J Korean Assoc Oral Maxillofac Surg.
2022 Oct;48(5):303-308. 10.5125/jkaoms.2022.48.5.303.
Open versus closed treatment for extracapsular fracture of the mandibular condyle
- Affiliations
-
- 1Department of Oral and Maxillofacial Surgery, School of Dentistry and Dental Science Research Institute, Chonnam National University, Gwangju, Korea
- KMID: 2534811
- DOI: http://doi.org/10.5125/jkaoms.2022.48.5.303
Abstract
Objectives
Selection of treatment methods for mandibular condylar fractures remains controversial. In this study, we investigated treatment methods for condylar fractures to determine the indications for open or closed reduction.
Patients and Methods
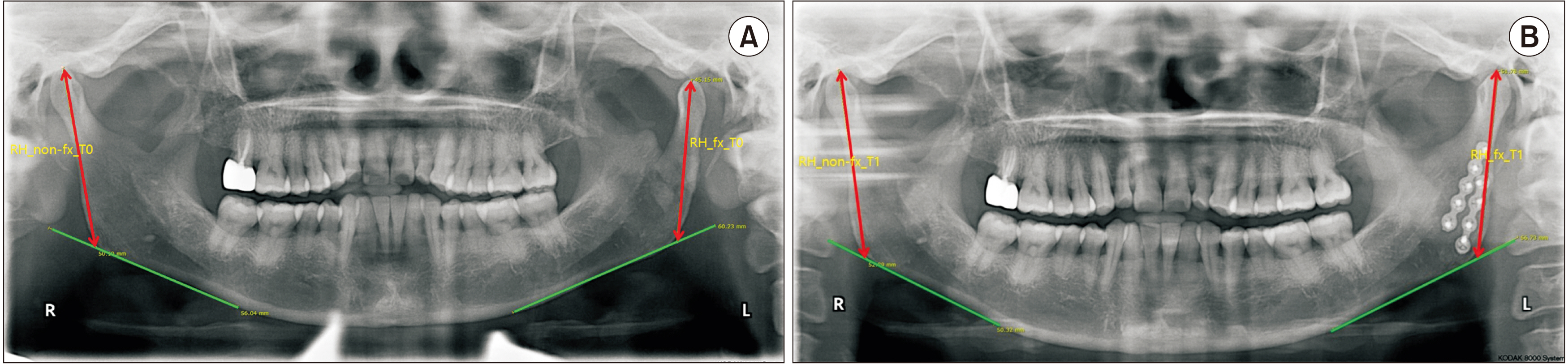
Patients >12 years of age treated for mandibular condylar fractures with a follow-up period of ≥3 months were included in this study. The medical records of enrolled patients were reviewed for sex, age, fracture site, treatment method (open or closed reconstruction), postoperative intermaxillary fixation period, operation time, and complications. Radiological analysis of fracture fragment displacement and changes in ramal height difference was performed using computed tomography and panoramic radiography.
Results
A total of 198 patients was investigated, 48.0% (n=95) of whom underwent closed reduction and 52.0% (n=103) underwent open reduction. There was no significant correlation between reduction method and patient sex, age, or follow-up period. No statistically significant difference between the incidence of complications and treatment method was observed. None of the patients underwent open reduction of condylar head fracture. Binary logistic regression analysis showed that open reduction was significantly more frequent in patients with subcondylar fracture compared to in those with a fracture in the condylar head area. There was no statistically significant correlation between the groups and fracture fragment displacement. However, there was a significant difference between the treatment groups in amount of change in ramal height difference between the fractured and the nonfractured sides during treatment.
Conclusion
No significant clinical differences were found between the open and closed reduction methods in patients with mandibular condylar fractures. According to fracture site, closed reduction was preferred for condyle head fractures. There was no significant relationship between fracture fragment displacement and treatment method.
Figure
Reference
-
References
1. Lindahl L. 1977; Condylar fractures of the mandible. IV. Function of the masticatory system. Int J Oral Surg. 6:195–203. https://doi.org/10.1016/s0300-9785(77)80009-4. DOI: 10.1016/S0300-9785(77)80009-4. PMID: 410741.
Article2. Rastogi S, Sharma S, Kumar S, Reddy MP, Niranjanaprasad Indra B. 2015; Fracture of mandibular condyle-to open or not to open: an attempt to settle the controversy. Oral Surg Oral Med Oral Pathol Oral Radiol. 119:608–13. https://doi.org/10.1016/j.oooo.2015.01.012. DOI: 10.1016/j.oooo.2015.01.012.
