J Rheum Dis.
2017 Oct;24(5):303-308. 10.4078/jrd.2017.24.5.303.
Focal Eosinophilic Myositis Associated with Behçet's Disease
- Affiliations
-
- 1Division of Rheumatology, Department of Internal Medicine, Kyungpook National University School of Medicine, Daegu, Korea. ejnam@knu.ac.kr
- 2Division of Rheumatology, Department of Internal Medicine, Changwon Fatima Hospital, Changwon, Korea.
- 3Department of Pathology, Kyungpook National University School of Medicine, Daegu, Korea.
- KMID: 2394346
- DOI: http://doi.org/10.4078/jrd.2017.24.5.303
Abstract
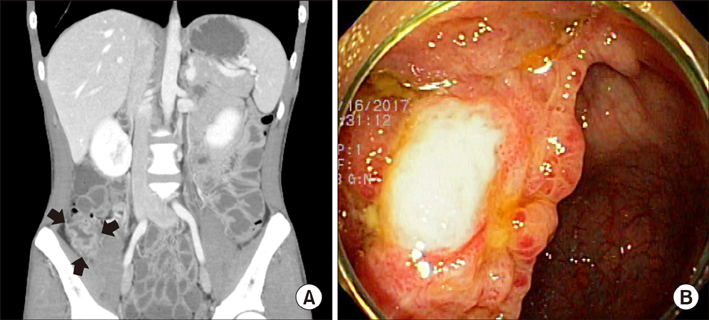
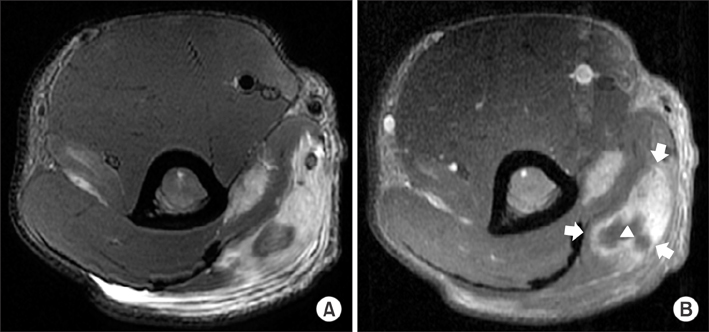
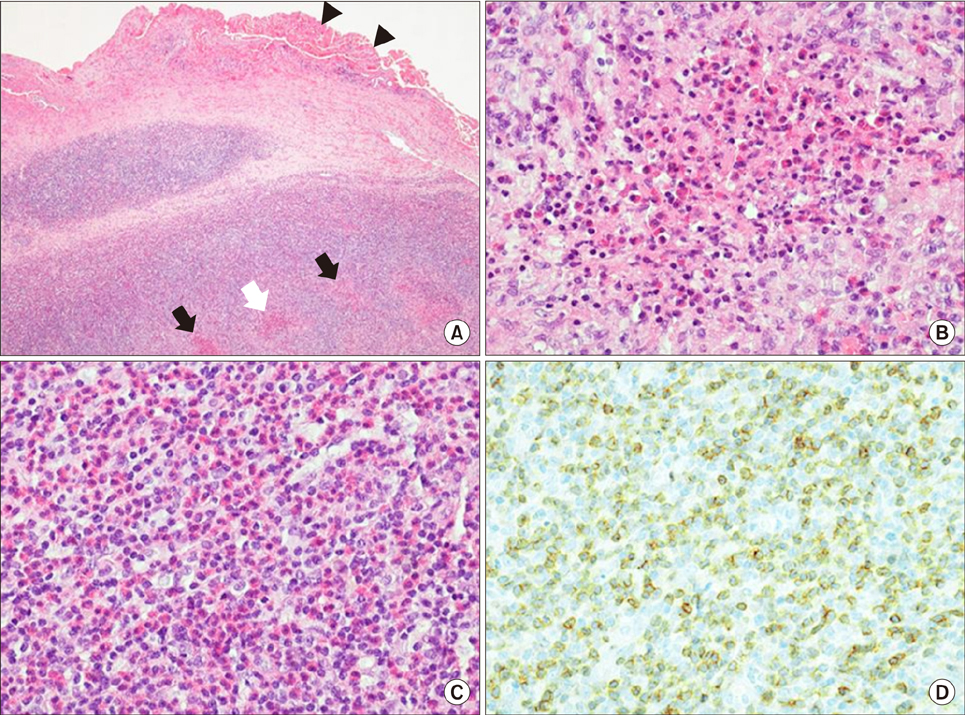
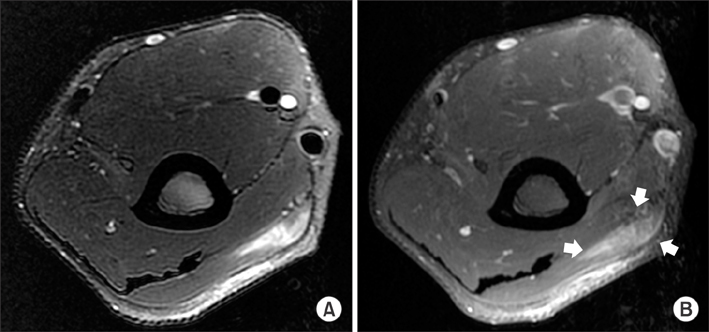
- Behçet's disease (BD) is a systemic vasculitis commonly accompanied by recurrent mucosal ulceration and other systemic manifestations, but rarely by myositis. Focal eosinophilic myositis is the most limited idiopathic eosinophilic myopathy characterized by peripheral blood eosinophilia and/or eosinophilic muscle infiltration. Clinical manifestations include myalgia, muscle weakness, and cutaneous lesions, such as subcutaneous induration and erythema. Given that BD can mimic deep vein thrombosis or pseudotumor, muscle biopsy should be performed to enhance the accuracy of diagnosis. Microscopic examination reveals extensive infiltration of eosinophils and mononuclear cells into muscle, myofiber necrosis, and regeneration. To the best of our knowledge, there have not been any published reports on MEDLINE regarding focal eosinophilic myositis associated with BD. Here, we presented a case of focal eosinophilic myositis associated with intestinal BD in a 23-year-old man who suffered from a large ulcer in the terminal ileum.
MeSH Terms
Figure
Reference
-
