Ann Hepatobiliary Pancreat Surg.
2017 Nov;21(4):237-242. 10.14701/ahbps.2017.21.4.237.
Extra-gastrointestinal stromal tumor of the pancreas: report of a case
- Affiliations
-
- 1Department of Surgery, Kyungpook National University Chilgok Hospital, Kyungpook National University School of Medicine, Daegu, Korea. kwonhj95@naver.com
- KMID: 2397806
- DOI: http://doi.org/10.14701/ahbps.2017.21.4.237
Abstract
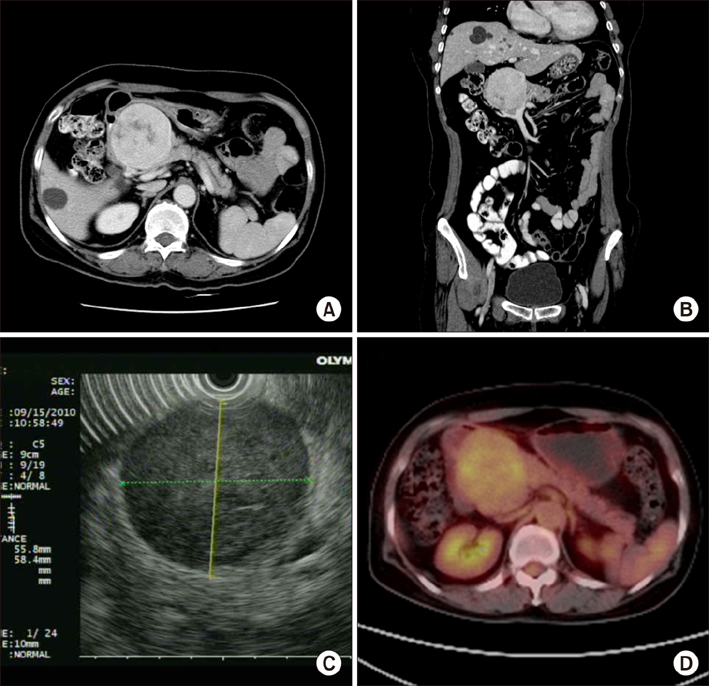
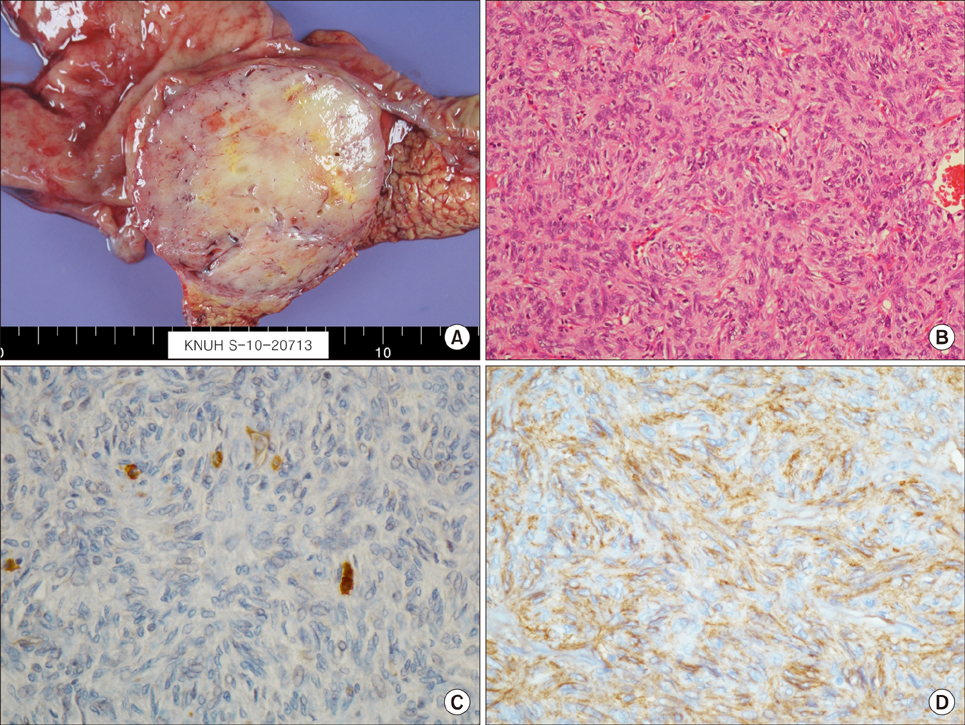
- Gastrointestinal tumors (GISTs) of the pancreas are extremely rare with limited individual case reports and small number of case series. Herein, we report a case of pancreatic extragastrointestinal stromal tumor (EGIST) along with literature review. A 64-year-old female patient was referred to us for treatment of an abdominal mass detected by ultrasonographic examination. The tumor was located in the periamullary region. Under a preoperative diagnosis of a duodenal GIST, we performed a pylorus preserving pancreatoduodenectomy for this lesion. Laboratory examination results were within normal ranges. On pathologic gross examination, the tumor measured at 7 cm in its greatest dimension almost entirely involved the pancreatic head. Its cut surface was rubbery and white. It was surrounded by a thin pseudocapsule and well demarcated. Histopathological examination of the specimen showed a cellular lesion with compressed pancreatic tissue at peripheral. Mitotic count was 5 per 50 high-power fields. Immunohistochemically, neoplastic cells were positive for antibodies against C-KIT (CD117), CD 34, and vimentin. However, smooth-muscle actin reactions with antibodies against S-100 or desmin were negative. Based on above findings, the tumor was finally diagnosed as GISTs originating from the pancreas. The patient has been followed up postoperatively for 72 months. There is no evidence of recurrence. Here we report this case of pancreatic EGIST presenting as a solid neoplasm along with literature review of cases previously described. Our review on pancreatic EGISTs is limited and insufficient to make a conclusion regarding its clinical features. Those manifested large masses tended to have an aggressive biological and clinical behavior. Thus, pancreatic EGISTs need to be carefully differentiated. Adequate surgical intervention is necessary for pancreatic EGISTs.
MeSH Terms
Figure
