J Korean Assoc Oral Maxillofac Surg.
2017 Oct;43(5):343-350. 10.5125/jkaoms.2017.43.5.343.
Intracorporeal reduction of condylar fracture using both pedicled condylar and seperated ramal fragments after vertical ramal osteotomy
- Affiliations
-
- 1Division of Oral and Maxillofacial Surgery, Department of Dentistry, Inha University School of Medicine, Incheon, Korea. jjm0219@naver.com
- KMID: 2393601
- DOI: http://doi.org/10.5125/jkaoms.2017.43.5.343
Abstract
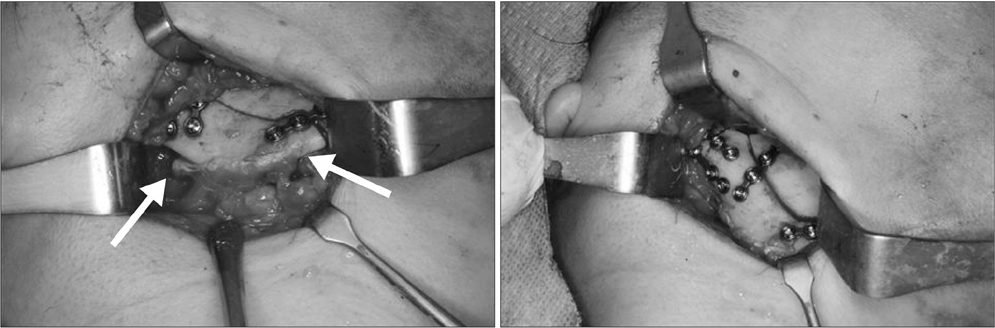
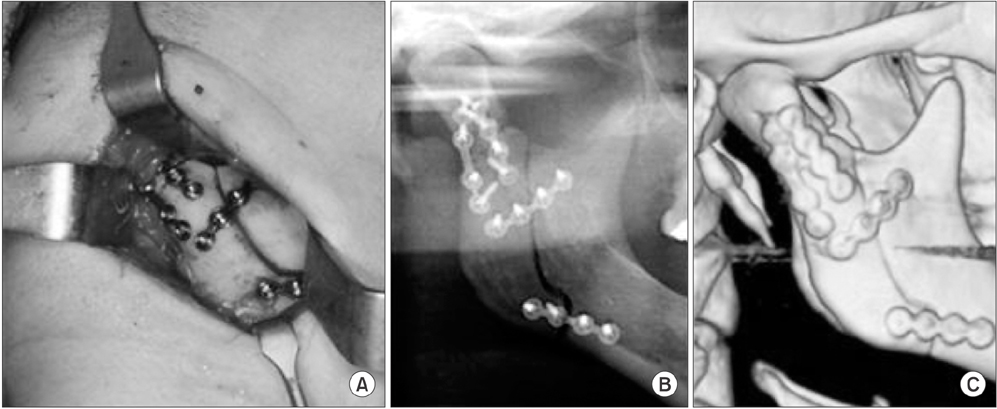
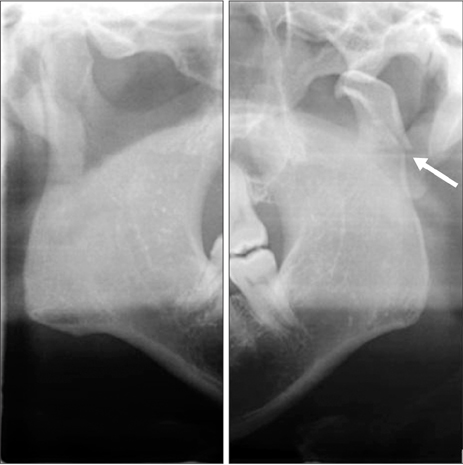
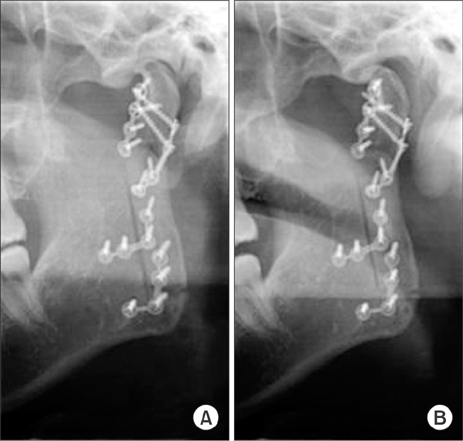
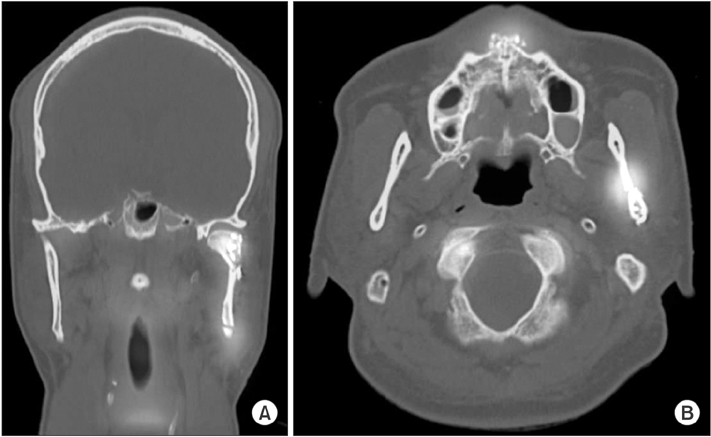
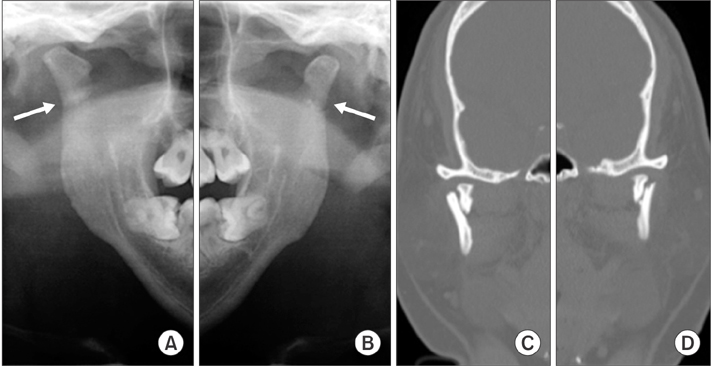
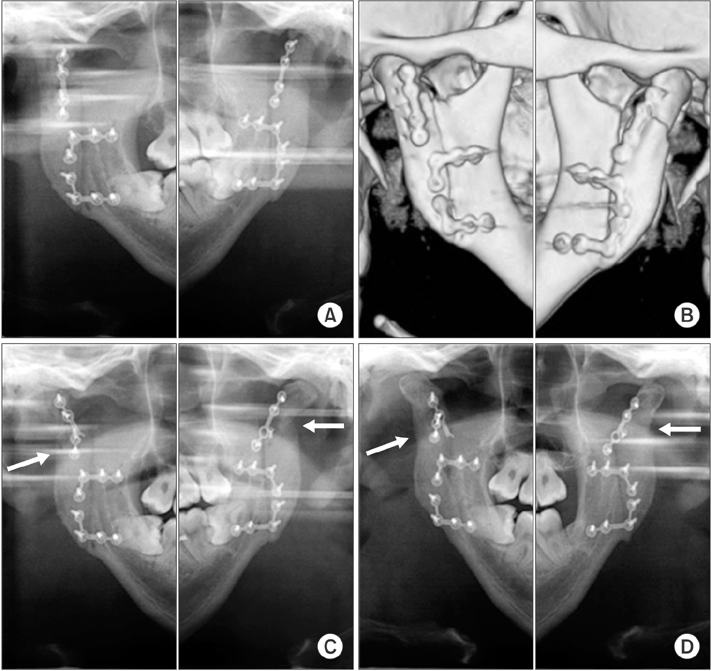
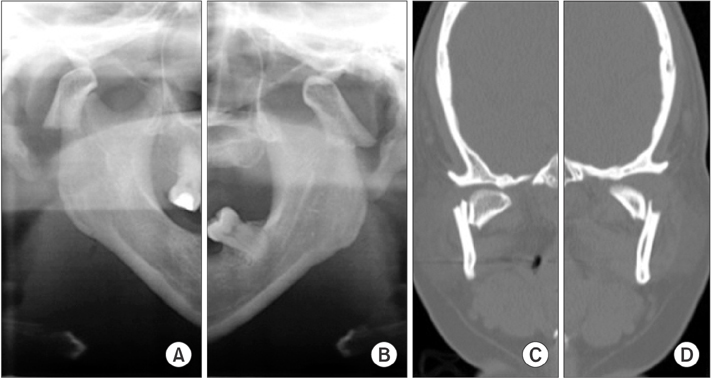
- The aim of this study is to introduce a surgical technique that can maintain blood supply to prevent condylar resorption in the extracorporeal reduction of condylar fracture. Neither the medial pterygoid muscle on the ramal bone nor the lateral pterygoid muscle on the condylar fragment was detached after vertical ramal osteotomy. Thus, reduction was performed in the intracorporeal state. Therefore, blood supply was expected to be maintained to the fragments of both the condylar and ramal bones. On postoperative radiographs, the anatomical outline of the fractured condyle was well restored, and the occlusion was stable. In the unilateral case, there were no signs of mandibular condylar resorption until postoperative 3 weeks. In the 2 bilateral cases, condylar displacements with plate fractures and screw loosening were observed at postoperative 1 month or 5 months, but radiodensity at the displaced fracture site increased during the follow-up period. Finally, complete remodeling of the condylar fragments with restored anatomic appearance was observed on 8-month or 2-year follow-up radiographs. All cases exhibited good healing aspects with no signs or symptoms of mandibular condylar dysfunction during the postoperative remodeling period after intracorporeal reduction of condylar fracture.
