J Korean Neurosurg Soc.
2017 Nov;60(6):667-675. 10.3340/jkns.2017.0404.002.
Resection and Observation for Brain Metastasis without Prompt Postoperative Radiation Therapy
- Affiliations
-
- 1Brain Tumor Clinic & Gamma Knife Center, Department of Neurosurgery, Chonnam National University Hwasun Hospital, Chonnam National University Medical School, Hwasun, Korea. kiy87@hanmail.net
- 2Department of Neurosurgery, Chonnam National University Hospital, Chonnam National University Medical School, Gwangju, Korea.
- KMID: 2395786
- DOI: http://doi.org/10.3340/jkns.2017.0404.002
Abstract
OBJECTIVE
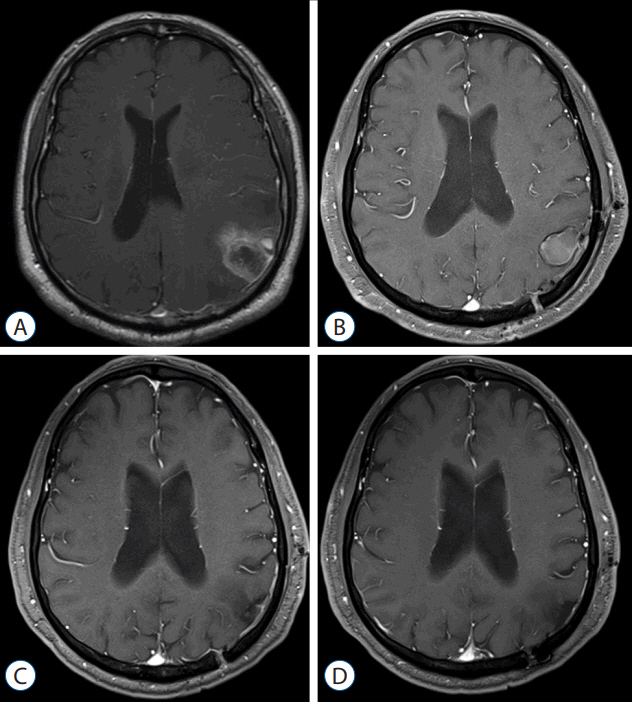
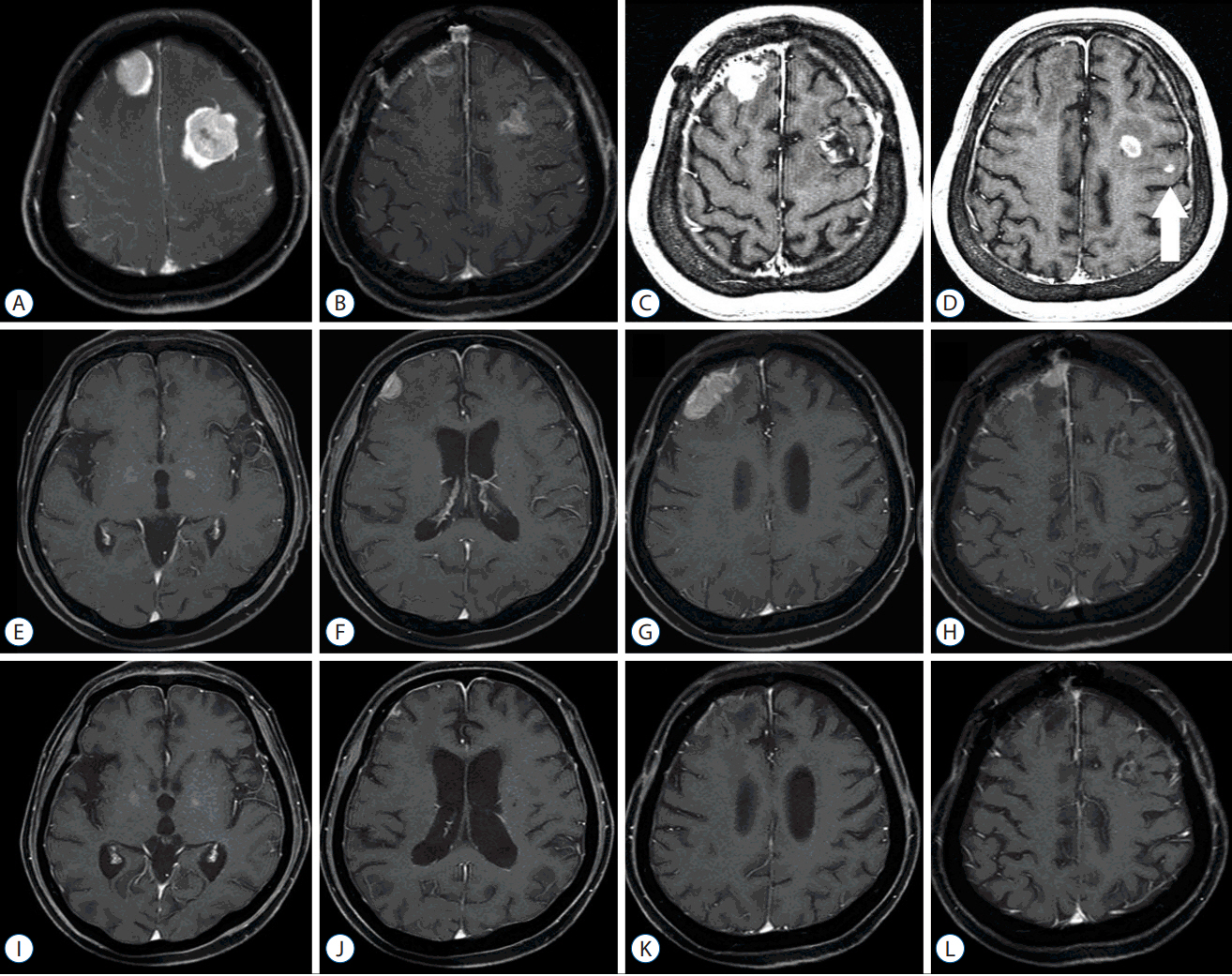
Total resection without consecutive postoperative whole brain radiation therapy is indicated for patients with a single or two sites of brain metastasis, with