Asia Pac Allergy.
2015 Oct;5(4):203-209. 10.5415/apallergy.2015.5.4.203.
Attitudes, practices on allergic rhinitis of generalists and specialists in Philippine National Capital Region
- Affiliations
-
- 1Department of Otolaryngology-Head & Neck Surgery, St. Luke's Medical Center, Quezon City 1112, Philippines. gret_navarrolocsin@yahoo.com
- KMID: 2397036
- DOI: http://doi.org/10.5415/apallergy.2015.5.4.203
Abstract
- BACKGROUND
Treatment of allergic rhinitis (AR) consistent with consensus guidelines is reported to result in better patient outcomes. However, physicians may manage patients independently of guidelines. Asian data on physician perspectives regarding AR diagnosis and management is limited.
OBJECTIVE
The study objective is to assess attitudes and practices on AR of Filipino specialists and generalists.
METHODS
A cross sectional survey of 100 specialists and 100 generalists was conducted from November 2014 to January 2015. A previously validated and pilot tested questionnaire was administered via structured face to face interviews.
RESULTS
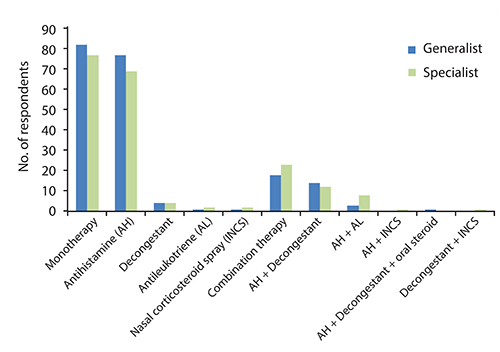
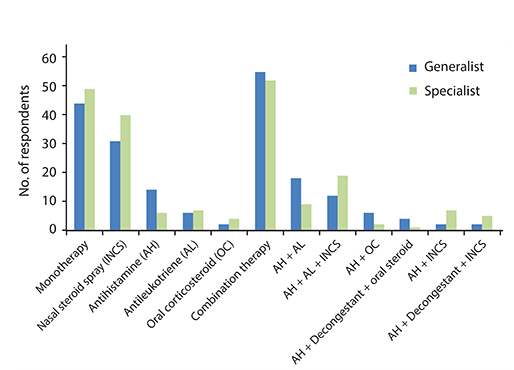
Specialists reported greater adequate knowledge of AR (specialists, 58%; generalists, 39%) and adherence to guidelines (specialists, 84%; generalists, 54%). Diagnostic tests were not routinely used (specialists, 81%; generalists, 92%). Monotherapy, specifically antihistamines, was preferred for mild AR. For moderate-severe AR, preference for monotherapy versus combination therapy (specialists, 49% vs. 51%; generalists, 44% vs. 56%) was similar. Both groups preferred intranasal corticosteroid spray (INCS) for monotherapy and antileukotrienes, antihistamines, INCS for combination therapy. For adjuvant therapy, specialists (82%) preferred nasal irrigation/douche. Primary consideration for choice of therapy was efficacy. Cost was the perceived reason for patients' noncompliance with treatment.
CONCLUSION
Despite differences in awareness of and adherence to guidelines, prescribing patterns on management of mild and moderate-severe AR are similar among Filipino specialists and generalists. This can be attributed to a shared perception of efficacy and cost as drivers for therapeutic choices.
MeSH Terms
Figure
Cited by 2 articles
-
Great learning, much networking, and friendship
Yoon-Seok Chang
Asia Pac Allergy. 2015;5(4):191-192. doi: 10.5415/apallergy.2015.5.4.191.Attitudes, practices on allergic rhinitis of three socioeconomic classes of Filipinos in the National Capital Region
Cecilia Gretchen Navarro-Locsin, Joel A. Romualdez
Asia Pac Allergy. 2016;6(2):94-100. doi: 10.5415/apallergy.2016.6.2.94.
Reference
-
1. Ozdoganoglu T, Songu M. The burden of allergic rhinitis and asthma. Ther Adv Respir Dis. 2012; 6:11–23.
Article2. Wang DY, Chan A, Smith JD. Management of allergic rhinitis: a common part of practice in primary care clinics. Allergy. 2004; 59:315–319.
Article3. Abong JM, Kwong SL, Alava HD, Castor MA, De Leon JC. Prevalence of allergic rhinitis in Filipino adults based on the National Nutrition and Health Survey 2008. Asia Pac Allergy. 2012; 2:129–135.
