Prog Med Phys.
2018 Jun;29(2):59-65. 10.14316/pmp.2018.29.2.59.
Patient-Specific Quality Assurance in a Multileaf Collimator-Based CyberKnife System Using the Planar Ion Chamber Array
- Affiliations
-
- 1Department of Radiation Oncology, Seoul National University Hospital, Seoul, Korea.
- 2Department of Radiation Oncology, Yonsei University College of Medicine, Seoul, Korea. holee@yuhs.ac
- KMID: 2415904
- DOI: http://doi.org/10.14316/pmp.2018.29.2.59
Abstract
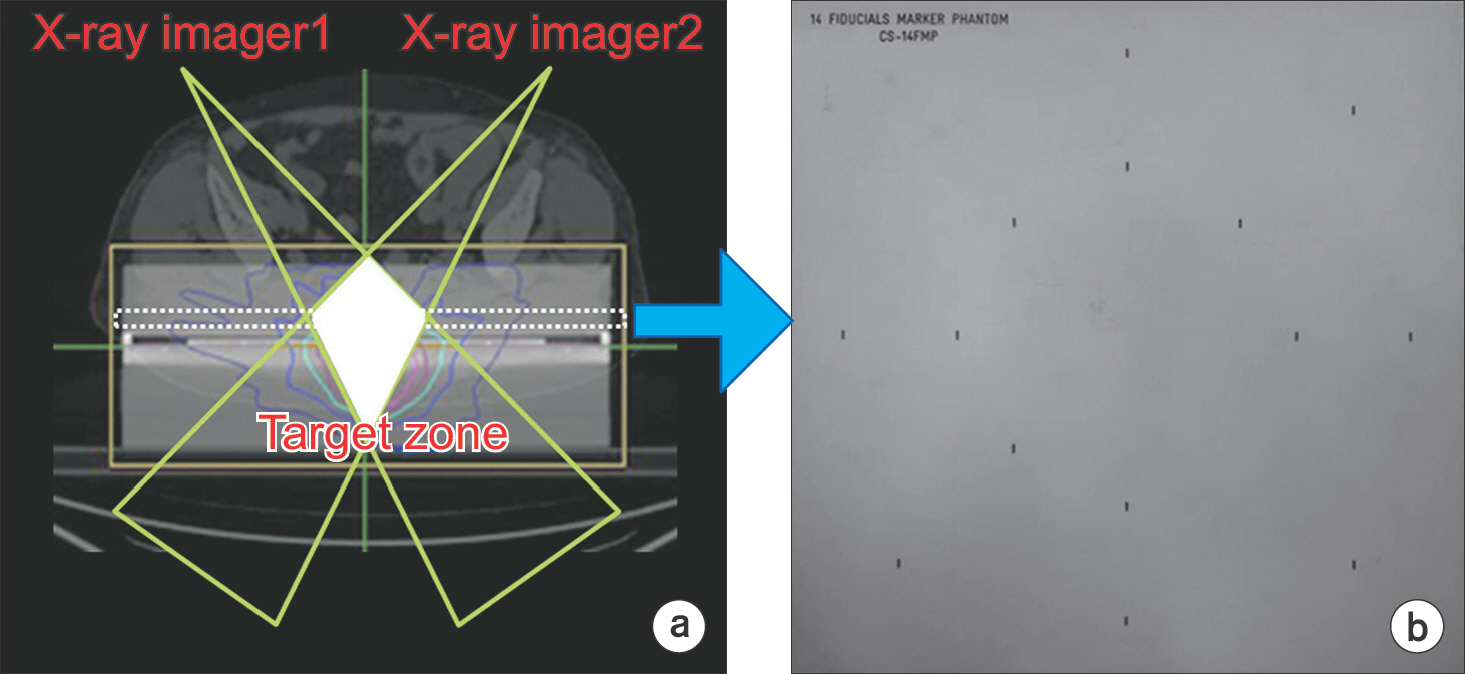
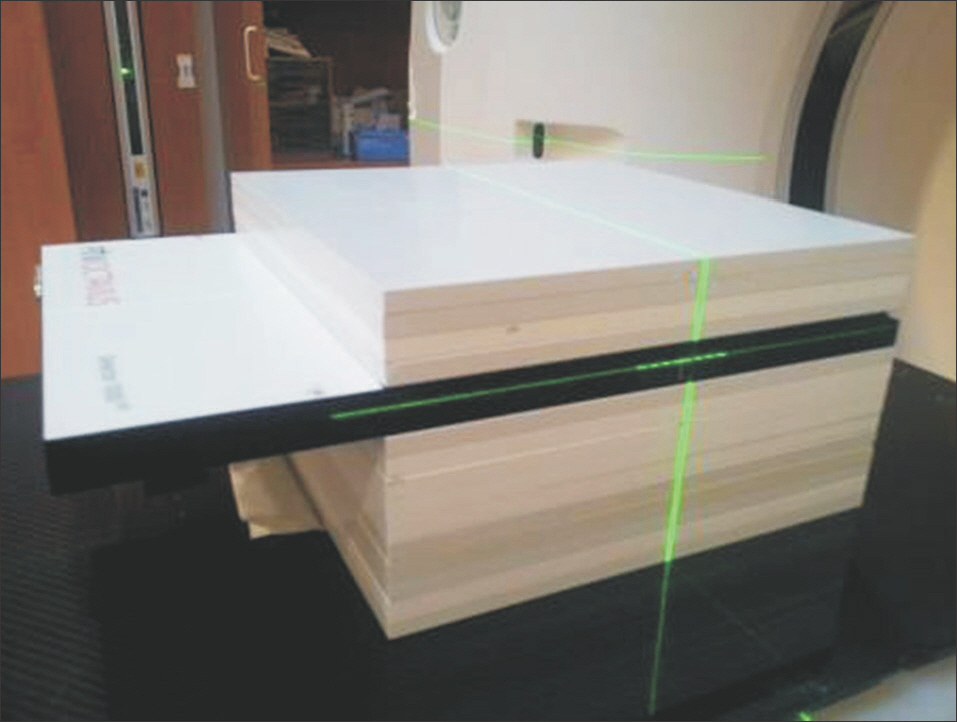
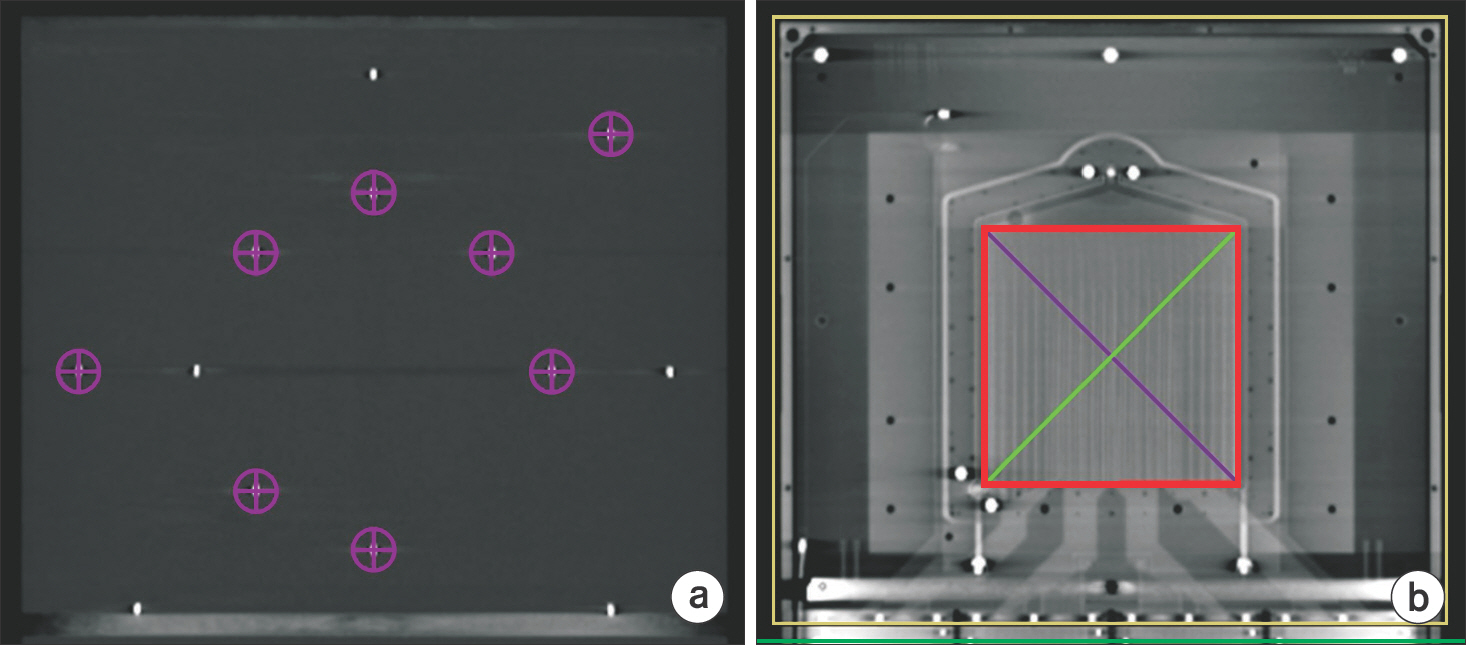
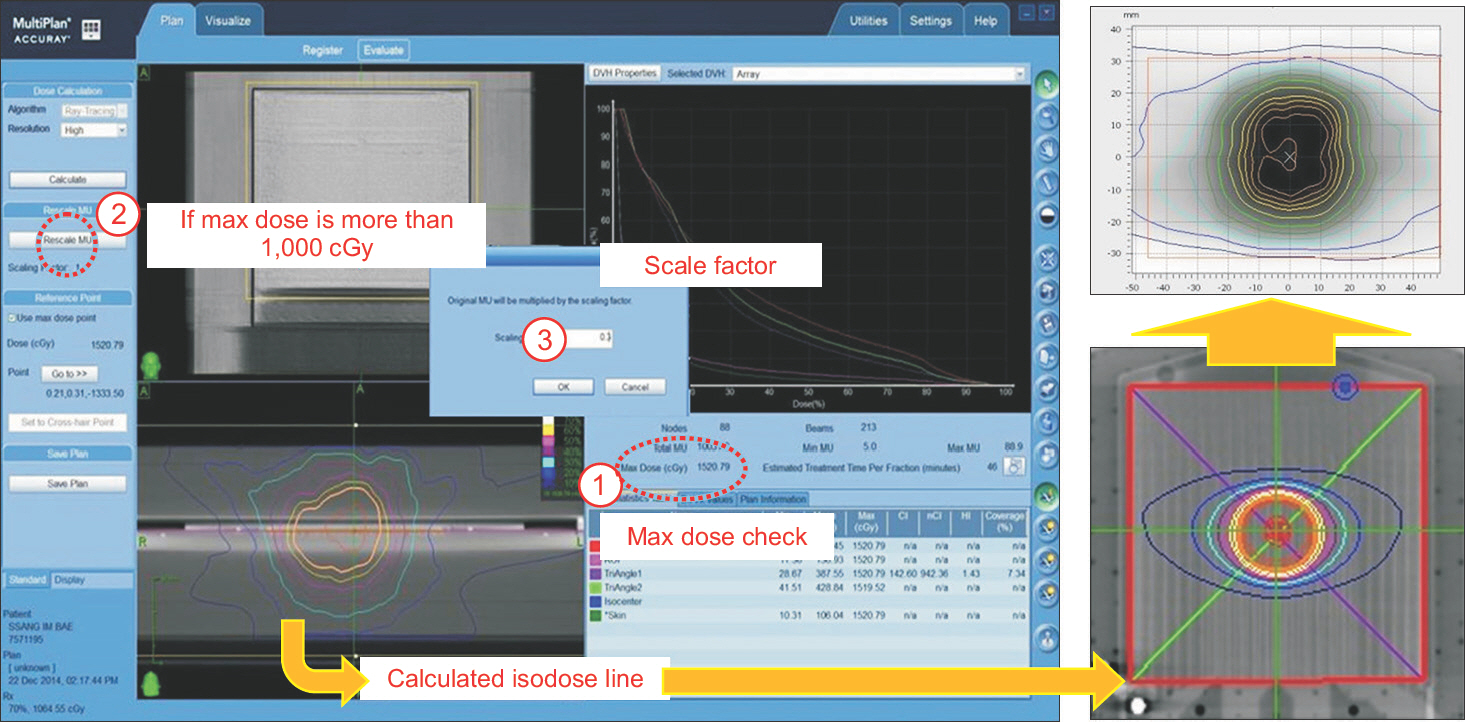
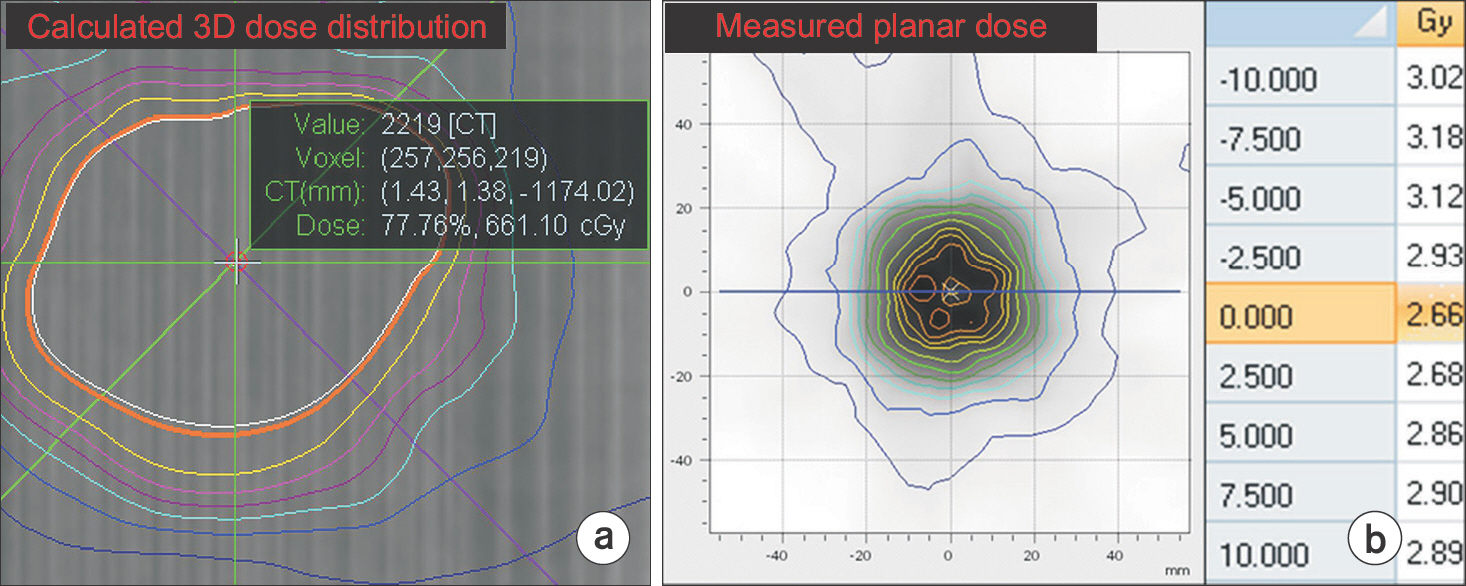
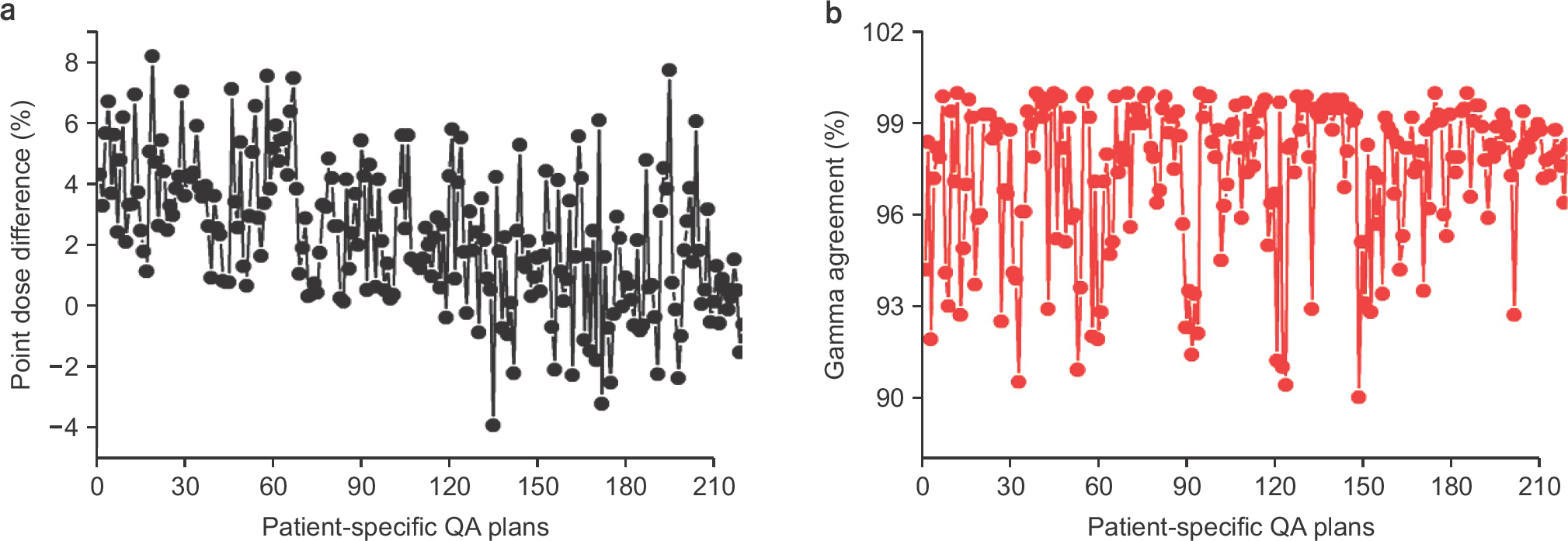
- This paper describes the clinical use of the dose verification of multileaf collimator (MLC)-based CyberKnife plans by combining the Octavius 1000SRS detector and water-equivalent RW3 slab phantom. The slab phantom consists of 14 plates, each with a thickness of 10 mm. One plate was modified to support tracking by inserting 14 custom-made fiducials on surface holes positioned at the outer region of 10×10 cm². The fiducial-inserted plate was placed on the 1000SRS detector and three plates were additionally stacked up to build the reference depth. Below the detector, 10 plates were placed to avoid longer delivery times caused by proximity detection program alerts. The cross-calibration factor prior to phantom delivery was obtained by performing with 200 monitor units (MU) on the field size of 95×92.5 mm². After irradiation, the measured dose distribution of the coronal plane was compared with the dose distribution calculated by the MultiPlan treatment planning system. The results were assessed by comparing the absolute dose at the center point of 1000SRS and the 3-D Gamma (γ) index using 220 patient-specific quality assurance (QA). The discrepancy between measured and calculated doses at the center point of 1000SRS detector ranged from −3.9% to 8.2%. In the dosimetric comparison using 3-D γ-function (3%/3 mm criteria), the mean passing rates with γ-parameter ≤ 1 were 97.4%±2.4%. The combination of the 1000SRS detector and RW3 slab phantom can be utilized for dosimetry validation of patient-specific QA in the CyberKnife MLC system, which made it possible to measure absolute dose distributions regardless of tracking mode.
