Clin Exp Otorhinolaryngol.
2017 Sep;10(3):228-235. 10.21053/ceo.2016.00612.
Analysis of Prognostic Factors in Malignant External Otitis
- Affiliations
-
- 1Department of Otorhinolaryngology-Head and Neck Surgery, Soonchunhyang University College of Medicine, Bucheon, Korea. bgkim@schmc.ac.kr
- 2Department of Otorhinolaryngology, Yonsei University College of Medicine, Seoul, Korea.
- KMID: 2395736
- DOI: http://doi.org/10.21053/ceo.2016.00612
Abstract
OBJECTIVES
Malignant external otitis (MEO) is a potentially fatal infection of the external auditory canal, temporal bone, and skull base. Despite treatment with modern antibiotics, MEO can lead to skull base osteomyelitis. Until now, there have been few studies on the prognostic factors of MEO.
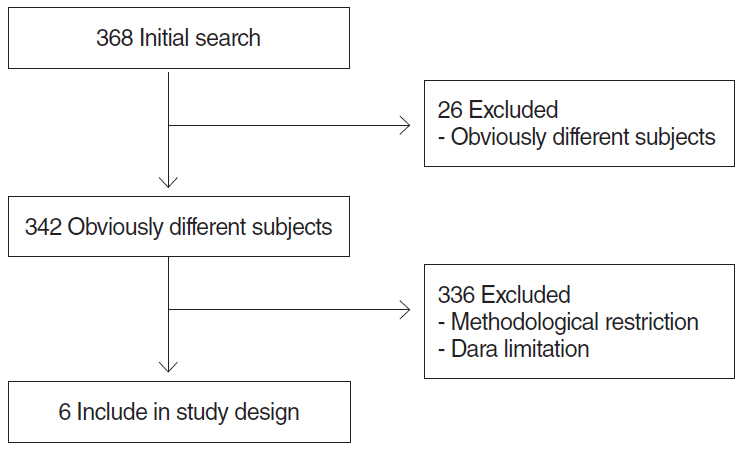
METHODS
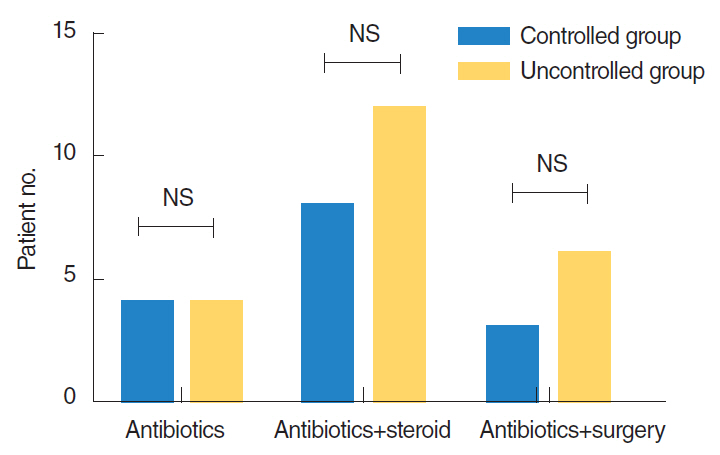
We performed a retrospective study to identify prognostic factors of MEO, and a meta-analysis of other articles investigating MEO. On the basis of disease progression the 28 patients in our study were divided into "˜controlled' and "˜uncontrolled' groups, consisting of 12 and 16 patients, respectively. We identified three categories of prognostic factors: those related to patient, disease, and treatment. We compared these prognostic factors between the controlled and uncontrolled groups.
