumors. Cancer. 2003; 97:934–959.
Article5. Dasari A, Shen C, Halperin D, et al. Trends in the incidence, prevalence, and survival outcomes in patients with neuroendocrine tumors in the United States. JAMA Oncol. 2017; 3:1335–1342.
Article6. Rindi G, Petrone G, Inzani F. The 2010 WHO classification of digestive neuroendocrine neoplasms: a critical appraisal four years after its introduction. Endocr Pathol. 2014; 25:186–192.7. Shim KN, Yang SK, Myung SJ, et al. Atypical endoscopic features of rectal carcinoids. Endoscopy. 2004; 36:313–316.
Article8. Anthony LB, Strosberg JR, Klimstra DS, et al. The NANETS consensus guidelines for the diagnosis and management of gastrointestinal neuroendocrine tumors (nets): well-differentiated nets of the distal colon and rectum. Pancreas. 2010; 39:767–774.9. Mandair D, Caplin ME. Colonic and rectal NET’s. Best Pract Res Clin Gastroenterol. 2012; 26:775–789.
Article10. Weinstock B, Ward SC, Harpaz N, Warner RR, Itzkowitz S, Kim MK. Clinical and prognostic features of rectal neuroendocrine tumors. Neuroendocrinology. 2013; 98:180–187.
Article11. American Joint Committee on Cancer (AJCC). Cancer staging manual [Internet]. Chicago (IL): American Joint Committee on Cancer (AJCC);c2016. [cited 2017 Aug 22]. Available from: https://cancerstaging.org/references-tools/deskreferences/Pages/default.aspx.12. Park CH, Cheon JH, Kim JO, et al. Criteria for decision making after endoscopic resection of well-differentiated rectal carcinoids with regard to potential lymphatic spread. Endoscopy. 2011; 43:790–795.
Article13. Mani S, Modlin IM, Ballantyne G, Ahlman H, West B. Carcinoids of the rectum. J Am Coll Surg. 1994; 179:231–248.14. Fusaroli P, Caletti G. Endoscopic ultrasonography: current clinical role. Eur J Gastroenterol Hepatol. 2005; 17:293–301.
Article15. Basuroy R, Haji A, Ramage JK, Quaglia A, Srirajaskanthan R. Review article: the investigation and management of rectal neuroendocrine tumours. Aliment Pharmacol Ther. 2016; 44:332–345.
Article16. Kobayashi K, Katsumata T, Yoshizawa S, et al. Indications of endoscopic polypectomy for rectal carcinoid tumors and clinical usefulness of endoscopic ultrasonography. Dis Colon Rectum. 2005; 48:285–291.
Article17. Park SB, Kim DJ, Kim HW, et al. Is endoscopic ultrasonography essential for endoscopic resection of small rectal neuroendocrine tumors? World J Gastroenterol. 2017; 23:2037–2043.
Article18. Ishii N, Horiki N, Itoh T, et al. Endoscopic submucosal dissection and preoperative assessment with endoscopic ultrasonography for the treatment of rectal carcinoid tumors. Surg Endosc. 2010; 24:1413–1419.
Article19. Son HJ, Sohn DK, Hong CW, et al. Factors associated with complete local excision of small rectal carcinoid tumor. Int J Colorectal Dis. 2013; 28:57–61.
Article20. de Mestier L, Brixi H, Gincul R, Ponchon T, Cadiot G. Updating the management of patients with rectal neuroendocrine tumors. Endoscopy. 2013; 45:1039–1046.
Article21. Onozato Y, Kakizaki S, Iizuka H, Sohara N, Mori M, Itoh H. Endoscopic treatment of rectal carcinoid tumors. Dis Colon Rectum. 2010; 53:169–176.
Article22. Kim BN, Sohn DK, Hong CW, et al. Atypical endoscopic features can be associated with metastasis in rectal carcinoid tumors. Surg Endosc. 2008; 22:1992–1996.
Article23. Kim KM, Eo SJ, Shim SG, et al. Treatment outcomes according to endoscopic treatment modalities for rectal carcinoid tumors. Clin Res Hepatol Gastroenterol. 2013; 37:275–282.
Article24. Yang DH, Park Y, Park SH, et al. Cap-assisted EMR for rectal neuroendocrine tumors: comparisons with conventional EMR and endoscopic submucosal dissection (with videos). Gastrointest Endosc. 2016; 83:1015–1022. quiz 1023-.e6.
Article25. Nakamura K, Osada M, Goto A, et al. Short- and long-term outcomes of endoscopic resection of rectal neuroendocrine tumours: analyses according to the WHO 2010 classification. Scand J Gastroenterol. 2016; 51:448–455.
Article26. Jeon JH, Cheung DY, Lee SJ, et al. Endoscopic resection yields reliable outcomes for small rectal neuroendocrine tumors. Dig Endosc. 2014; 26:556–563.