Article4. Brozek JL, Bousquet J, Baena-Cagnani CE, Bonini S, Canonica GW, Casale TB, van Wijk RG, Ohta K, Zuberbier T, Schunemann HJ. Global Allergy and Asthma European Network. Grading of Recommendations Assessment, Development and Evaluation Working Group. Allergic Rhinitis and its Impact on Asthma (ARIA) guidelines: 2010 revision. J Allergy Clin Immunol. 2010; 126:466–476.5. Bousquet J, Lund VJ, van Cauwenberge P, Bremard-Oury C, Mounedji N, Stevens MT, El-Akkad T. Implementation of guidelines for seasonal allergic rhinitis: a randomized controlled trial. Allergy. 2003; 58:733–741.
Article6. Van Hoecke H, Van Cauwenberge P, Thas O, Watelet JB. The ARIA guidelines in specialist practice: a nationwide survey. Rhinology. 2010; 48:28–34.
Article7. Baldacci S, Maio S, Simoni M, Cerrai S, Sarno G, Silvi P, Di Pede F, Borbotti M, Pala AP, Bresciani M, Viegi G. ARGA study group. The ARGA study with general practitioners: impact of medical education on asthma/rhinitis management. Respir Med. 2012; 106:777–785.
Article8. Prepageran N, Wang de Y, Nair G, Maurer M. The status quo and unmet needs in the management of allergic rhinitis and chronic rhinosinusitis: a Malaysian perspective. Asia Pac Allergy. 2014; 4:142–148.
Article9. Keith PK, Desrosiers M, Laister T, Schellenberg RR, Waserman S. The burden of allergic rhinitis (AR) in Canada: perspectives of physicians and patients. Allergy Asthma Clin Immunol. 2012; 8:7.
Article10. Blaiss MS, Meltzer EO, Derebery MJ, Boyle JM. Patient and healthcare-provider perspectives on the burden of allergic rhinitis. Allergy Asthma Proc. 2007; 28:Suppl 1. S4–S10.
Article11. Meltzer EO, Nathan RA, Derebery J, Dalal AA, Stanford RH, Corrao MA, McMorris BJ. Physician perceptions of the treatment and management of allergic and nonallergic rhinitis. Allergy Asthma Proc. 2009; 30:75–83.
Article12. Wang de Y. Management of allergic rhinitis in general practitioners. Asia Pac Allergy. 2012; 2:233–236.
Article13. Pawankar R, Bunnag C, Khaltaev N, Bousquet J. Allergic Rhinitis and Its Impact on Asthma in Asia Pacific and the ARIA Update 2008. World Allergy Organ J. 2012; 5:Suppl 3. S212–S217.
Article14. Costa DJ, Bousquet PJ, Ryan D, Price D, Demoly P, Brozek J, Schunemann HJ, Bousquet J. Guidelines for allergic rhinitis need to be used in primary care. Prim Care Respir J. 2009; 18:250–257.
Article15. O'Neil KM, Addrizzo-Harris DJ. American College of Chest Physicians Health and Science Policy Committee. Continuing medical education effect on physician knowledge application and psychomotor skills: effectiveness of continuing medical education: American College of Chest Physicians Evidence-Based Educational Guidelines. Chest. 2009; 135:3 Suppl. 37S–41S.16. Blaiss MS, Fromer LM, Jacob-Nara JA, Long RM, Mannion KM, Lauersen LA. Current Allergic Rhinitis Experiences Survey (CARES): Healthcare practitioners' awareness, attitudes and practices. Allergy Asthma Proc. 2014; 35:316–322.
Article17. Quillen DM, Feller DB. Diagnosing rhinitis: allergic vs. nonallergic. Am Fam Physician. 2006; 73:1583–1590.18. Baena-Cagnani CE, Canonica GW, Zaky Helal M, Gomez RM, Compalati E, Zernotti ME, Sanchez-Borges M, Morato Castro FF, Murrieta Aguttes M, Lopez-Garcia A, Tadros FA. ISMAR Study Group. The international survey on the management of allergic rhinitis by physicians and patients (ISMAR). World Allergy Organ J. 2015; 8:10.
Article19. Ball D, Tisocki K. Medicines price components in the Philippines. Amsterdam (PH): Health Action International;2009.20. Mainardi T, Kapoor S, Bielory L. Complementary and alternative medicine: herbs, phytochemicals and vitamins and their immunologic effects. J Allergy Clin Immunol. 2009; 123:283–294.
Article21. Hermelingmeier KE, Weber RK, Hellmich M, Heubach CP, Mosges R. Nasal irrigation as an adjunctive treatment in allergic rhinitis: a systematic review and meta-analysis. Am J Rhinol Allergy. 2012; 26:e119–e125.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Attitudes, practices on allergic rhinitis of three socioeconomic classes of Filipinos in the National Capital Region
- The status quo and unmet needs in the management of allergic rhinitis and chronic rhinosinusitis: a Malaysian perspective
- Diagnosis of Allergic Rhinitis
- Allergic Rhinitis Mouse Model
- Allergic Rhinitis and Sleep-disordered Breathing