Prog Med Phys.
2017 Sep;28(3):111-121. 10.14316/pmp.2017.28.3.111.
Uncertainty Assessment: Relative versus Absolute Point Dose Measurement for Patient Specific Quality Assurance in EBRT
- Affiliations
-
- 1Medical Physics & Radiation Engineering Department, Canberra Hospital & Health Services, ACT, Australia. talat.mahmood@act.gov.au
- 2Radiation Oncology Department, North-West General Hospital & Research Centre, Peshawar, Pakistan.
- KMID: 2393372
- DOI: http://doi.org/10.14316/pmp.2017.28.3.111
Abstract
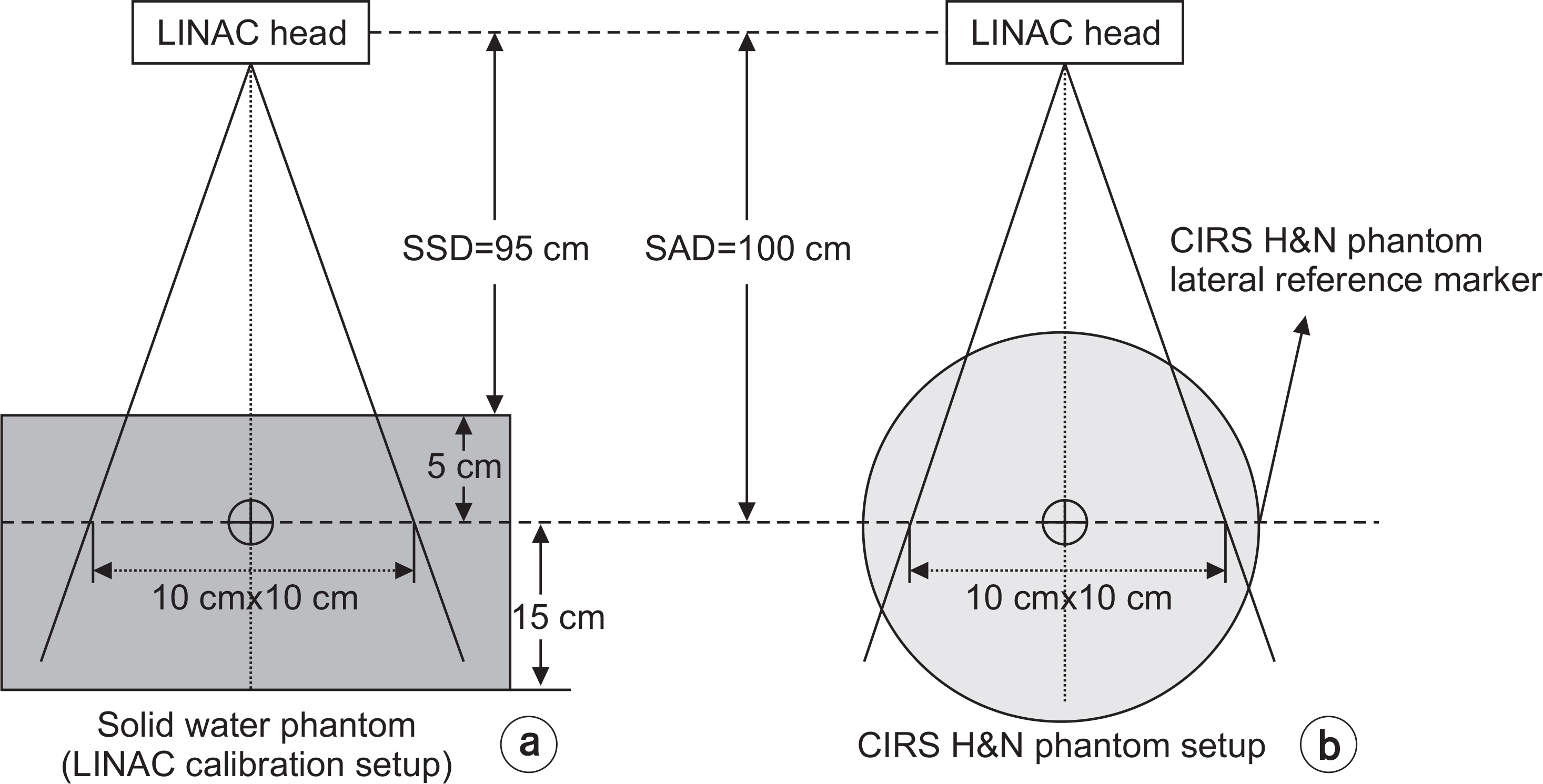
- Verification of dose distribution is an essential part of ensuring the treatment planning system's (TPS) calculated dose will achieve the desired outcome in radiation therapy. Each measurement have uncertainty associated with it. It is desirable to reduce the measurement uncertainty. A best approach is to reduce the uncertainty associated with each step of the process to keep the total uncertainty under acceptable limits. Point dose patient specific quality assurance (QA) is recommended by American Association of Medical Physicists (AAPM) and European Society for Radiotherapy and Oncology (ESTRO) for all the complex radiation therapy treatment techniques. Relative and absolute point dose measurement methods are used to verify the TPS computed dose. Relative and absolute point dose measurement techniques have a number of steps to measure the point dose which includes chamber cross calibration, electrometer reading, chamber calibration coefficient, beam quality correction factor, reference conditions, influences quantities, machine stability, nominal calibration factor (for relative method) and absolute dose calibration of machine. Keeping these parameters in mind, the estimated