J Korean Med Assoc.
2008 Mar;51(3):244-252.
Excessive Daytime Sleepiness
- Affiliations
-
- 1Department of Psychiatry, The Catholic University of Korea College of Medicine, Korea. hscjohn@hotmail.com
Abstract
- Excessive daytime sleepiness (EDS) is a prevalent complaint among patients in psychiatric and medical care. Patients with EDS have often been misdiagnosed with depression due to their complaints of lack of energy and poor concentration. Also, they have even been diagnosed erroneously with a psychotic disorder in case of coexistence with hypnagogic hallucination. EDS can seriously affect the person's quality of life by causing decreased academic achievement or work performance, low self esteem, and social withdrawal. EDS is also frequently associated with various medical and psychiatric conditions, and often fatal traffic or on-the-job accidents. The causes of EDS range from insufficient sleep to central nervous system-originated hypersomnia. The conditions that can lead to EDS include circadian rhythm disorders, primary disorders of alertness such as narcolepsy, sleep-related breathing disorders such as obstructive sleep apnea syndrome, sleep-related movement disorders such as periodic limb movement disorder and restless legs syndrome, chronic medical conditions such as cancer, and medications causing sleepiness. Treatment options should be tailored according to the underlying condition and include sufficient sleep time, light therapy, sleep scheduling, wakefulness-promoting medications, or mechanical airway managements such as nasal continuous positive airway pressure (CPAP).
MeSH Terms
-
Achievement
Chronobiology Disorders
Continuous Positive Airway Pressure
Depression
Diagnosis, Differential
Disorders of Excessive Somnolence
Hallucinations
Humans
Movement Disorders
Narcolepsy
Nocturnal Myoclonus Syndrome
Phototherapy
Psychotic Disorders
Quality of Life
Respiration
Restless Legs Syndrome
Self Concept
Sleep Apnea, Obstructive
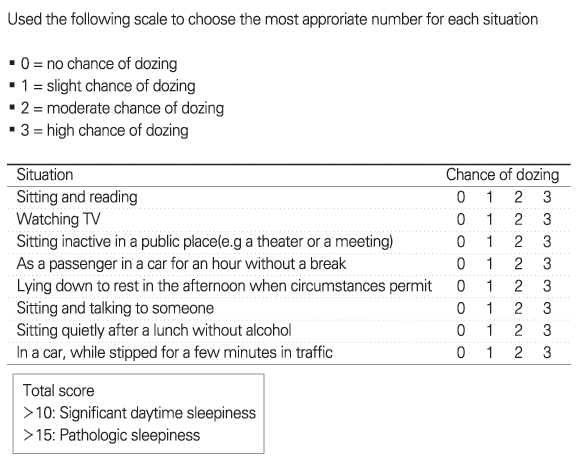
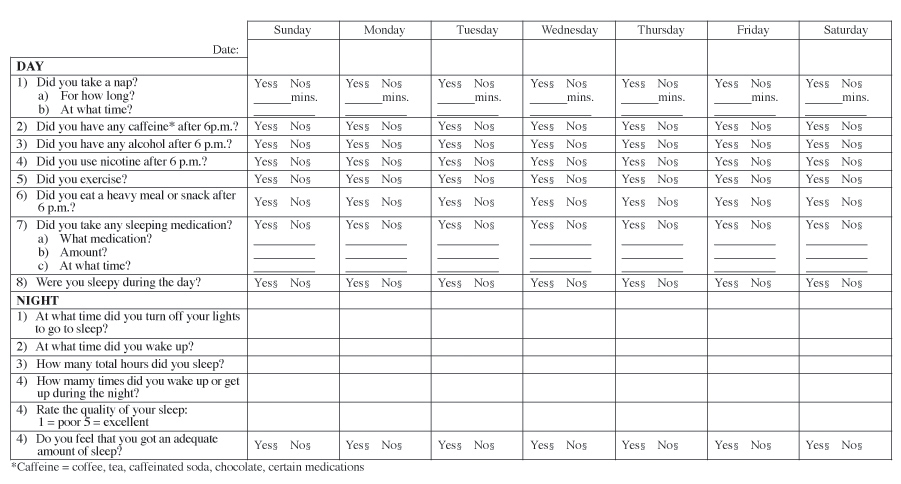
Figure
Reference
-
1. International Classification of Sleep Disorders. Diagnostic and coding manual, revised. 1997. Rochester (MN): American Sleep Disorders Association.2. Ohayon MM, Priest RG, Zulley J, Smirne S, Pavia T. Prevalence of narcolepsy symptomatology and diagnosis in the European general population. Neurology. 2002. 58:1826–1833.