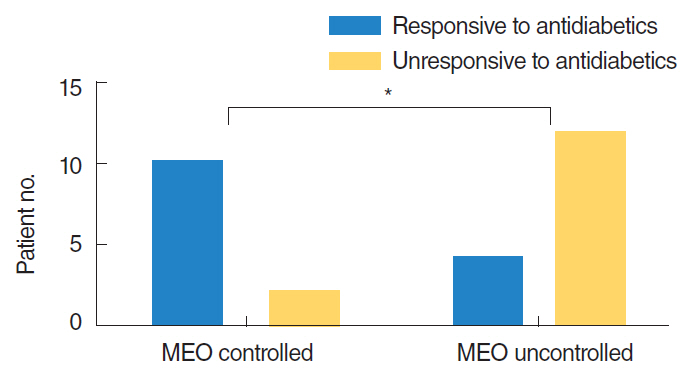
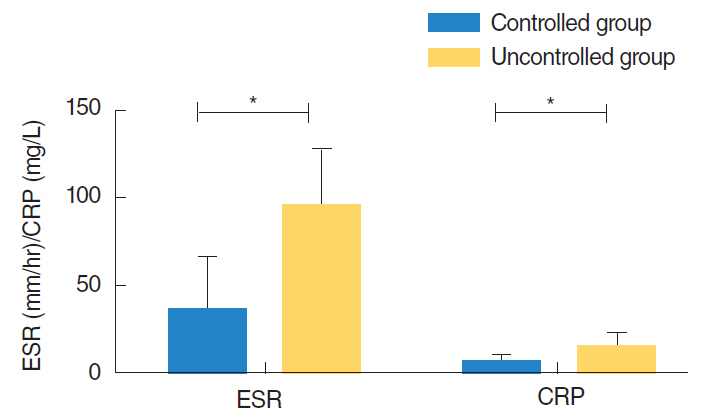
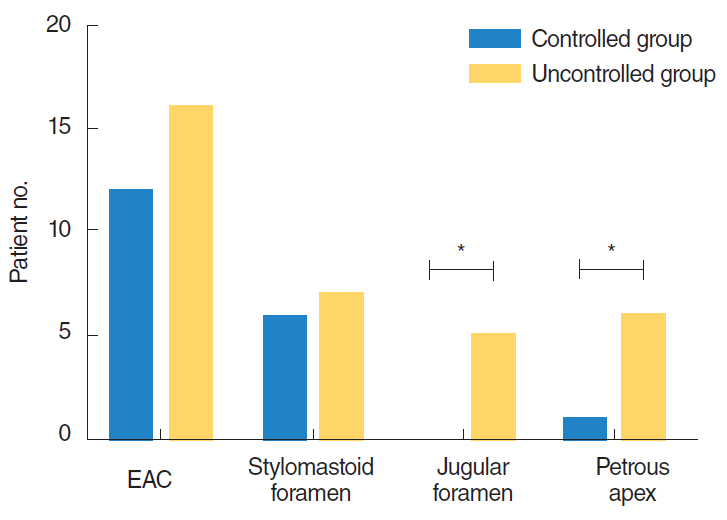
RESULTS
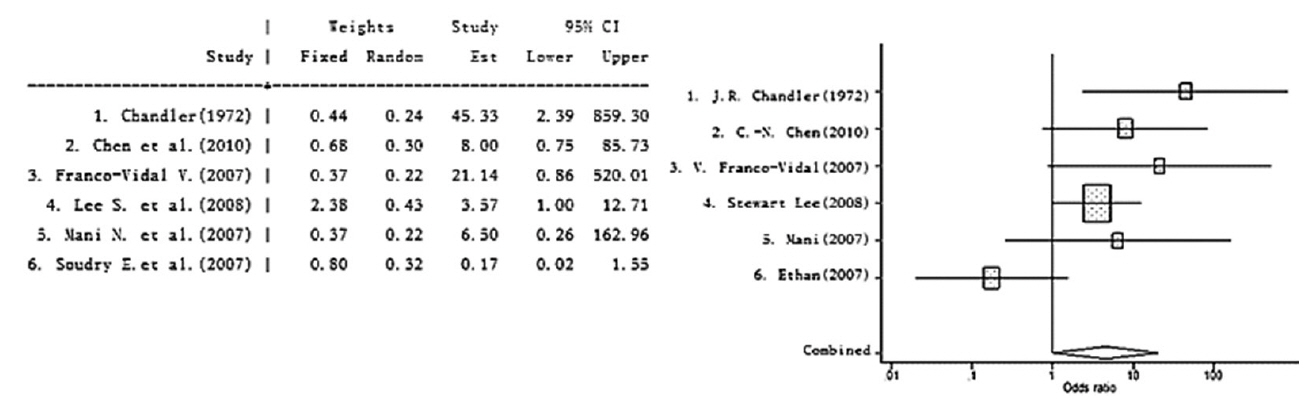
In our study, the duration of diabetes mellitus (DM), presence of inflammatory markers (C-reactive protein and erythrocyte sedimentation rate), and computed tomography or magnetic resonance imaging findings influenced the prognosis of MEO. In contrast, prognosis was unrelated to age, gender, mean glucose level, hemoglobin A1c level, pathogen, comorbidity, or cranial nerve involvement. No factor related to treatment modality was correlated with prognosis, such as surgery, steroid therapy, or interval to the first appropriate treatment. Cranial nerve involvement has been proven to be associated with disease progression, but the relationship between cranial nerve involvement and the prognosis of MEO remains controversial. As a part of this study, we conducted a meta-analysis of cranial nerve involvement as a prognostic factor of MEO. We found that cranial nerve involvement has a statistically significant influence on the prognosis of MEO.
CONCLUSION
We found that glycemic control in diabetes mellitus, cranial nerve involvement, and the extent of disease determined from various imaging modalities influence the prognosis of MEO. We suggest that significant prognostic factors should be monitored to determine the prognosis of patients with MEO.
Keyword
MeSH Terms
Figure
Reference
-
1. Rubin J, Yu VL. Malignant external otitis: insights into pathogenesis, clinical manifestations, diagnosis, and therapy. Am J Med. 1988; Sep. 85(3):391–8.
