Baseline Characteristics of a Retrospective Patient Cohort in the Korean Vascular Intervention Society Endovascular Therapy in Lower Limb Artery Diseases (K-VIS ELLA) Registry
- Affiliations
-
- 1Division of Cardiology, Department of Internal Medicine, Severance Cardiovascular Hospital, Yonsei University College of Medicine, Seoul, Korea. cdhlyj@yuhs.ac
- 2Division of Cardiology, Department of Internal Medicine, Gangnam Severance Hospital, Yonsei University College of Medicine, Seoul, Korea.
- 3Division of Cardiology, Department of Internal Medicine, Chungnam National University Hospital, Daejeon, Korea.
- 4Seoul National University Bundang Hospital, Seongnam, Korea.
- 5Division of Cardiology, Department of Internal Medicine, Korea University Anam Hospital, Seoul, Korea.
- 6Division of Cardiology, Department of Internal Medicine, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea.
- 7Division of Cardiology, Department of Internal Medicine, Chonbuk National University Hospital, Jeonju, Korea.
- 8Division of Cardiology, Department of Medicine, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea.
- 9Division of Cardiology, Department of Internal Medicine, Seoul St. Mary's Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea.
- KMID: 2392884
- DOI: http://doi.org/10.4070/kcj.2017.0020
Abstract
- BACKGROUND AND OBJECTIVES
The Korean Vascular Intervention Society Endovascular Therapy in Lower Limb Artery Diseases (K-VIS ELLA) Registry is a multicenter observational study with retrospective and prospective cohorts of patients with lower extremity peripheral artery disease (PAD) undergoing endovascular treatment. In this study, we report the baseline characteristics of this retrospective cohort.
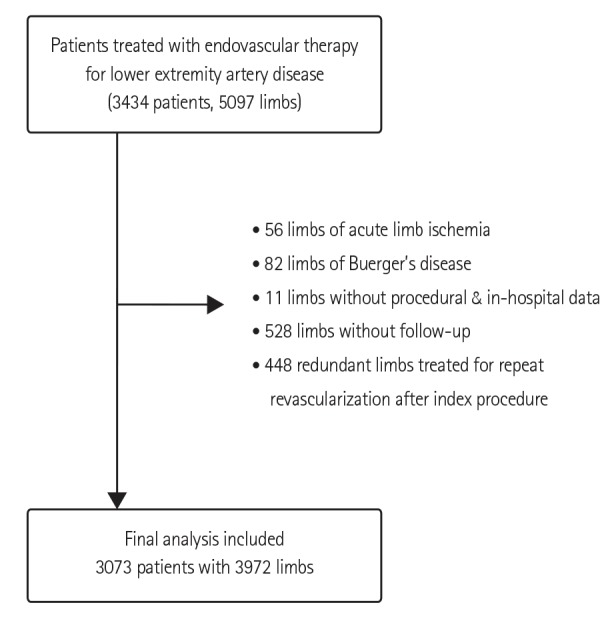
SUBJECTS AND METHODS
In the present study we analyzed datasets of 3073 patients with 3972 target limbs from a retrospective cohort treated with endovascular therapy in 31 Korean hospitals. Data regarding patient baseline clinical and lesion characteristics and postintervention medications were collected from electronic medical records.