relative percentage uncertainty associated with the absolute point dose measurement is 2.1% (k=1). On the other hand, the relative percentage uncertainty associated with the relative point dose verification method is estimated to 1.0% (k=1). To compare both point dose measurement methods, 13 head and neck (H&N) IMRT patients were selected. A point dose for each patient was measured with both methods. The average percentage difference between TPS computed dose and measured absolute relative point dose was 1.4% and 1% respectively. The results of this comparative study show that while choosing the relative or absolute point dose measurement technique, both techniques can produce similar results for H&N IMRT treatment plans. There is no statistically significant difference between both point dose verification methods based upon the t-test for comparing two means.
Keyword
- Uncertainty; EBRT; IMRT; Point dose; QA
Figure
Reference
-
1. Thwaites DI. “Accuracy required and achievable in radiotherapy dosimetry: have modern technology and techniques changes our view?” 7th IC3DDose, Journal of Physics: Conference series. 2013. 444.2. ICRU Report 24. Determination of absorbed dose in a patient irradiated by beans of x or gamma rays in radiotherapy procedures, ICRU Report. Bethesda: ICRU. 1976; 24.3. Mayles P, Thwaites DI, Rosenwald JC. Handbook of Radiotherapy Physics. Taylor & Francis London. 2007. 793–808.
Article4. Dobbs J, Thwaites DI. Physics Aspect of Quality Control in radiotherapy. IPEM Report. Institute of physics and engineering in Medicine: IPEM. 1998; 08.5. Mijnheer BJ, Batterman JJ, Wambersie A. What degree of accuracy is required and can be achieved in photon and neutron therapy? Radiother Oncol. 1987; 3:237–52.