Article3. Sleep in America Poll, 2002. National Sleep Foundation. Available at: http://www.sleepfoundation.org.4. Sleep in America Poll, 2003. National Sleep Foundation. Available at: http://www.sleepfoundation.org.5. Johns MW. A new method of measuring sleepiness: the Epworth sleepiness scale. Sleep. 1991. 14:540–545.6. Hoddes E, Zarcone V, Smythe H, Smythe H, Phillips R, Dement WC. Quantification of sleepiness: a new approach. Psychophysiology. 1973. 10:431–436.
Article7. Rosenthal L, Roehr TA, Roth T. The sleep-wake activity inventory: a self-report measure of daytime sleepiness. Biol Psychiatry. 1993. 34:810–820.
Article8. Richardson G, Carskadon M, Flagg W, Van den Hoed J, Dement WC, Mitler MM. Excessive daytime sleepiness in man: multiple sleep latency measurements in narcoleptic and control subjects. Electroencephalogr Clin Neurophysiol. 1978. 45:621–627.
Article9. Johns MW, Hocking B. Daytime sleepiness and sleep habits of Australian workers. Sleep. 1997. 20:844–849.
Article10. Rechtschaffen A, Kales A, editors. A manual of standardized terminology, techniques and scoring system for sleep stages of human subjects. 1968. Washington D.C.: U.S. Public Health Service, U.S. Government Printing Office.11. Carskadon MA, Dement WC, Mitler MM, Roth T, Westbrook PR, Keenan S. Guidelines for the multiple sleep latency test (MSLT): a standard measure of sleepiness. Sleep. 1986. 9:519–524.
Article12. Thorpy MJ. The Standards of Practice Committee of the American Sleep Disorders Association. The clinical use of the Multiple Sleep Latency Test. Sleep. 1992. 15:268–276.
Article13. American Academy of Sleep Medicine. ICSD-2-International classification of sleep disorders. Diagnostic and coding manual. 2005. 2nd ed. American Academy of Sleep Medicine.14. Banks S, Cacheside P, Lack LC, Gunstein RR, McEvoy RD. The maintenance of wakefulness test and driving simulator performance. Sleep. 2005. 28:1360–1361.
Article15. Park YJ, Lee WC, Lim HW, Park YM. The association between sleep duration and obesity in Korean adults. J Prev Med Public Health. 2007. 40:454–460.
Article16. Roehrs TA, Shore E, Papineau K, Rosenthal L, Roth T. A two-week sleep extension in sleepy normals. Sleep. 1996. 19:576–582.17. Melendres CS, Lutz JM, Rubin ED, Marcus CL. Daytime sleepiness and hyperactivity in children with suspected sleep-disordered breathing. Pediatrics. 2004. 114:768–775.
Article18. Golan N, Shahar E, Ravid S, Pillar G. Sleep disorders and daytime sleepiness in children with attention-deficit/hyperactive disorder. Sleep. 2004. 27:261–266.
Article19. Rosen CL, Storfer-Isser A, Taylor HG, Kirchner HL, Emancipator JL, Redline S. Increased behavioral morbidity in school-aged children with sleep-disordered breathing. Pediatrics. 2004. 114:1640–1648.
Article20. Chervin RD, Archbold KH, Dillon JE, Panahi P, Pituch KJ, Dahl RE, Guilleminault C. Inattention, hyperactivity, and symptoms of sleep-disordered breathing. Pediatrics. 2002. 109:449–456.
Article21. Picchietti DL, England SJ, Walters AS, Willis K, Verrico T. Periodic limb movements disorder and restless legs syndrome in children with attention-deficit hyperactivity disorder. J Child Neurol. 1998. 13:588–594.
Article22. Picchietti DL, Walters AS. Moderate to severe periodic limb movements disorder in childhood and adolescence. Sleep. 1999. 22:297–300.