Keyword
Figure
Reference
-
1. Kim MK, Kwon KJ, Kim SG, Park YW, Kim JY, Kweon HY. Modified extracorporeal reduction of the mandibular condylar neck fracture. J Korean Assoc Maxillofac Plast Reconstr Surg. 2014; 36:30–36.
Article2. Hidding J, Wolf R, Pingel D. Surgical versus non-surgical treatment of fractures of the articular process of the mandible. J Craniomaxillofac Surg. 1992; 20:345–347.
Article3. Zide MF, Kent JN. Indications for open reduction of mandibular condyle fractures. J Oral Maxillofac Surg. 1983; 41:89–98.
Article4. Zide MF. Open reduction of mandibular condyle fractures. Clin Plast Surg. 1989; 16:69–76.5. Silvennoinen U, Raustia AM, Lindqvist C, Oikarinen K. Occlusal and temporomandibular joint disorders in patients with unilateral condylar fracture. A prospective one-year study. Int J Oral Maxillofac Surg. 1998; 27:280–285.
Article6. Ellis E 3rd, McFadden D, Simon P, Throckmorton G. Surgical complications with open treatment of mandibular condylar process fractures. J Oral Maxillofac Surg. 2000; 58:950–958.
Article7. Gupta MV, Sahoo NK. Extracorporeal fixation of displaced mandibular condylar fracture: viable option. Med J Armed Forces India. 2009; 65:229–231.
Article8. Davis BR, Powell JE, Morrison AD. Free-grafting of mandibular condyle fractures: clinical outcomes in 10 consecutive patients. Int J Oral Maxillofac Surg. 2005; 34:871–876.
Article9. Pereira MD, Marques A, Ishizuka M, Keira SM, Brenda E, Wolosker AB. Surgical treatment of the fractured and dislocated condylar process of the mandible. J Craniomaxillofac Surg. 1995; 23:369–376.
Article10. Iizuka T, Lindqvist C, Hallikainen D, Mikkonen P, Paukku P. Severe bone resorption and osteoarthrosis after miniplate fixation of high condylar fractures. A clinical and radiologic study of thirteen patients. Oral Surg Oral Med Oral Pathol. 1991; 72:400–407.
Article11. Park JM, Jang YW, Kim SG, Park YW, Rotaru H, Baciut G, et al. Comparative study of the prognosis of an extracorporeal reduction and a closed treatment in mandibular condyle head and/or neck fractures. J Oral Maxillofac Surg. 2010; 68:2986–2993.
Article12. Tominaga K, Habu M, Khanal A, Mimori Y, Yoshioka I, Fukuda J. Biomechanical evaluation of different types of rigid internal fixation techniques for subcondylar fractures. J Oral Maxillofac Surg. 2006; 64:1510–1516.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Open versus closed treatment for extracapsular fracture of the mandibular condyle
- T-Condylar Fracture of Distal Humerus in a Child: A Case Report
- Long-term evaluation of mandibular condyle fractures
- Modified high-submandibular appraoch for open reduction and internal fixation of condylar fracture: case series report
- Non-Surgical Treatment of Mandibular Condylar Fracture with Functional Appliance: Clinical and Radiographic Analysis of 1 Case