Reference
-
1. Fletcher CD, Berman JJ, Corless C, Gorstein F, Lasota J, Longley BJ, et al. Diagnosis of gastrointestinal stromal tumors: A consensus approach. Hum Pathol. 2002; 33:459–465.2. Agaimy A, Wünsch PH. Gastrointestinal stromal tumours: a regular origin in the muscularis propria, but an extremely diverse gross presentation. A review of 200 cases to critically re-evaluate the concept of so-called extra-gastrointestinal stromal tumours. Langenbecks Arch Surg. 2006; 391:322–329.3. Park JK, Choi SH, Lee S, Min KO, Yun SS, Jeon HM. Malignant gastrointestinal stromal tumor of the gallbladder. J Korean Med Sci. 2004; 19:763–767.4. Neto MR, Machuca TN, Pinho RV, Yuasa LD, Bleggi-Torres LF. Gastrointestinal stromal tumor: report of two unusual cases. Virchows Arch. 2004; 444:594–596.5. Yamaura K, Kato K, Miyazawa M, Haba Y, Muramatsu A, Miyata K, et al. Stromal tumor of the pancreas with expression of c-kit protein: report of a case. J Gastroenterol Hepatol. 2004; 19:467–470.6. Krska Z, Pesková M, Povýsil C, Horejs J, Sedlácková E, Kudrnová Z. GIST of pancreas. Prague Med Rep. 2005; 106:201–208.7. Daum O, Klecka J, Ferda J, Treska V, Vanecek T, Sima R, et al. Gastrointestinal stromal tumor of the pancreas: case report with documentation of KIT gene mutation. Virchows Arch. 2005; 446:470–472.8. Showalter SL, Lloyd JM, Glassman DT, Berger AC. Extra-gastrointestinal stromal tumor of the pancreas: case report and a review of the literature. Arch Surg. 2008; 143:305–308.9. Trabelsi A, Yacoub-Abid LB, Mtimet A, Abdelkrim SB, Hammedi F, Ali AB, et al. Gastrointestinal stromal tumor of the pancreas: a case report and review of the literature. N Am J Med Sci. 2009; 1:324–326.10. Padhi S, Kongara R, Uppin SG, Uppin MS, Prayaga AK, Challa S, et al. Extragastrointestinal stromal tumor arising in the pancreas: a case report with a review of the literature. JOP. 2010; 11:244–248.11. Saif MW, Hotchkiss S, Kaley K. Gastrointestinal stromal tumors of the pancreas. JOP. 2010; 11:405–406. author reply 412.12. Rao RN, Vij M, Singla N, Kumar A. Malignant pancreatic extra-gastrointestinal stromal tumor diagnosed by ultrasound guided fine needle aspiration cytology. A case report with a review of the literature. JOP. 2011; 12:283–286.13. Čečka F, Jon B, Ferko A, Šubrt Z, Nikolov DH, Tyčová V. Long-term survival of a patient after resection of a gastrointestinal stromal tumor