Article23. Hong SC, Lin Ling, Jeong JH, Han JH, Lee JH, Lee SP, Zhang Jing, Einen Mali, Mignot Emmanuel. A study of the diagnostic utility of HLA-typing, CSF hypocretin-1 measurements and MSLT testing for the diagnosis of narcolepsy in 163 Korean patients with unexplained excessive daytime sleepiness. Sleep. 2006. 29:1429–1438.
Article24. Hong SC, Lin L, Lo B, Jeong JH, Shin YK, Kim SY, Kweon YS, Zhang Jing, Einen Mali, Smith Anajane, Hansen John, Grumet F.Carl, Mignot Emmanuel. DQB1*0301 and DQB10601 modulate narcolepsy susceptibility in Koreans. Human Immunology. 2007. 68:59–68.
Article25. Diagnostic and Statistical Mannual of Mental Disorders: DSM-IV-TR. 2000. 4th ed. Washington (DC): American Psychiatric Association.26. Tylee A, Gastpar M, Lepine JP, Mendlewicz J. DEPRES Steering Committee. DEPRES II (Depression Research in European Society II): a patient survey of the symptoms, disability and current management of depression in the community. Int Clin Psychopharmacol. 1999. 14:139–151.
Article27. Reynolds CF 3rd, Coble PA, Kupfer DJ, Holzer BC. Application of the multiple sleep latency test in disorders of excessive sleepiness. Electroencephalogr Clin Neurophysiol. 1982. 53:443–452.
Article28. Chesson AL Jr, Littner M, Davila D, Anderson WM, Griqq-Damberger M, Hartse K, Johnson S, Wise M. Practice parameters for the use of light therapy in the treatment of sleep disorders. Standards of Practice Committee, American Academy of Sleep Medicine. Sleep. 1999. 22:641–660.
Article29. Czeisler CA. Commentary: evidence for melatonin as a circadian phase-shifting agent. J Biol Rhythms. 1997. 12:618–623.
Article30. Patel SR, White DP, Malhotra A, Stanchina ML, Ayas NT. Continuous positive airway pressure therapy for treating sleepiness in a diverse population with obstructive sleep apnea: results of a meta-analysis. Arch Intern Med. 2003. 163:565–571.
Article31. Morisson F, Decary A, Petit D, Lavigne G, Malo J, Montplaisir J. Daytime sleepiness and EEG spectral analysis in apneic patients before and after treatment with continuous positive airway pressure. Chest. 2001. 119:45–52.
Article32. Allen RP, Early CJ. Restless legs syndrome: a review of clinical and pathophysiologic features. J Clin Neurophysiol. 2001. 18:128–147.33. Allen R, Becker PM, Bogan R, Schmidt M, Kushida CA, Fry JM, Poceta JS, Winslow D. Ropinirole decreases periodic leg movements and improves sleep parameters in patients with restless legs syndrome. Sleep. 2004. 27:907–914.
Article34. Trenwalder C, Garcia-Borreguero D, Montagna P, Lainey E, de Weerd AW, Tidswell P, Saletu-Zyhlarz G, Telstad W, Ferini-Starambi L. Ropinirole in the treatment of restless legs syndrome: results form the TREAT RLS1 study, a 12 week, randomized, placebo controlled study in 10 European countries. J Neurol Neurosurg Psychiatry. 2004. 75:92–97.35. US Xyrem in Narcolepsy Multi-center Study Group. A randomized, double blind, placebocontrolled multicenter trial comparing the effects of three doses of orally administered sodium oxybate with placebo for the treatment of narcolepsy. Sleep. 2002. 25:42–49.36. Mamelak M, Black J, Monplaisir J, Ristanovic R. A pilot study on the effects of sodium oxybate on sleep architecture and daytime alertness in narcolepsy. Sleep. 2004. 27:1327–1334.
Article37. Black J, Houghton WC. Sodium oxybate improves excessive daytime sleepiness in narcolepsy. Sleep. 2006. 29:939–946.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Sleepy Child
- Predictors of Excessive Daytime Sleepiness in Korean Snoring Patients
- Usefulness of Various Questionnaires in the Assessment of Excessive Daytime Sleepiness and Circadian Rhythm
- Exploration of Insomnia With Excessive Daytime Sleepiness From Clinical and Polysomnographic Perspectives
- Analysis of Factors Associated with Daytime Sleepiness in Korean Adolescents