Korean J Neurotrauma.
2017 Oct;13(2):167-170. 10.13004/kjnt.2017.13.2.167.
Posterior Reversible Encephalopathy Syndrome after Head Trauma Surgery in Pediatric Patient without Any Underlying Disease
- Affiliations
-
- 1Department of Neurosurgery, Konyang University Hospital, Konyang University Collge of Medicine, Daejeon, Korea. leecy009@hanmail.net
- KMID: 2394555
- DOI: http://doi.org/10.13004/kjnt.2017.13.2.167
Abstract
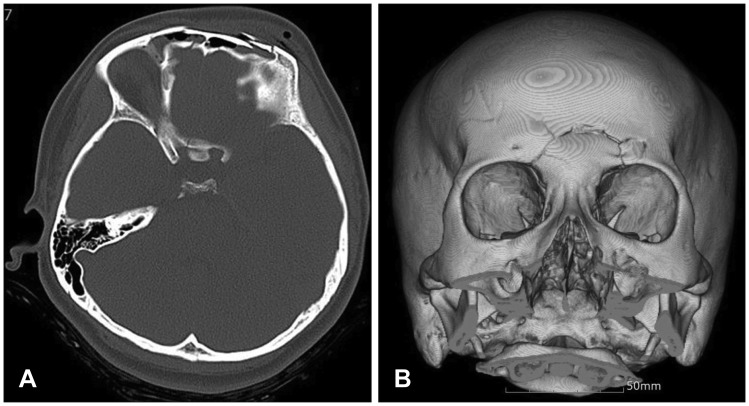
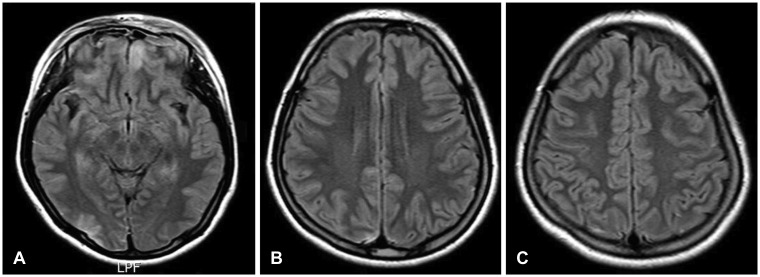
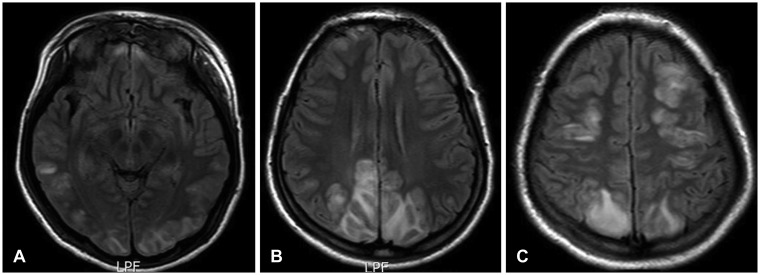
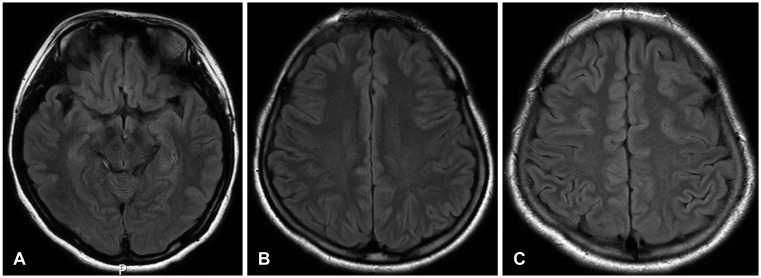
- Posterior reversible encephalopathy syndrome (PRES) is a neurological disorder characterized by signs of posterior cerebral edema upon radiographic examination. A 16-year-old girl was involved in motorcycle accident and depressed frontal fracture was presented. She had generalized seizures 3 days after dural repair and fracture reduction. Signal changes was noted on both parietal lobes in the magnetic resonance images and it was completely resolved in 3 months follow-up. We would like to present the case that demonstrated PRES related hypertension after head trauma surgery for cerebrospinal fluid leakage in pediatric patient without any underlying disease.
MeSH Terms
Figure
Reference
-
1. Bartynski WS, Boardman JF. Distinct imaging patterns and lesion distribution in posterior reversible encephalopathy syndrome. AJNR Am J Neuroradiol. 2007; 28:1320–1327. PMID: 17698535.
Article2. Feil K, Forbrig R, Thaler FS, Conrad J, Heck S, Dorn F, et al. Reversible cerebral vasoconstriction syndrome and posterior reversible encephalopathy syndrome associated with intracranial hypotension. Neurocrit Care. 2017; 26:103–108. PMID: 27848124.
Article3. Girişgen I, Tosun A, Sönmez F, Ozsunar Y. Recurrent and atypical posterior reversible encephalopathy syndrome in a child with peritoneal dialysis. Turk J Pediatr. 2010; 52:416–419. PMID: 21043390.4. Hammad T, DeDent A, Algahtani R, Alastal Y, Elmer L. Posterior reversible encephalopathy syndrome secondary to CSF leak and intracranial hypotension: a case report and literature review. Case Rep Neurol Med. 2015; 2015:538523. PMID: 26106495.
Article5. Hinchey J, Chaves C, Appignani B, Breen J, Pao L, Wang A, et al. A reversible posterior leukoencephalopathy syndrome. N Engl J Med. 1996; 334:494–500. PMID: 8559202.
Article6. Jones BV, Egelhoff JC, Patterson RJ. Hypertensive encephalopathy in children. AJNR Am J Neuroradiol. 1997; 18:101–106. PMID: 9010526.7. Koichihara R, Hamano S, Yamashita S, Tanaka M. Posterior reversible encephalopathy syndrome associated with IVIG in a patient with Guillain-Barre syndrome. Pediatr Neurol. 2008; 39:123–125. PMID: 18639758.8. Kwon S, Koo J, Lee S. Clinical spectrum of reversible posterior leukoencephalopathy syndrome. Pediatr Neurol. 2001; 24:361–364. PMID: 11516610.
Article9. McCoy B, King M, Gill D, Twomey E. Childhood posterior reversible encephalopathy syndrome. Eur J Paediatr Neurol. 2011; 15:91–94. PMID: 21074464.
Article10. McKinney AM, Short J, Truwit CL, McKinney ZJ, Kozak OS, SantaCruz KS, et al. incidence of atypical regions of involvement and imaging findings. AJR Am J Roentgenol. 2007; 189:904–912. PMID: 17885064.11. Mirza A. Posterior reversible encephalopathy syndrome: a variant of hypertensive encephalopathy. J Clin Neurosci. 2006; 13:590–595. PMID: 16769518.
Article12. Onder AM, Lopez R, Teomete U, Francoeur D, Bhatia R, Knowbi O, et al. Posterior reversible encephalopathy syndrome in the pediatric renal population. Pediatr Nephrol. 2007; 22:1921–1929. PMID: 17694337.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Posterior reversible encephalopathy syndrome and reversible cerebral vasoconstriction syndrome associated with acute exacerbation of chronic obstructive pulmonary disease
- Central-variant Posterior Reversible Encephalopathy Syndrome after Head Trauma
- Posterior Reversible Encephalopathy Syndrome in a Patient with Intoxication of Arisaema amurense
- A Case of Posterior Reversible Encephalopathy Syndrome in a Patient having Continuous Ambulatory Peritoneal Dialysis
- Posterior Reversible Encephalopathy Syndrome