Article3. Kim JS, Seo HS, Kim KY, Song YJ, Kim S, Hong SM, et al. 2008; Open versus closed reduction of mandibular condyle fractures: a systematic review of comparative studies. J Korean Oral Maxillofac Surg. 34:99–107.4. Johner JP, Essig H, Neff A, Wagner MEH, Blumer M, Gander T. 2021; Volumetric evaluated bone resorption after open reduction and internal fixation of condylar head fractures of the mandible. J Oral Maxillofac Surg. 79:1902–13. https://doi.org/10.1016/j.joms.2021.04.018. DOI: 10.1016/j.joms.2021.04.018. PMID: 34062130.
Article5. Rozeboom AVJ, Dubois L, Bos RRM, Spijker R, de Lange J. 2017; Closed treatment of unilateral mandibular condyle fractures in adults: a systematic review. Int J Oral Maxillofac Surg. 46:456–64. https://doi.org/10.1016/j.ijom.2016.11.009. DOI: 10.1016/j.ijom.2016.11.009. PMID: 27955799.
Article6. van den Bergh B, Blankestijn J, van der Ploeg T, Tuinzing DB, Forouzanfar T. 2015; Conservative treatment of a mandibular condyle fracture: comparing intermaxillary fixation with screws or arch bar. A randomised clinical trial. J Craniomaxillofac Surg. 43:671–6. https://doi.org/10.1016/j.jcms.2015.03.010. DOI: 10.1016/j.jcms.2015.03.010. PMID: 25911121.
Article7. Gupta M, Iyer N, Das D, Nagaraj J. 2012; Analysis of different treatment protocols for fractures of condylar process of mandible. J Oral Maxillofac Surg. 70:83–91. https://doi.org/10.1016/j.joms.2011.02.009. DOI: 10.1016/j.joms.2011.02.009. PMID: 21549492.
Article8. Bhagol A, Singh V, Kumar I, Verma A. 2011; Prospective evaluation of a new classification system for the management of mandibular subcondylar fractures. J Oral Maxillofac Surg. 69:1159–65. https://doi.org/10.1016/j.joms.2010.05.050. DOI: 10.1016/j.joms.2010.05.050. PMID: 21211891.
Article9. So BK, Ko KS, Kim DH, Jang HS, Lee ES, Lim HK. 2021; Semi-rigid fixation using a sliding plate for treating fractures of the mandibular condylar process. J Clin Med. 10:5782. https://doi.org/10.3390/jcm10245782. DOI: 10.3390/jcm10245782. PMID: 34945078. PMCID: PMC8705034.
Article10. He D, Yang C, Chen M, Jiang B, Wang B. 2009; Intracapsular condylar fracture of the mandible: our classification and open treatment experience. J Oral Maxillofac Surg. 67:1672–9. https://doi.org/10.1016/j.joms.2009.02.012. DOI: 10.1016/j.joms.2009.02.012. PMID: 19615581.
Article11. Mohamed AAS, Abotaleb B, Ahmed Abdulqader A, Hongliang D, Sakran KA, He D. 2021; Three-dimensional assessment of accuracy for open reduction and internal fixation of the subcondylar fracture and its implications on the TMJ function. J Craniomaxillofac Surg. 49:1035–43. https://doi.org/10.1016/j.jcms.2021.06.009. DOI: 10.1016/j.jcms.2021.06.009. PMID: 34217568.
Article12. Ren R, Dai J, Zhi Y, Xie F, Shi J. 2020; Comparison of temporomandibular joint function and morphology after surgical and non-surgical treatment in adult condylar head fractures. J Craniomaxillofac Surg. 48:323–30. https://doi.org/10.1016/j.jcms.2020.01.019. DOI: 10.1016/j.jcms.2020.01.019. PMID: 32113881.
Article13. Shiju M, Rastogi S, Gupta P, Kukreja S, Thomas R, Bhugra AK, et al. 2015; Fractures of the mandibular condyle--open versus closed--a treatment dilemma. J Craniomaxillofac Surg. 43:448–51. https://doi.org/10.1016/j.jcms.2015.01.012. DOI: 10.1016/j.jcms.2015.01.012. PMID: 25726918.
Article14. Danda AK, Muthusekhar MR, Narayanan V, Baig MF, Siddareddi A. 2010; Open versus closed treatment of unilateral subcondylar and condylar neck fractures: a prospective, randomized clinical study. J Oral Maxillofac Surg. 68:1238–41. https://doi.org/10.1016/j.joms.2009.09.042. DOI: 10.1016/j.joms.2009.09.042. PMID: 20303209.