Article2. Chandler JR. Malignant external otitis and facial paralysis. Otolaryngol Clin North Am. 1974; Jun. 7(2):375–83.
Article3. Nadol JB Jr. Histopathology of Pseudomonas osteomyelitis of the temporal bone starting as malignant external otitis. Am J Otolaryngol. 1980; Nov. 1(5):359–71.
Article4. Rowlands RG, Lekakis GK, Hinton AE. Masked pseudomonal skull base osteomyelitis presenting with a bilateral Xth cranial nerve palsy. J Laryngol Otol. 2002; Jul. 116(7):556–8.
Article5. Mani N, Sudhoff H, Rajagopal S, Moffat D, Axon PR. Cranial nerve involvement in malignant external otitis: implications for clinical outcome. Laryngoscope. 2007; May. 117(5):907–10.
Article6. Soudry E, Joshua BZ, Sulkes J, Nageris BI. Characteristics and prognosis of malignant external otitis with facial paralysis. Arch Otolaryngol Head Neck Surg. 2007; Oct. 133(10):1002–4.
Article7. Cohen D, Friedman P. The diagnostic criteria of malignant external otitis. J Laryngol Otol. 1987; Mar. 101(3):216–21.
Article8. Ali T, Meade K, Anari S, ElBadawey MR, Zammit-Maempel I. Malignant otitis externa: case series. J Laryngol Otol. 2010; Aug. 124(8):846–51.
Article9. Lee S, Hooper R, Fuller A, Turlakow A, Cousins V, Nouraei R. Otogenic cranial base osteomyelitis: a proposed prognosis-based system for disease classification. Otol Neurotol. 2008; Aug. 29(5):666–72.10. Franco-Vidal V, Blanchet H, Bebear C, Dutronc H, Darrouzet V. Necrotizing external otitis: a report of 46 cases. Otol Neurotol. 2007; Sep. 28(6):771–3.11. Chen CN, Chen YS, Yeh TH, Hsu CJ, Tseng FY. Outcomes of malignant external otitis: survival vs mortality. Acta Otolaryngol. 2010; 130(1):89–94.