close follow-up by serial magnetic resonance imaging (MRI). In this study, we explored the effectiveness, usefulness, and safety of this follow-up regimen.
METHODS
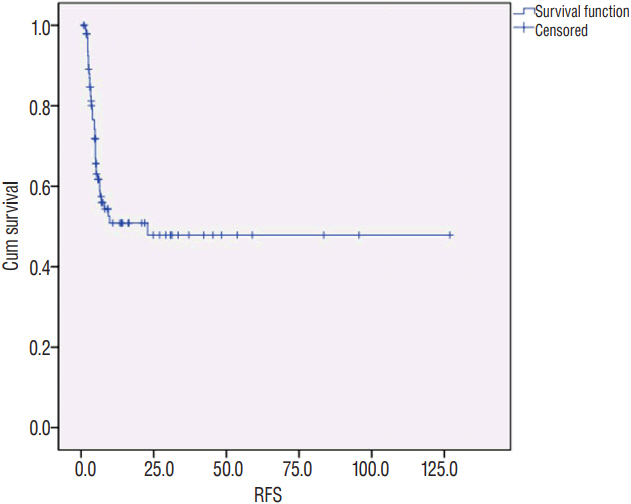
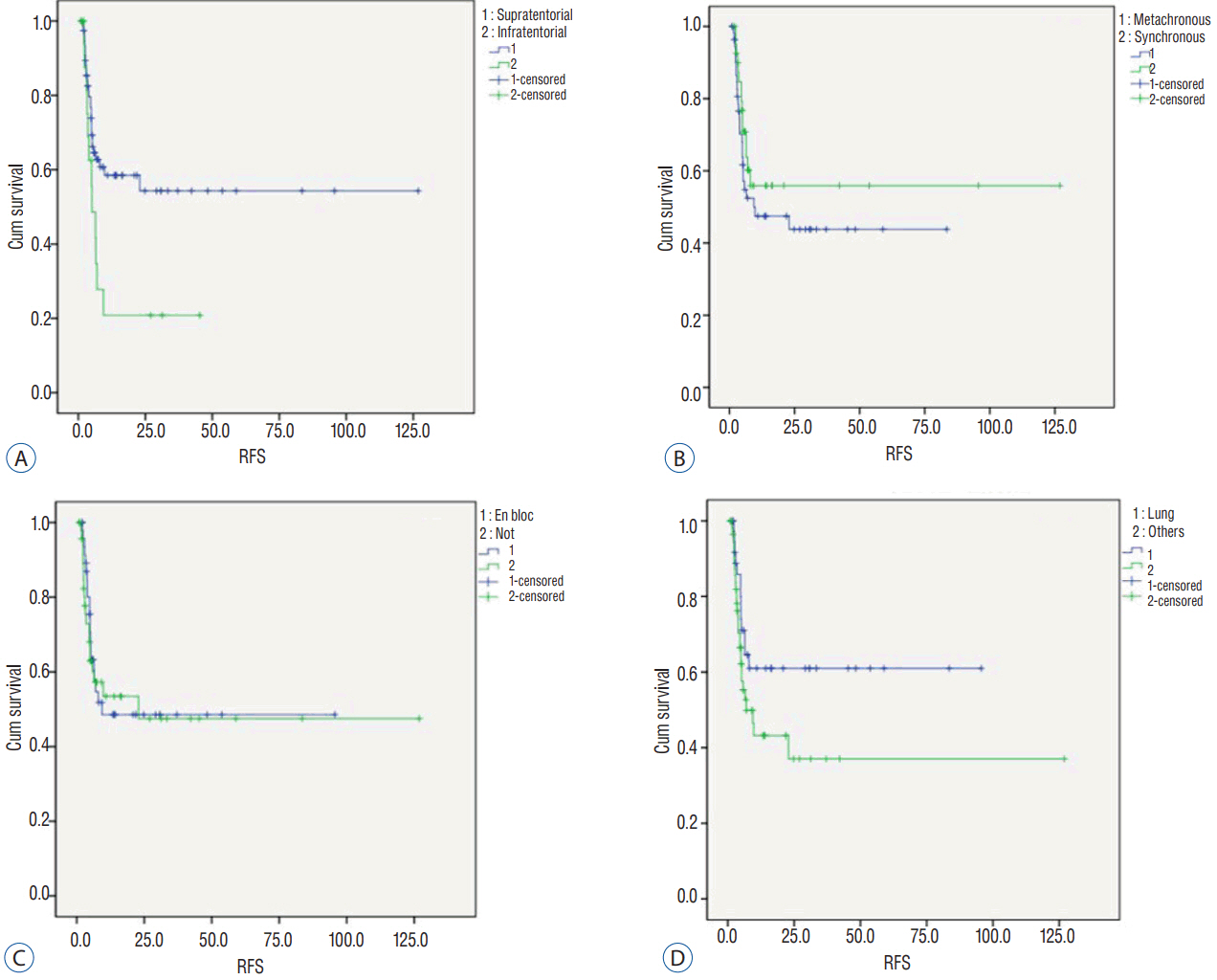
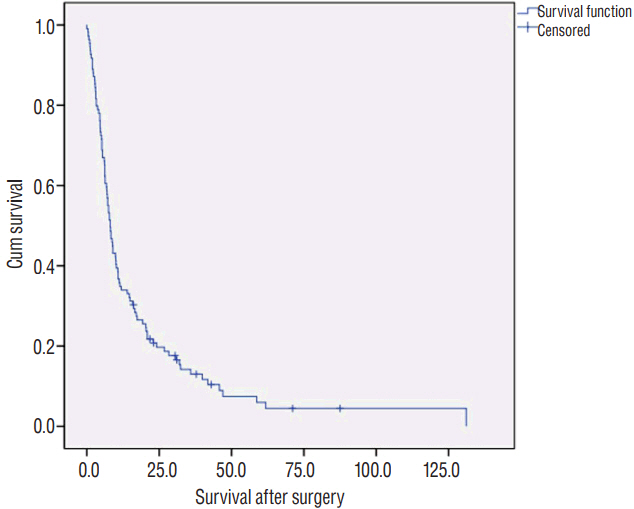
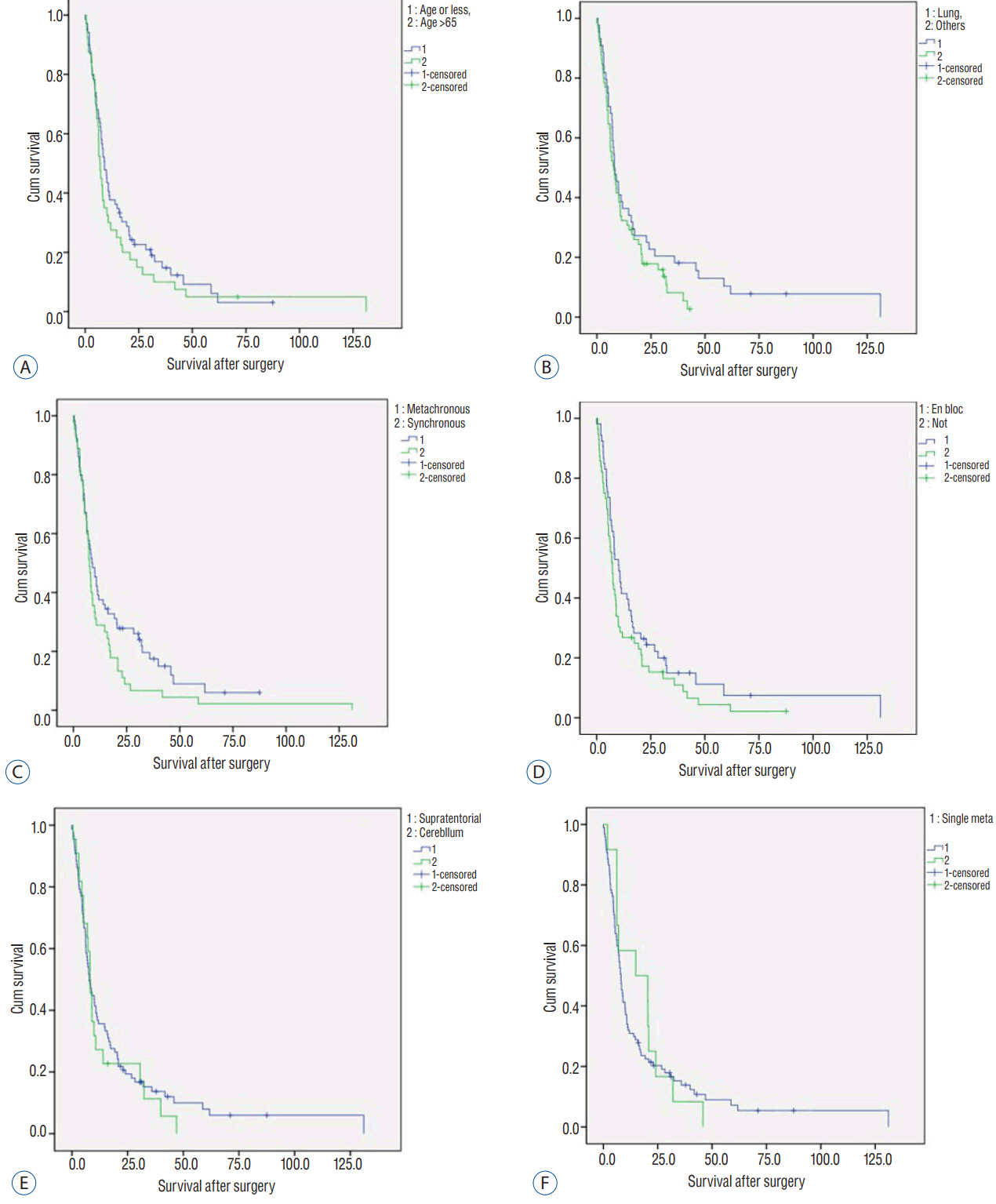
From January 2006 to December 2015, a total of 109 patients (76 males, 33 females) underwent tumor resection as the first treatment for brain metastases (97 patients with single metastases, 12 with two metastases). The mean age was 59.8 years (range 27-80). The location of the 121 tumors in the 109 patients was supratentorial (n=98) and in the cerebellum (n=23). The origin of the primary cancers was lung (n=45), breast (n=17), gastrointestinal tract (n=18), hepatobiliary system (n=8), kidney (n=7), others (n=11), and unknown origin (n=3). The 121 tumors were totally resected. Follow-up involved regular clinical and MRI assessments. Recurrence-free survival (RFS) and overall survival (OS) after tumor resection were analyzed by Kaplan-Meier methods based on clinical prognostic factors.
RESULTS
During the follow-up, MRI scans were done for 85 patients (78%) with 97 tumors. Fifty-six of the 97 tumors showed no recurrence without adjuvant local treatment, representing a numerical tumor recurrence-free rate of 57.7%. Mean and median RFS was 13.6 and 5.3 months, respectively. Kaplan-Meier analysis revealed the cerebellar location of the tumor as the only statistically significant prognostic factor related to RFS (p=0.020). Mean and median OS was 15.2 and 8.1 months, respectively. There were no significant prognostic factors related to OS. The survival rate at one year was 8.2% (9 of 109).
CONCLUSION
With close and regular clinical and image follow-up, initial postoperative observation without prompt postoperative radiation therapy can be applied in patients of brain metastasi(e)s when both the tumor(s) are completely resected.
Keyword
MeSH Terms
Figure
Reference
-
References
1. Aoyama H, Shirato H, Tago M, Nakagawa K, Toyoda T, Hatano K, et al. Stereotactic radiosurgery plus whole-brain radiation therapy vs stereotactic radiosurgery alone for treatment of brain metastases: a randomized controlled trial. JAMA. 295:2483–2491. 2006.
Article2. Barker FG 2nd. Craniotomy for the resection of metastatic brain tumors in the U.S., 1988–2000: decreasing mortality and the effect of provider caseload. Cancer. 100:999–1007. 2004.
