Korean J Obstet Gynecol.
2012 Oct;55(10):766-771.
Metastatic gestational trophoblastic neoplasm presenting as spontaneous renal and cerebral hemorrhage with low titer of HCG: A case report of an unusual case
- Affiliations
-
- 1Department of Obstetrics and Gynecology, Chonnam National University Medical School, Gwangju, Korea. seokmo2001@yahoo.co.kr
Abstract
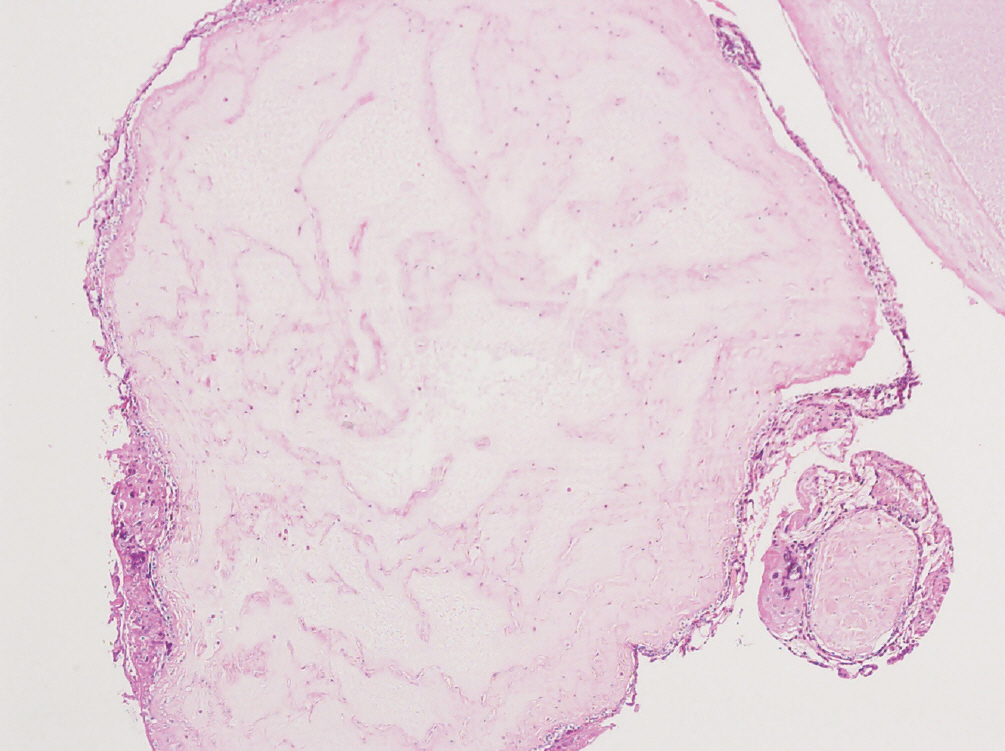
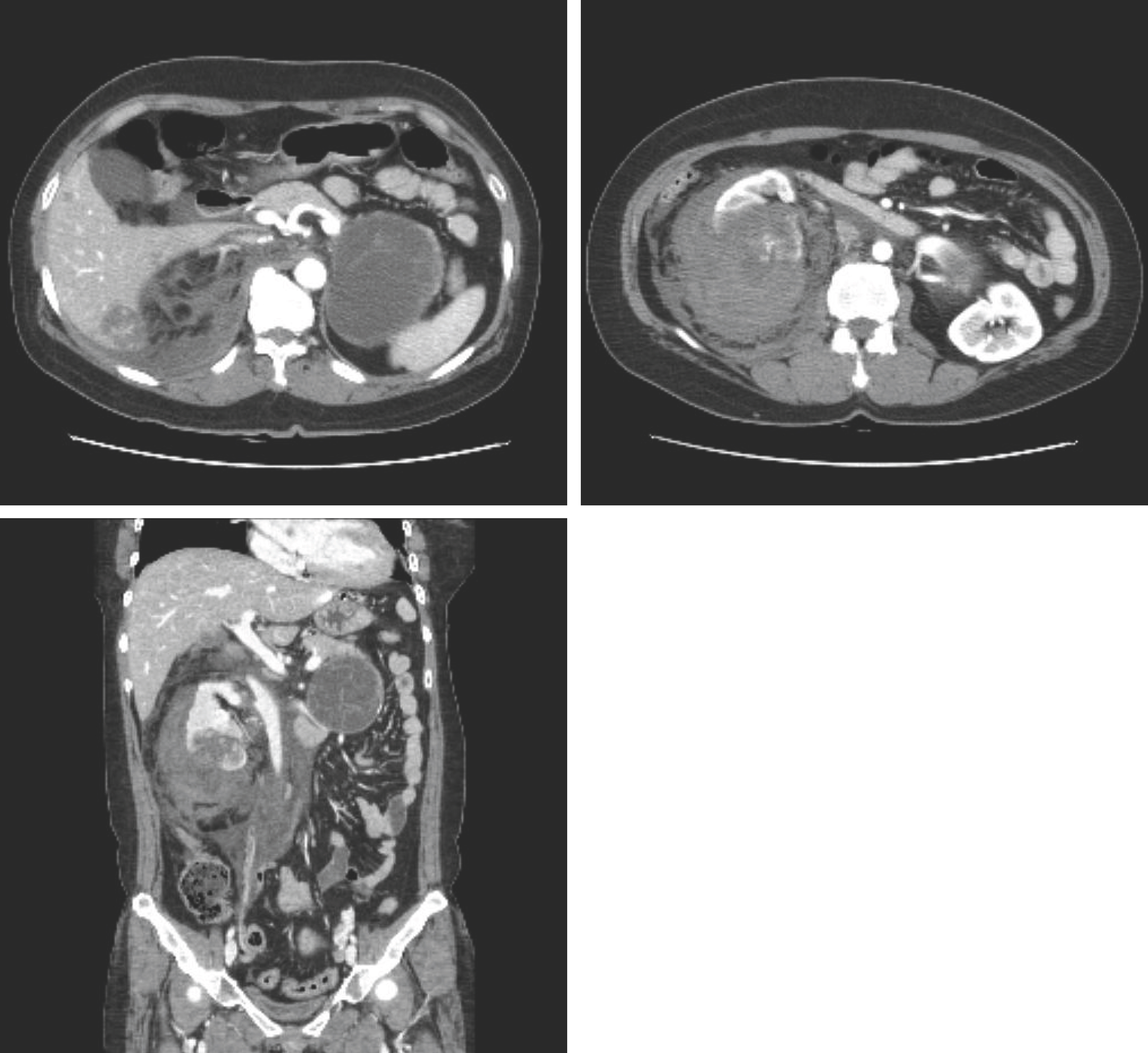
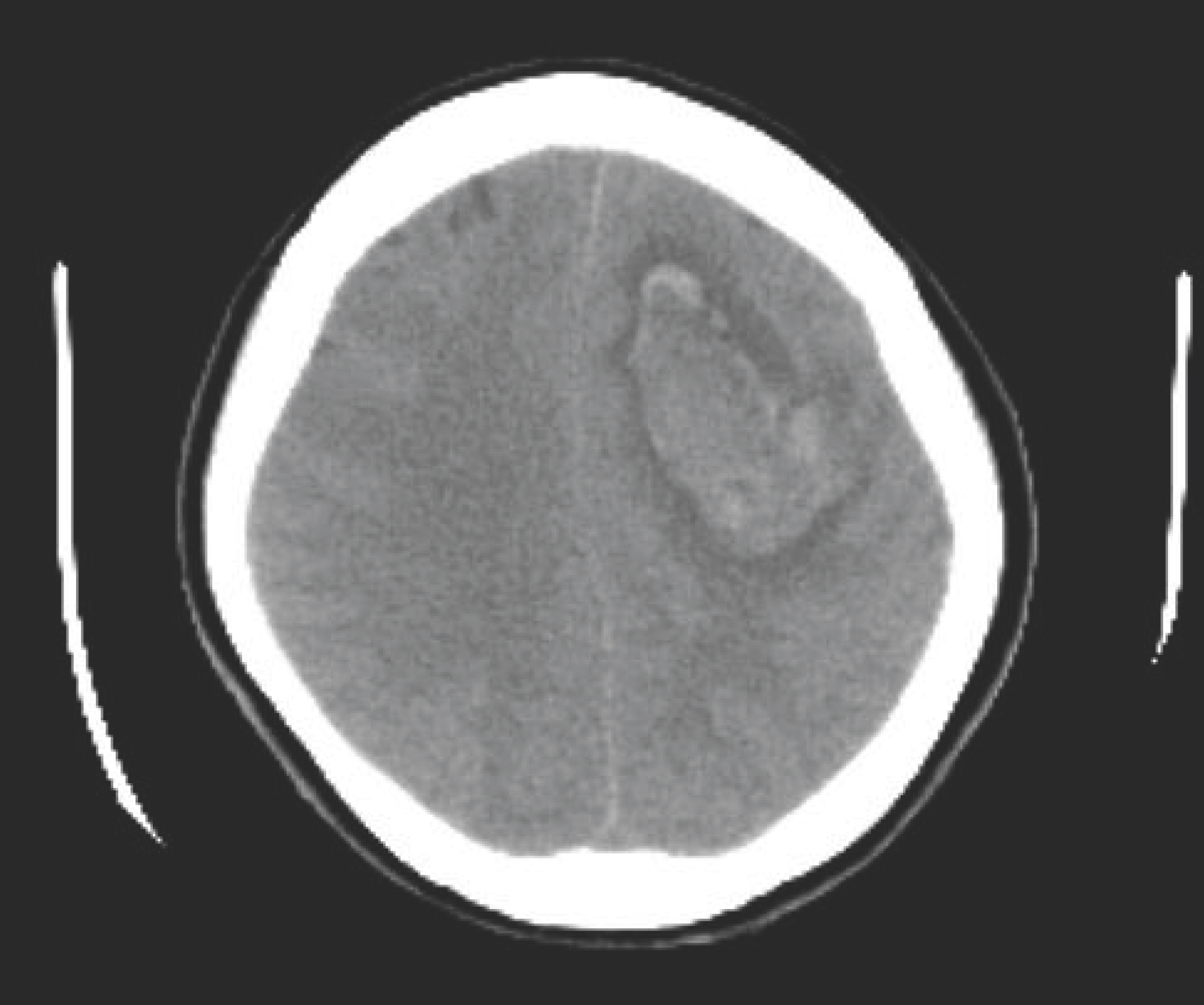
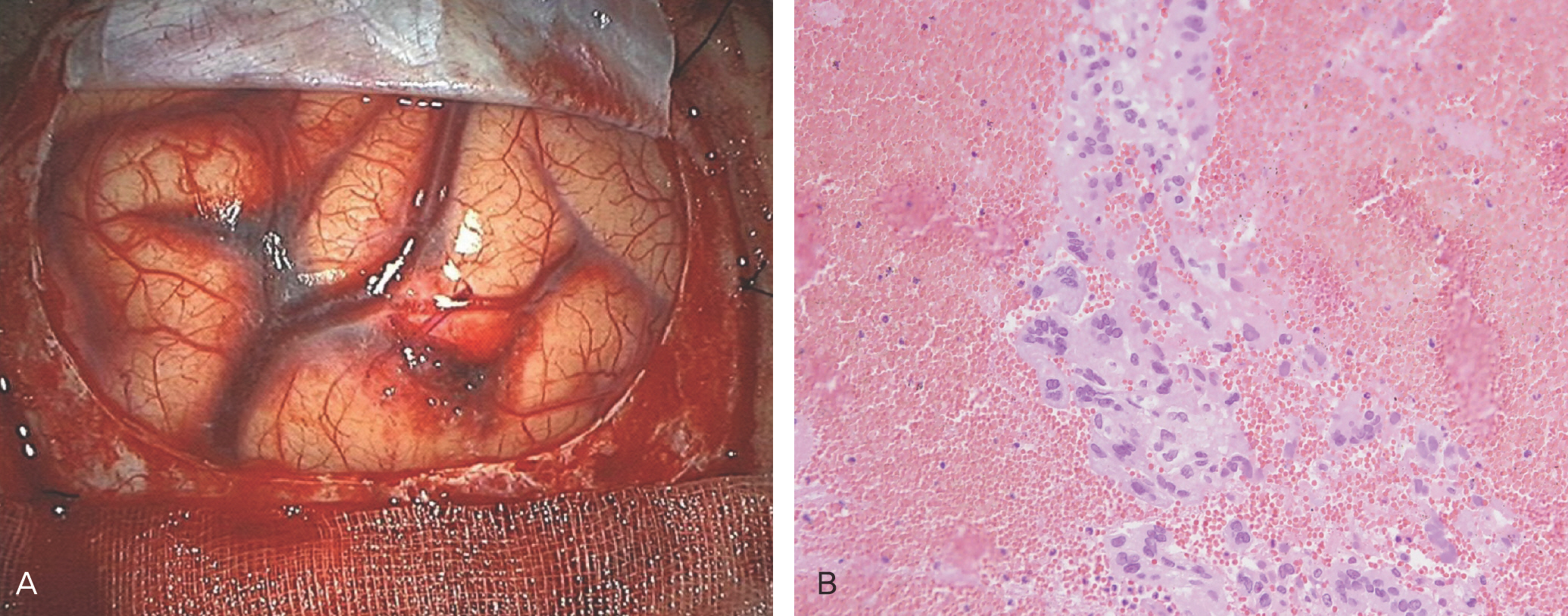
- Gestational trophoblastic neoplasm includes tumor spectrum of four entities: hydatidiform mole (complete and partial), invasive mole, choriocarcinoma and placental site trophoblastic tumor. The