Article27. Kim HH, Park SJ, Lee SH, et al. Efficacy of endoscopic submucosal resection with a ligation device for removing small rectal carcinoid tumor compared with endoscopic mucosal resection: analysis of 100 cases. Dig Endosc. 2012; 24:159–163.
Article28. Zhou X, Xie H, Xie L, Li J, Cao W, Fu W. Endoscopic resection therapies for rectal neuroendocrine tumors: a systematic review and meta-analysis. J Gastroenterol Hepatol. 2014; 29:259–268.
Article29. Zhang HP, Wu W, Yang S, Lin J. Endoscopic treatments for rectal neuroendocrine tumors smaller than 16 mm: a meta-analysis. Scand J Gastroenterol. 2016; 51:1345–1353.30. Zhou PH, Yao LQ, Qin XY, et al. Advantages of endoscopic submucosal dissection with needle-knife over endoscopic mucosal resection for small rectal carcinoid tumors: a retrospective study. Surg Endosc. 2010; 24:2607–2612.
Article31. Chen T, Yao LQ, Xu MD, et al. Efficacy and safety of endoscopic submucosal dissection for colorectal carcinoids. Clin Gastroenterol Hepatol. 2016; 14:575–581.32. Park HW, Byeon JS, Park YS, et al. Endoscopic submucosal dissection for treatment of rectal carcinoid tumors. Gastrointest Endosc. 2010; 72:143–149.
Article33. Zhong DD, Shao LM, Cai JT. Endoscopic mucosal resection vs endoscopic submucosal dissection for rectal carcinoid tumours: a systematic review and meta-analysis. Colorectal Dis. 2013; 15:283–291.34. He L, Deng T, Luo H. Efficacy and safety of endoscopic resection therapies for rectal carcinoid tumors: a meta-analysis. Yonsei Med J. 2015; 56:72–81.
Article35. Lee DS, Jeon SW, Park SY, et al. The feasibility of endoscopic submucosal dissection for rectal carcinoid tumors: comparison with endoscopic mucosal resection. Endoscopy. 2010; 42:647–651.
Article36. Park SB, Kim HW, Kang DH, Choi CW, Kim SJ, Nam HS. Advantage of endoscopic mucosal resection with a cap for rectal neuroendocrine tumors. World J Gastroenterol. 2015; 21:9387–9393.
Article37. Choi CW, Kang DH, Kim HW, et al. Comparison of endoscopic resection therapies for rectal carcinoid tumor: endoscopic submucosal dissection versus endoscopic mucosal resection using band ligation. J Clin Gastroenterol. 2013; 47:432–436.38. Ono A, Fujii T, Saito Y, et al. Endoscopic submucosal resection of rectal carcinoid tumors with a ligation device. Gastrointest Endosc. 2003; 57:583–587.
Article39. Mashimo Y, Matsuda T, Uraoka T, et al. Endoscopic submucosal resection with a ligation device is an effective and safe treatment for carcinoid tumors in the lower rectum. J Gastroenterol Hepatol. 2008; 23:218–221.
Article40. Niimi K, Goto O, Fujishiro M, et al. Endoscopic mucosal resection with a ligation device or endoscopic submucosal dissection for rectal carcinoid tumors: an analysis of 24 consecutive cases. Dig Endosc. 2012; 24:443–447.
Article41. Bang BW, Park JS, Kim HK, Shin YW, Kwon KS, Kim JM. Endoscopic resection for small rectal neuroendocrine tumors: comparison of endoscopic submucosal resection with band ligation and endoscopic submucosal dissection. Gastroenterol Res Pract. 2016; 2016:6198927.
Article42. Wang X, Xiang L, Li A, et al. Endoscopic submucosal dissection for the treatment of rectal carcinoid tumors 7-16 mm in diameter. Int J Colorectal Dis. 2015; 30:375–380.43. Jeon SM, Lee JH, Hong SP, Kim TI, Kim WH, Cheon JH. Feasibility of salvage endoscopic mucosal resection by using a cap for remnant rectal carcinoids after primary EMR. Gastrointest Endosc. 2011; 73:1009–1014.
Article44. Sekiguchi M, Sekine S, Sakamoto T, et al. Excellent prognosis following endoscopic resection of patients with rectal neuroendocrine tumors despite the frequent presence of lymphovascular invasion. J Gastroenterol. 2015; 50:1184–1189.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Multiple Rectal Neuroendocrine Tumors: Report of Five Cases
- Endoscopic Treatment Outcome of Rectal Neuroendocrine Tumors Removed by Ligation-assisted Endoscopic Submucosal Resection
- Neuroendocrine Tumors of the Female Reproductive Tract: A Literature Review
- Diagnosis and Management of Upper Gastrointestinal Neuroendocrine Tumors
- Diagnosis and Treatment of Rectal Neuroendocrine Tumor