Article3. Brown PD, Jaeckle K, Ballman KV, Farace E, Cerhan JH, Anderson SK, et al. Effect of radiosurgery alone vs radiosurgery with whole brain radiation therapy on cognitive function in patients with 1 to 3 brain metastases: a randomized clinical trial. JAMA. 316:401–409. 2016.
Article4. Chang EL, Wefel JS, Hess KR, Allen PK, Lang FF, Kornguth DG, et al. Neurocognition in patients with brain metastases treated with radiosurgery or radiosurgery plus whole-brain irradiation: a randomised controlled trial. Lancet Oncol. 10:1037–1044. 2009.
Article5. Do L, Pezner R, Radany E, Liu A, Staud C, Badie B. Resection followed by stereotactic radiosurgery to resection cavity for intracranial metastases. Int J Radiat Oncol Biol Phys. 73:486–491. 2009.
Article6. Jagannathan J, Yen CP, Ray DK, Schlesinger D, Oskouian RJ, Pouratian N, et al. Gamma knife radiosurgery to the surgical cavity following resection of brain metastases. J Neurosurg. 111:431–438. 2009.
Article7. Karlovits BJ, Quigley MR, Karlovits SM, Miller L, Johnson M, Gayou O, et al. Stereotactic radiosurgery boost to the resection bed for oligometastatic brain disease: challenging the tradition of adjuvant whole-brain radiotherapy. Neurosurg Focus. 27:E7. 20009.
Article8. Kim PK, Ellis TL, Stieber VW, McMullen KP, Shaw EG, McCoy TP, et al. Gamma knife surgery targeting the resection cavity of brain metastasis that has progressed after whole-brain radiotherapy. J Neurosurg. 105(Suppl):75–78. 2006.
Article9. Kocher M, Soffietti R, Abacioglu U, Villà S, Fauchon F, Baumert BG, et al. Adjuvant whole-brain radiotherapy versus observation after radiosurgery or surgical resection of one to three cerebral metastases: results of the EORTC 22952–26001 study. J Clin Oncol. 29:134–141. 2011.
Article10. Laukkanen E, Klonoff H, Allan B, Graeb D, Murray N. The role of prophylactic brain irradiation in limited stage small cell lung cancer: clinical, neuropsychologic, and CT sequelae. Int J Radiat Oncol Biol Phys. 14:1109–1117. 1988.
Article11. Modha A, Shepard SR, Gutin PH. Surgery of brain metastases--is there still a place for it? J Neurooncol. 75:21–29. 2005.
Article12. Mut M. Surgical treatment of brain metastasis: a review. Clin Neurol Neurosurg. 114:1–8. 2012.
Article13. Nataf F, Schlienger M, Liu Z, Foulquier JN, Grès B, Orthuon A, et al. Radiosurgery with or without a 2-mm margin for 93 single brain metastases. Int J Radiat Oncol Biol Phys. 70:766–772. 2008.
Article14. Patchell RA, Tibbs PA, Walsh JW, Dempsey RJ, Maruyama Y, Kryscio RJ, et al. A randomized trial of surgery in the treatment of single metastases to the brain. N Engl J Med. 322:494–500. 1990.
Article15. Saad S, Wang TJ. Neurocognitive deficits after radiation therapy for brain malignancies. Am J Clin Oncol. 38:634–640. 2015.
Article16. Soltys SG, Adler JR, Lipani JD, Jackson PS, Choi CY, Puataweepong P, et al. Stereotactic radiosurgery of the postoperative resection cavity for brain metastases. Int J Radiat Oncol Biol Phys. 70:187–193. 2008.
Article17. Sunderland GJ, Jenkinson MD, Zakaria R. Surgical management of posterior fossa metastases. J Neurooncol. 130:535–542. 2016.
Article18. Vogelbaum MA, Suh JH. Resectable brain metastases. J Clin Oncol. 24:1289–1294. 2006.
Article19. Yoo H, Kim YZ, Nam BH, Shin SH, Yang HS, Lee JS, et al. Reduced local recurrence of a single brain metastasis through microscopic total resection. J Neurosurg. 110:730–736. 2009.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Long Term Survival in Patient with Hepatocellular Carcinoma after Surgical Resection of Brain Metastasis: A Case Report
- Secondary Mania after Postoperative Radiation Therapy for Primary Brain Tumor
- Role of Radiation Therapy in the Treatment of Brain Metastases
- Postoperative Radiation Therapy of Astrocytoma and Glioblastoma Multiforme
- A Retrospective Analysis of Treatment and Prognosis in Brain Metastases