arising from the pancreas. Hepatobiliary Pancreat Dis Int. 2011; 10:330–332.14. Vij M, Agrawal V, Pandey R. Malignant extra-gastrointestinal stromal tumor of the pancreas. A case report and review of literature. JOP. 2011; 12:200–204.15. Yang F, Jin C, Fu D, Ni Q. Extra-gastrointestinal stromal tumor of the pancreas: clinical characteristics, diagnosis, treatment, and outcome. J Surg Oncol. 2011; 103:739–740.16. Kim HH, Koh YS, Park EK, Seoung JS, Hur YH, Kim JC, et al. Primary extragastrointestinal stromal tumor arising in the pancreas: report of a case. Surg Today. 2012; 42:386–390.17. Tian YT, Liu H, Shi SS, Xie YB, Xu Q, Zhang JW, et al. Malignant extra-gastrointestinal stromal tumor of the pancreas: Report of two cases and review of the literature. World J Gastroenterol. 2014; 20:863–868.18. Elgeidie A, El-Magd EA, El-Maaty SRA, El-Hawary AK. Pancreatic gastrointestinal stromal tumor: a case report. Int J Surg Case Rep. 2016; 29:67–70.19. Kang YK, Kang HJ, Kim KM, Sohn T, Choi D, Ryu MH, et al. Clinical practice guideline for accurate diagnosis and effective treatment of gastrointestinal stromal tumor in Korea. Cancer Res Treat. 2012; 44:85–96.20. Valsangkar N, Sehdev A, Misra S, Zimmers TA, O'Neil BH, Koniaris LG. Current management of gastrointestinal stromal tumors: surgery, current biomarkers, mutations, and therapy. Surgery. 2015; 158:1149–1164.21. Joensuu H, Hohenberger P, Corless CL. Gastrointestinal stromal tumour. Lancet. 2013; 382:973–983.22. DeMatteo RP, Lewis JJ, Leung D, Mudan SS, Woodruff JM, Brennan MF. Two hundred gastrointestinal stromal tumors: recurrence patterns and prognostic factors for survival. Ann Surg. 2000; 231:51–58.23. Reith JD, Goldblum JR, Lyles RH, Weiss SW. Extragastrointestinal (soft tissue) stromal tumors: an analysis of 48 cases with emphasis on histologic predictors of outcome. Mod Pathol. 2000; 13:577–585.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Extra-Gastrointestinal stromal tumor of the pancreas with c-KIT gene mutation: Report of a case
- Diagnosis of a Gastrointestinal Stromal Tumor Presenting as a Prostatic Mass: A Case Report
- A Case of Anaplastic Carcinoma of the Pancreas Mimicking a Gastrointestinal Stromal Tumor
- Extra-Gastrointestinal Stromal Tumor of Retroperitoneal Origin: A Case Report
- Gastrointestinal Stromal Tumor in a Patient Complaining about Less Decreasing Abdominal Obesity