Figure
Cited by 1 articles
-
Skin Dose Comparison of CyberKnife and Helical Tomotherapy for Head-and-Neck Stereotactic Body Radiotherapy
Jeongmin Yoon, Kwangwoo Park, Jin Sung Kim, Yong Bae Kim, Ho Lee
Prog Med Phys. 2019;30(1):1-6. doi: 10.14316/pmp.2019.30.1.1.
Reference
-
References
1. Blomgren H, Lax I, Naslund I, Svanstrom R. Stereotactic high dose fraction radiation therapy of extracranial tumors using an accelerator. Clinical experience of the first thirty-one patients. Acta Oncol. 1995; 34(6):861–70.
Article2. Yoon J, Park K, Kim JS, Kim YB, Lee H. Acceptance Testing and Commissioning of Robotic Intensity-Modulated Radiation Therapy M6 System Equipped with InCiseTM 2 Multileaf Collimator. Prog Med Phys. 2018; 29(1):8–15.3. Murai T, Hattori Y, Sugie C, Iwata H, Iwabuchi M, Shibamoto Y. Comparison of multileaf collimator and conventional circular collimator systems in Cyberknife stereotactic radiotherapy. J Radiat Res. 2017; 58(5):693–700.
Article4. Mcguinness CM, Gottschalk AR, Lessard E, et al. Investigating the clinical advantages of a robotic linac equipped with a multileaf collimator in the treatment of brain and prostate cancer patients. J Appl Clin Med Phys. 2015; 16(5):284–95.
Article5. Dieterich S, Cavedon C, Chuang CF, et al. Report of AAPM TG 135: quality assurance for robotic radiosurgery. Med Phys. 2011; 38(6):2914–36.
Article6. Chong NS, Lee JJS, Kung WH, et al. Patient delivery quality assurance for linac-based IMRT and helical tomotherapy using solid state detectors. Radiat Meas. 2011; 46(12):1993–95.
Article7. Markovic M, Stathakis S, Mavroidis P, Jurkovic IA, Papanikolaou N. Characterization of a two-dimensional liquid-filled ion chamber detector array used for verification of the treatments in radiotherapy. Med Phys. 2014; 41(5):
Article8. Seppenwoolde Y, Berbeco RI, Nishioka S, Shirato H, Heijmen B. Accuracy of tumor motion compensation algorithm from a robotic respiratory tracking system: A simulation study. Med Phys. 2007; 34(7):2774–84.
Article9. Pepin EW, Wu H, Zhang Y, Lord B. Correlation and prediction uncertainties in the cyberknife synchrony respiratory tracking system. Med Phys. 2011; 38(7):4036–44.
Article10. Ezzell GA, Burmeister JW, Dogan N, et al. IMRT commissioning: multiple institution planning and dosimetry comparisons, a report from AAPM Task Group 119. Med Phys. 2009; 36(11):5359–73.
Article11. Blanck O, Masi L, Damme MC, et al. Film-based delivery quality assurance for robotic radiosurgery: Commissioning and validation. Phys Med. 2015; 31(5):476–83.
Article12. Lin MH, Veltchev I, Koren S, Ma C, Li J. Robotic radiosurgery system patient-specific QA for extracranial treatments using the planar ion chamber array and the cylindrical diode array. J Appl Clin Med Phys. 2015; 16(4):290–305.
Article13. Kim J, Park K, Yoon J, et al. Feasibility Study of a Custom-made Film for End-to-End Quality Assurance Test of Robotic Intensity Modulated Radiation Therapy System. Prog Med Phys. 2016; 27(4):189–95.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Feasibility Study of Vertical Multileaf Collimator for Determination of Irradiation Size
- Practical Implementation of Patient-Specific Quality Assurance for Small and Multiple Brain Tumors in CyberKnife with Fixed Collimators
- Acceptance Testing and Commissioning of Robotic Intensity-Modulated Radiation Therapy M6 System Equipped with InCiseâ„¢2 Multileaf Collimator
- Clinical performance of FractionLab in patient-specific quality assurance for intensity-modulated radiotherapy: a retrospective study
- Optimization of Parallel-Hole Collimator for Small Gamma Camera Based on Pixellated Crystal Array