Article15. Bindal M, Joshi A, Bhat A, Anehosur V. 2019; Are facial asymmetry and condylar displacement associated with ramal height and treatment outcomes in unilateral condylar fracture when managed by the closed method? J Oral Maxillofac Surg. 77:789.e1–8. https://doi.org/10.1016/j.joms.2018.11.013. DOI: 10.1016/j.joms.2018.11.013. PMID: 30576677.
Article16. Chrcanovic BR. 2015; Surgical versus non-surgical treatment of mandibular condylar fractures: a meta-analysis. Int J Oral Maxillofac Surg. 44:158–79. https://doi.org/10.1016/j.ijom.2014.09.024. DOI: 10.1016/j.ijom.2014.09.024. PMID: 25457827.
Article17. Ryu JY, Kim HS, Park CY, Kook MS, Park HJ, Oh HK. 2008; A retrospective clinical study of condylar fractures of the mandible in a 4-year period. J Korean Oral Maxillofac Surg. 34:388–97.18. Marker P, Nielsen A, Bastian HL. 2000; Fractures of the mandibular condyle. Part 2: results of treatment of 348 patients. Br J Oral Maxillofac Surg. 38:422–6. https://doi.org/10.1054/bjom.2000.0457. DOI: 10.1054/bjom.2000.0457. PMID: 11010767.
Article19. Takenoshita Y, Ishibashi H, Oka M. 1990; Comparison of functional recovery after nonsurgical and surgical treatment of condylar fractures. J Oral Maxillofac Surg. 48:1191–5. https://doi.org/10.1016/0278-2391(90)90535-a. DOI: 10.1016/0278-2391(90)90535-A. PMID: 2213313.
Article20. Vesnaver A, Ahčan U, Rozman J. 2012; Evaluation of surgical treatment in mandibular condyle fractures. J Craniomaxillofac Surg. 40:647–53. https://doi.org/10.1016/j.jcms.2011.10.029. DOI: 10.1016/j.jcms.2011.10.029. PMID: 22079126.
Article21. Wiedemann D, Bonaros N, Schachner T, Weidinger F, Lehr EJ, Vesely M, et al. 2012; Surgical problems and complex procedures: issues for operative time in robotic totally endoscopic coronary artery bypass grafting. J Thorac Cardiovasc Surg. 143:639–47.e2. https://doi.org/10.1016/j.jtcvs.2011.04.039. DOI: 10.1016/j.jtcvs.2011.04.039. PMID: 21719035.
Article22. Mohammad OA, Ashour EM, Hassanein FAA. 2022; Evaluation of condylar position in anterior mandibular fractures using 3 dimensional miniplate osteosynthesis versus conventional miniplates: randomized clinical trial. J Craniomaxillofac Surg. 50:61–9. https://doi.org/10.1016/j.jcms.2021.09.014. DOI: 10.1016/j.jcms.2021.09.014. PMID: 34756733.
Article23. Sawazaki R, Lima Júnior SM, Asprino L, Moreira RW, de Moraes M. 2010; Incidence and patterns of mandibular condyle fractures. J Oral Maxillofac Surg. 68:1252–9. https://doi.org/10.1016/j.joms.2009.03.064. DOI: 10.1016/j.joms.2009.03.064. PMID: 19939534.
Article24. Abdel-Galil K, Loukota R. 2010; Fractures of the mandibular condyle: evidence base and current concepts of management. Br J Oral Maxillofac Surg. 48:520–6. https://doi.org/10.1016/j.bjoms.2009.10.010. DOI: 10.1016/j.bjoms.2009.10.010. PMID: 19900741.
Article25. Sang JK, Lee JH. 2011; The study of the effect of mandibular growth and function in pediatric unilateral condyle fractures. J Korean Assoc Oral Maxillofac Surg. 37:448–56. https://doi.org/10.5125/jkaoms.2011.37.6.448. DOI: 10.5125/jkaoms.2011.37.6.448.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Current Concepts in the Mandibular Condyle Fracture Management Part II: Open Reduction Versus Closed Reduction
- OPEN REDUCTION AND TRANSORAL FIXATION USING TROCHAR FOR MANDIBULAR SUBCONDYLE FRACTURE
- Retrospective study for prognosis after open and closed reduction of the mandibular condyle fractures
- Overview of Mandibular Condyle Fracture
- Outcome of Surgical Treatment for Mandibular Condyle Fractures