hydatidiform mole is usually benign, but it is regarded as a pre-malignant disease. The other three conditions are malignant and are termed gestational trophoblastic tumor. Although most molar pregnancies behave in a benign fashion, metastatic tumors develop after complete molar pregnancy in 4% of patients. However, even when the disease is spread to many distal organs, it is highly curable with chemotherapy in most cases. We recently encountered an unusual case of metastatic gestational trophoblastic neoplasm following complete mole, presenting as spontaneous renal and cerebral hemorrhage with a fatal course.
Keyword
MeSH Terms
Figure
Reference
-
References
1. Seckl MJ, Sebire NJ, Berkowitz RS. Gestational trophoblastic disease. Lancet. 2010; 376:717–29.
Article2. Martin BH, Kim JH. Changes in gestational trophoblastic tumors over four decades. A Korean experience. J Reprod Med. 1998; 43:60–8.3. Lurain JR. Gestational trophoblastic disease I: epidemiology, pathology, clinical presentation and diagnosis of gestational trophoblastic disease, and management of hydatidiform mole. Am J Obstet Gynecol. 2010; 203:531–9.
Article4. Crawford RA, Newlands E, Rustin GJ, Holden L, A'Hern R, Bag-shawe KD. Gestational trophoblastic disease with liver metastases: the Charing Cross experience. Br J Obstet Gynaecol. 1997; 104:105–9.5. Carlini L, Villa A, Busci L, Trezzi G, Agazzi R, Frigerio L. Selective uterine artery embolization: a new therapeutic approach in a patient with low-risk gestational trophoblastic disease. Am J Obstet Gynecol. 2006; 195:314–5.
Article6. Pearl ML, Braga CA. Percutaneous transcatheter embolization for control of life-threatening pelvic hemorrhage from gestational trophoblastic disease. Obstet Gynecol. 1992; 80:571–4.7. Takemura M, Yamasaki M, Tanaka F, Shimizu H, Okamoto E, Hisamatu K, et al. Transcatheter arterial embolization in the management of gynecological neoplasms. Gynecol Oncol. 1989; 34:38–42.
Article8. Moodley M, Moodley J. Transcatheter angiographic embolization for the control of massive pelvic hemorrhage due to gestational trophoblastic disease: a case series and review of the literature. Int J Gynecol Cancer. 2003; 13:94–7.