1. Sakane T, Takeno M, Suzuki N, Inaba G. Behçet's disease. N Engl J Med. 1999; 341:1284–1291.2. Skef W, Hamilton MJ, Arayssi T. Gastrointestinal Behçet's disease: a review. World J Gastroenterol. 2015; 21:3801–3812.3. Zou J, Shen Y, Ji DN, Zheng SB, Guan JL. Endoscopic findings of gastrointestinal involvement in Chinese patients with Behcet's disease. World J Gastroenterol. 2014; 20:17171–17178.4. Bicer A. Musculoskeletal findings in Behcet's disease. Patholog Res Int. 2012; 2012:653806.5. Akansel G, Akgoz Y, Ciftci E, Arslan A, Demirci A. MRI findings of myositis in Behçet disease. Skeletal Radiol. 2004; 33:426–428.6. Sarui H, Maruyama T, Ito I, Yamakita N, Takeda N, Nose M, et al. Necrotising myositis in Behçet's disease: characteristic features on magnetic resonance imaging and a review of the literature. Ann Rheum Dis. 2002; 61:751–752.7. Pickering MC, Walport MJ. Eosinophilic myopathic syndromes. Curr Opin Rheumatol. 1998; 10:504–510.8. Selva-O'Callaghan A, Trallero-Araguás E, Grau JM. Eosinophilic myositis: an updated review. Autoimmun Rev. 2014; 13:375–378.9. Trüeb RM, Pericin M, Winzeler B, Wüthrich B, Burg G. Eosinophilic myositis/perimyositis: frequency and spectrum of cutaneous manifestations. J Am Acad Dermatol. 1997; 37:385–391.10. Kaufman LD, Kephart GM, Seidman RJ, Buhner D, Qvarfordt I, Nässberger L, et al. The spectrum of eosinophilic myositis. Clinical and immunopathogenic studies of three patients, and review of the literature. Arthritis Rheum. 1993; 36:1014–1024.11. Hatemi G, Seyahi E, Fresko I, Talarico R, Hamuryudan V. One year in review 2016: Behçet's syndrome. Clin Exp Rheumatol. 2016; 34:6 Suppl 102. 10–22.12. Hall FC, Krausz T, Walport MJ. Idiopathic eosinophilic myositis. QJM. 1995; 88:581–586.13. Sladek GD, Vasey FB, Sieger B, Behnke DA, Germain BF, Espinoza LR. Relapsing eosinophilic myositis. J Rheumatol. 1983; 10:467–470.14. Agrawal BL, Giesen PC. Eosinophilic myositis. An unusual cause of pseudotumor and eosinophilia. JAMA. 1981; 246:70–71.15. Sharma P, Sharma MC. Resolving eosinophilic myositis: MR features. J Comput Assist Tomogr. 2001; 25:151–153.