Korean J Pain.
2017 Oct;30(4):265-271. 10.3344/kjp.2017.30.4.265.
A hybrid cardiac rehabilitation is as effective as a hospital-based program in reducing chest pain intensity and discomfort
- Affiliations
-
- 1Cardiac Rehabilitation Center, Imam Ali Hospital, Kermanshah University of Medical Sciences, Kermanshah, Iran.
- 2Clinical Research Development Center, Imam Reza Hospital, Kermanshah University of Medical Sciences, Kermanshah, Iran. S_komasi63@yahoo.com
- 3Department of Human Genetics, Punjabi University, Patiala, India.
- KMID: 2392903
- DOI: http://doi.org/10.3344/kjp.2017.30.4.265
Abstract
- BACKGROUND
Health care services effort to provide alternative cardiac rehabilitation (CR) models to serve patients according to their preferences and needs. So, the present study aimed to assess and compare the effects of hospital-based and hybrid CR programs on chest pain intensity and discomfort in cardiac surgery patients.
METHODS
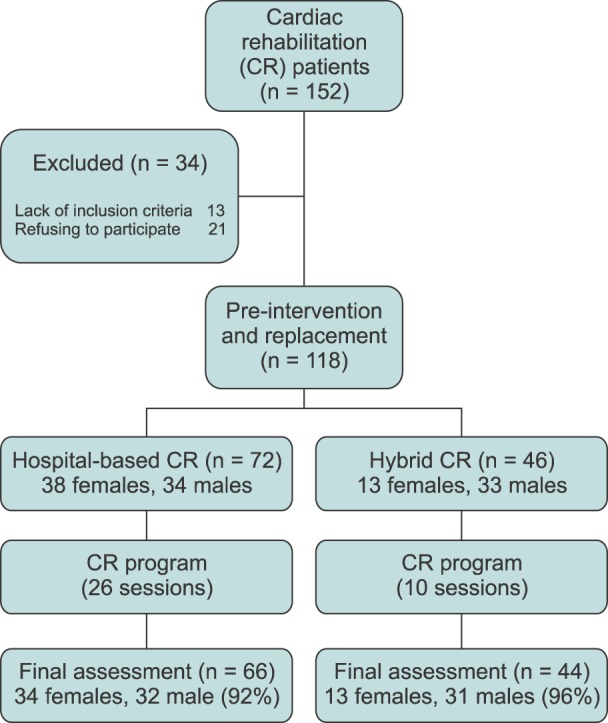
In this prospective study, 110 cardiac surgery patients were invited to the CR department of a hospital in the western part of Iran between March and July 2016. Patients were divided into two groups: hospital-based and hybrid CR. The hospital-based program included 26 sessions, and the hybrid program included 10 training sessions and exercise. The Brief Pain Inventory and Pain Discomfort Scale were used as research instrument, and data were analyzed using the paired t-test and ANCOVA.
RESULTS
The results indicated that both hospital-based and hybrid CR are effective in reducing the chest pain intensity and discomfort of cardiac surgery patients (P < 0.05). In addition, the comparison of scores before and after treatment using ANCOVA shows that no significant differences were observed between the two programs (P > 0.05).
CONCLUSIONS
Traditional hospital-based CR delivery is still the first choice for treatment in developing countries. However, hybrid CR is as effective as a hospital-based program in reducing pain components and it includes only 38% of the total cost in comparison to hospital-based delivery. So, we recommend using hybrid CR according with the recommendations of American Heart Association about using CR for the management of angina symptoms.
Keyword
MeSH Terms
Figure
Reference
-
1. Williams MA, Kaminsky LA. Healthy lifestyle medicine in the traditional healthcare environment-primary care and cardiac rehabilitation. Prog Cardiovasc Dis. 2017; 59:448–454. PMID: 28163014.
Article2. Komasi S, Saeidi M, Ezzati P, Amirian J. How can we deliver outpatient cardiac rehabilitation services to all low-risk patients in Iran. Res Cardiovasc Med. 2017; 6:e43585.3. Komasi S, Saeidi M. Hybrid cardiac rehabilitation as an alternative to common hospital-based cardiac rehabilitation in Iran: an appropriate model for the Iranian health system limitations, culture, and patients. Res Cardiovasc Med. 2017; 6:e39367.
Article4. Clark RA, Conway A, Poulsen V, Keech W, Tirimacco R, Tideman P. Alternative models of cardiac rehabilitation: a systematic review. Eur J Prev Cardiol. 2015; 22:35–74. PMID: 23943649.