Article9. Keepanasseril A, Suri V, Prasad GR, Gupta V, Bagga R, Aggarwal N, et al. Management of massive hemorrhage in patients with gestational trophoblastic neoplasia by angiographic embolization: a safer alternative. J Reprod Med. 2011; 56:235–40.10. Lim AK, Agarwal R, Seckl MJ, Newlands ES, Barrett NK, Mitchell AW. Embolization of bleeding residual uterine vascular malformations in patients with treated gestational trophoblastic tumors. Radiology. 2002; 222:640–4.
Article11. Berkowitz RS, Goldstein DP. Gestational trophoblastic disease. Berek JS, Novak E, editors. editors.Berek & Novak's gynecology. 14th ed.Philadelphia (PA): Lippincott Williams & Wilkins;2007. p. 1581–604.12. Li MC. Trophoblastic disease: natural history, diagnosis, and treatment. Ann Intern Med. 1971; 74:102–12.
Article13. Lal A, Singhal M, Kumar S, Bag S, Singh SK, Khandelwal N. Bilateral renal and jejunal metastasis of choriocarcinoma presenting as spontaneous renal hemorrhage. Cancer Imaging. 2009; 9:56–8.
Article14. Lurain JR, Brewer JI, Mazur MT, Torok EE. Fatal gestational trophoblastic disease: an analysis of treatment failures. Am J Obstet Gynecol. 1982; 144:391–5.
Article15. Lok CA, Reekers JA, Westermann AM, Van der Velden J. Embolization for hemorrhage of liver metastases from choriocarcinoma. Gynecol Oncol. 2005; 98:506–9.
Article16. Menczer J, Modan M, Serr DM. Prospective follow-up of patients with hydatidiform mole. Obstet Gynecol. 1980; 55:346–9.
Article17. Genest DR, Laborde O, Berkowitz RS, Goldstein DP, Bernstein MR, Lage J. A clinicopathologic study of 153 cases of complete hydatidiform mole (1980–1990): histologic grade lacks prognostic significance. Obstet Gynecol. 1991; 78:402–9.18. Flam F, Hambraeus-Jonzon K, Hansson LO, Kjaeldgaard A. Hydatidiform mole with non-metastatic pulmonary complications and a false low level of hCG. Eur J Obstet Gynecol Reprod Biol. 1998; 77:235–7.
Article19. Cole LA, Butler SA, Khanlian SA, Giddings A, Muller CY, Seckl MJ, et al. Gestational trophoblastic diseases: 2. Hyperglycosyl-ated hCG as a reliable marker of active neoplasia. Gynecol Oncol. 2006; 102:151–9.
Article20. Cole LA, Khanlian SA, Muller CY, Giddings A, Kohorn E, Berkowitz R. Gestational trophoblastic diseases: 3. Human chorionic gonadotropin-free beta-subunit, a reliable marker of placental site trophoblastic tumors. Gynecol Oncol. 2006; 102:160–4.21. O'Reilly SM, Rustin GJ. Mismanagement of choriocarcinoma due to a false low HCG measurement. Int J Gynecol Cancer. 1993; 3:186–8.22. Levavi H, Neri A, Bar J, Regev D, Nordenberg J, Ovadia J. “Hook effect” in complete hydatidiform molar pregnancy: a falsely low level of beta-HCG. Obstet Gynecol. 1993; 82:720–1.23. Hoffman KL. Optimization of sandwich immunometric assay. J Clin Immunoassay. 1985; 8:237–44.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Metastatic gestational trophoblastic tumor presenting as spontaneous kidney rupture: Treatment with embolization
- A Case of Persistent Metastatic Gestational Trophoblastic Disease after Partial Hydatidiform Mole
- Malignant gestational trophobalstic tumor with markedly elevated serum hCG levels and negative urine hCG level
- A Case of Metastatic Choriocarcinoma with Uterine Perforation following Term Pregnancy
- A Case of Persistent Gestational Trophoblastic Disease after Complete Hydatidiform Mole