Article6. ICRU Report 76. Measurement Quality assurance for ionisation radiation dosimetry. ICRU Report. Bethesda: ICRU. 2006.7. Oliver C, Butler D, Webb D, Wright T Lye J. Ramanathan G, Harty P, Takau V. Maintaining the accuracy of the 60Co Calibration services at the ARPANSA post source replacement in 2010. Australas Phys Eng Sci Med. 2015; 38:325–30.8. Gary A. Ezzell, James M. Galvin, Daniel Low, Jatinder R. Palta, Isaac Rosen, Michael B. Sharpe, Ping Xia, Lei Xing, Cedric X. Yu. Guidance document on delivery, treatment planning, and clinical implementation of IMRT: Report of the IMRT subcommittee of the AAPM radiation therapy committee. Med. Phys. 2003; 30:2089–115.9. Daniel A. Low, Jean M. Moran, James F. Dempsey, Lei Dong, Mark Oldham. Dosimetry tools and techniques for IMRT. Med. Phys. 2011; 38:1313–38.10. IAEA-TRS-398. International Atomic Energy Agency, Absorb dose determination on external beam radiotherapy, An international code of practise for dosimetry based on standard of absorbed dose to water, Technical Reports Series No. 398. IAEA Report. IAEA Vienna. 2006. 61–72.11. Absolute dose measurements in external beam radiotherapy application of codes of practice based on standards of absorbed dose to water IBA dosimetry GmbH, Schwarzenbruck, Germany (Doc-Id: P-Codes of Practice Absolute Dosimetry-510-001 01). 2012.12. Calibration report (cCAL00710/03) on a therapy ionisation chamber and cal00239/01 calibration report on an electrometer from primary standard dosimetry laboratories (PSDL) of Australian Radiation Protection and Nuclear Safely Agency (ARPNSA). 2014.13. ICRU Report 37. International Commission on Radiation Units and Measurements, Stopping Powers for Electrons and Positrons. ICRU Report. Bethesda:. 1984.14. Das IJ, Zhu TC. Thermal and temporal response of ionisation chambers in radiation dosimetry. Med Phys. 2004; 31:573–578.15. Castro P, García-Vicente F, Mínguez C, Floriano A, Sevilla-no D, Pérez L, Torres JJ. Study of the uncertainty in the determination of the absorbed dose to water during external beam radiotherapy calibration. J. Appl. Clin. Med. Phys. 2008; 22:70–86.
Article16. Seuntjens JP, Ross CK. Shortt KP, Roger DWO. Absorbed-dose beam quality conversion factor cylindrical chamber in high energy photon beam. Med Phys. 2000; 27:2763–78.17. Weinhous MS, Meli JA. Determining Pion, the correction factor for recombination losses in an ionisation chamber. Med. Phys. 1984; 11:846–9.18. Zankowski C, Podgorask EB. Determination of saturation charge and collection efficiency for ionisation chamber in continuous beam. Med Phys. 1998; 25:908–15.19. Seuntjens JP, Ross CK, Shortt KR, Rogers DWO. Absorbed-dose beam quality conversion factors for cylindrical chambers in high energy photon beams. Med. Phys. 2000; 27:2763–78.
Article20. Gareth J Webster, Carl G Rowbottom, Ranald I Mackay. Development of an optimum photon beam model for headand-neck intensity-modulated radiotherapy. J. Appl. Clin. Med. Phys. 2007; 8:29–138.21. Losasso T. IMRT delivery performance with a Varian multileaf collimator. Int. J. Radiat. Oncol. Biol. Phys. 2008; 71:85–8.
Article22. Eun J, Kyung-Rae D, Woon-Kwan C, In-Chul I, Yun-Sik Y. An Overall Stem Effect, including Stem Leakage and Stem Scatter, for a TM30013 Farmer-type Chamber. J. Korean Phy Soc. 2011; 58:1688–96.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- GafChromic Film Dosimetry for Stereotactic Radiosurgery with a Linear Accelerator
- Practical Implementation of Patient-Specific Quality Assurance for Small and Multiple Brain Tumors in CyberKnife with Fixed Collimators
- The Study on the Head and Neck Phantom for Quality Assurance of Intensity Modulated Radiotherapy
- Patient-Specific Quality Assurance in a Multileaf Collimator-Based CyberKnife System Using the Planar Ion Chamber Array
- Therapeutic Proton Beam Range Measurement with EBT3 Film and Comparison with Tool for Particle Simulation