Article5. Korzeniowska-Kubacka I, Dobraszkiewicz-Wasilewska B, Bilińska M, Rydzewska E, Piotrowicz R. Two models of early cardiac rehabilitation in male patients after myocardial infarction with preserved left ventricular function: comparison of standard out-patient versus hybrid training programmes. Kardiol Pol. 2011; 69:220–226. PMID: 21432787.6. Korzeniowska-Kubacka I, Bilińska M, Dobraszkiewicz-Wasilewska B, Piotrowicz R. Hybrid model of cardiac rehabilitation in men and women after myocardial infarction. Cardiol J. 2015; 22:212–218. PMID: 25588535.
Article7. Najafi F, Nalini M. Hospital-based versus hybrid cardiac rehabilitation program in coronary bypass surgery patients in western Iran: effects on exercise capacity, risk factors, psychological factors, and quality of life. J Cardiopulm Rehabil Prev. 2015; 35:29–36. PMID: 25402170.
Article8. Strand E, Pedersen ER, Svingen GF, Olsen T, Bjørndal B, Karlsson T, et al. Serum acylcarnitines and risk of cardiovascular death and acute myocardial infarction in patients with stable angina pectoris. J Am Heart Assoc. 2017; 6:e003620. PMID: 28159823.
Article9. Babu AS, Noone MS, Narayanan SM, Franklin BA. Exercise based cardiac rehabilitation for unstable angina: a case report. Oman Med J. 2012; 27:e034. PMID: 28861188.
Article10. Piestrzeniewicz K, Navarro-Kuczborska N, Bolińska H, Jegier A, Maciejewski M. The impact of comprehensive cardiac rehabilitation in patients up to 55 years old after acute myocardial infarction treated with primary coronary intervention. Pol Arch Med Wewn. 2004; 111:309–317. PMID: 15230212.11. Asbury EA, Webb CM, Probert H, Wright C, Barbir M, Fox K, et al. Cardiac rehabilitation to improve physical functioning in refractory angina: a pilot study. Cardiology. 2012; 122:170–177. PMID: 22846707.
Article12. American College of Sports Medicine. ACSM's guidelines for exercise testing and prescription. 7th ed. Philadelphia (PA): Lippincott Williams & Wilkins;2006.13. Mirzamani SM, Sadidi A, Salimi SH, Besharat MA. Validation of the Persian version of the brief pain inventory. Acta Med Iran. 2005; 43:425–428.14. Jensen MP, Karoly P, Harris P. Assessing the affective component of chronic pain: development of the pain discomfort scale. J Psychosom Res. 1991; 35:149–154. PMID: 2046049.
Article15. Pallant J. SPSS survival manual: a step by step guide to data analysis using SPSS for windows (version 12). 2nd ed. Crows Nest: Allen & Unwin;2005. p. 142–152.16. Nytrøen K, Gullestad L. Exercise after heart transplantation: an overview. World J Transplant. 2013; 3:78–90. PMID: 24392312.
Article17. Fletcher GF, Balady GJ, Amsterdam EA, Chaitman B, Eckel R, Fleg J, et al. Exercise standards for testing and training: a statement for healthcare professionals from the American Heart Association. Circulation. 2001; 104:1694–1740. PMID: 11581152.18. Heydarpour B, Saeidi M, Ezzati P, Soroush A, Komasi S. Sociodemographic predictors in failure to complete outpatient cardiac rehabilitation. Ann Rehabil Med. 2015; 39:863–871. PMID: 26798599.
Article19. Mazumdar S, Kumar A, Verma SK. Effect of cardiac rehabilitation on blood pressure in stable angina patients. J Exerc Sci Physiother. 2014; 10:54–59.
Article20. Moore RK, Groves D, Bateson S, Barlow P, Hammond C, Leach AA, et al. Health related quality of life of patients with refractory angina before and one year after enrolment onto a refractory angina program. Eur J Pain. 2005; 9:305–310. PMID: 15862480.
Article21. Moore R, Groves D, Hammond C, Leach A, Chester MR. Temporary sympathectomy in the treatment of chronic refractory angina. J Pain Symptom Manage. 2005; 30:183–191. PMID: 16125034.
Article22. Furze G. Angina rehabilitation: exercise is not enough. Procedia Soc Behav Sci. 2010; 5:1545–1549.
Article23. Moradi B, Maleki M, Esmaeilzadeh M, Abkenar HB. Physician-related factors affecting cardiac rehabilitation referral. J Tehran Heart Cent. 2011; 6:187–192. PMID: 23074367.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Irrational beliefs predict pain/discomfort and emotional distress as a result of pain in patients with non-cardiac chest pain
- Reducing Irrational Beliefs and Pain Severity in Patients Suffering from Non-Cardiac Chest Pain (NCCP): A Comparison of Relaxation Training and Metaphor Therapy
- Cardiovascular Complications during Cardiac Exercise Program
- The Effect of Home-Based Cardiac Rehabilitation on Cardiovascular Risk Factors Management
- Determinants of depression in non-cardiac chest pain patients: a cross sectional study