Article12. Chandler JR. Malignant external otitis. Laryngoscope. 1968; Aug. 78(8):1257–94.
Article13. Joshua BZ, Sulkes J, Raveh E, Bishara J, Nageris BI. Predicting outcome of malignant external otitis. Otol Neurotol. 2008; Apr. 29(3):339–43.
Article14. Geerlings SE, Hoepelman AI. Immune dysfunction in patients with diabetes mellitus (DM). FEMS Immunol Med Microbiol. 1999; Dec. 26(3-4):259–65.
Article15. O’Sullivan TJ, Dickson RI, Blokmanis A, Roberts FJ, Kaan K. The pathogenesis, differential diagnosis, and treatment of malignant otitis externa. J Otolaryngol. 1978; Aug. 7(4):297–303.16. Lucente FE, Parisier SC, Som PM, Arnold LM. Malignant external otitis: a dangerous misnomer? Otolaryngol Head Neck Surg. 1982; Mar-Apr. 90(2):266–9.
Article17. Lucente FE, Parisier SC, Som PM. Complications of the treatment of malignant external otitis. Laryngoscope. 1983; Mar. 93(3):279–81.
Article18. Bernheim J, Sade J. Histopathology of the soft parts in 50 patients with malignant external otitis. J Laryngol Otol. 1989; Apr. 103(4):366–8.
Article19. Sudhoff H, Rajagopal S, Mani N, Moumoulidis I, Axon PR, Moffat D. Usefulness of CT scans in malignant external otitis: effective tool for the diagnosis, but of limited value in predicting outcome. Eur Arch Otorhinolaryngol. 2008; Jan. 265(1):53–6.
Article20. Kondziella D, Skagervik I. Malignant external otitis with extensive cranial neuropathy but no facial paralysis. J Neurol. 2007; Sep. 254(9):1298–9.
Article21. Stokkel MP, Takes RP, van Eck-Smit BL, Baatenburg de Jong RJ. The value of quantitative gallium-67 single-photon emission tomography in the clinical management of malignant external otitis. Eur J Nucl Med. 1997; Nov. 24(11):1429–32.
Article22. Okpala NC, Siraj QH, Nilssen E, Pringle M. Radiological and radionuclide investigation of malignant otitis externa. J Laryngol Otol. 2005; Jan. 119(1):71–5.
Article23. Stevens SM, Lambert PR. Mastoidectomy: surgical techniques. In : Flint PW, Haughey BH, Lund VJ, Niparko JK, Robbins KT, Thomas JR, editors. Cummings otolaryngology: head and neck surgery. 6th ed. Philadelphia (PA): Elsevier Saunders;2015. p. 2188–99.24. Brant JA, Ruckenstein MJ. Infections of the external ear. In : Flint PW, Haughey BH, Lund VJ, Niparko JK, Robbins KT, Thomas JR, editors. Cummings otolaryngology: head and neck surgery. 6th ed. Philadelphia (PA): Elsevier Saunders;2015. p. 2115–22.25. Walvekar RR, Culicchia F, Nuss DW. Surgery of the anterior and middle cranial base. In : Flint PW, Haughey BH, Lund VJ, Niparko JK, Robbins KT, Thomas JR, editors. Cummings otolaryngology: head and neck surgery. 6th ed. Philadelphia (PA): Elsevier Saunders;2015. p. 2671–700.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The preoperative prognostic factors in chronic otitis media
- Skin Prick Test Reactivity in Patients with Chronic Eczematous External Otitis
- A case of malignant external otitis using scintigraphic study
- A clinical study on the prognostic factors of tympanoplasty usingpostoperative tympanogram in chronic otitis media
- Temporomandibular joint involvement in malignant otitis externa: a case report