RESULTS
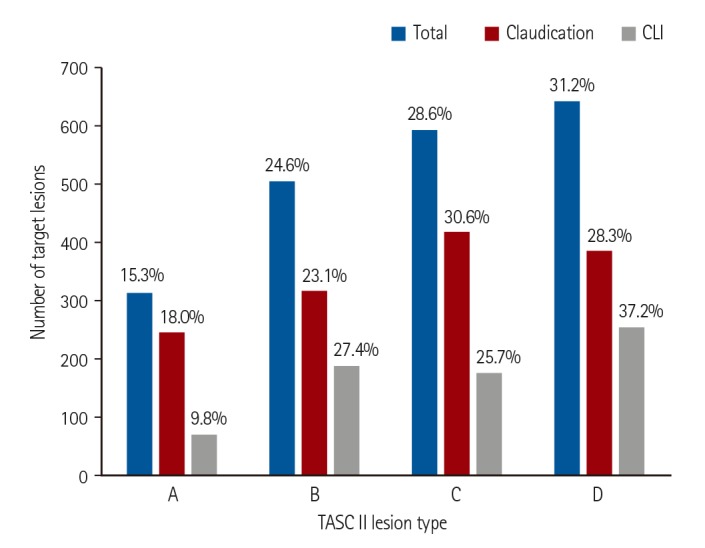
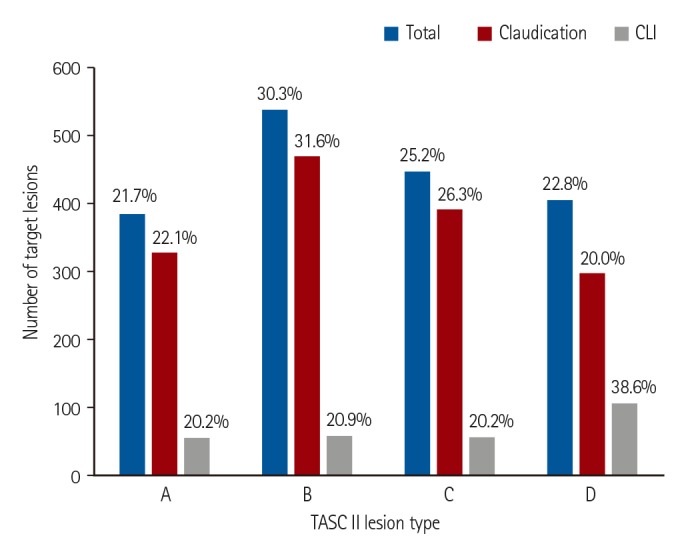
The mean patient age was 68.3±9.4 years. The majority were male (82.1%) with comorbidities such as diabetes mellitus (58.0%), hypertension (73.4%), and coronary artery disease (CAD; 55.3%). Patients more commonly presented with intermittent claudication (66.3%) than with critical limb ischemia (CLI; 33.7%). Femoropopliteal artery (41.2%) was the most common target vessel for endovascular treatment, followed by the aortoiliac (35.6%) and infrapopliteal arteries (23.2%). TransAtlantic Inter-Society Consensus for the Management of Peripheral Artery Disease (TASC II) type C/D aortoiliac (48.0%) or femoropopliteal lesions (60.2%) were frequent targets of endovascular treatment. At hospital discharge, only 73.1% of patients received dual antiplatelet therapy and 69.2% received a statin.
CONCLUSION
The majority of Korean patients with PAD exhibited conventional risk factors, such as male sex, older age, diabetes, and hypertension with coexisting CAD. Complex lesions were frequently treated with endovascular therapy. However, the rate of adherence to guidelines regarding post-procedural medical treatment requires improvement.
MeSH Terms
-
Arteries*
Cohort Studies*
Comorbidity
Consensus
Coronary Artery Disease
Dataset
Diabetes Mellitus
Electronic Health Records
Extremities
Humans
Hydroxymethylglutaryl-CoA Reductase Inhibitors
Hypertension
Intermittent Claudication
Ischemia
Lower Extremity*
Male
Observational Study
Peripheral Arterial Disease
Prospective Studies
Retrospective Studies*
Risk Factors
Figure
Cited by 9 articles
-
Treatment of Femoropopliteal Artery In-stent Restenosis
Wonho Kim, Donghoon Choi
Korean Circ J. 2018;48(3):191-197. doi: 10.4070/kcj.2018.0074.SFA Intervention: Intraluminal or Subintimal?
Young-Guk Ko
Korean Circ J. 2018;48(8):685-691. doi: 10.4070/kcj.2018.0216.Elucidation of the Diagnosis and Treatment of Peripheral Arterial Disease
Hyung Oh Kim, Weon Kim
Korean Circ J. 2018;48(9):826-827. doi: 10.4070/kcj.2018.0155.Korean Multicenter Registry Study of EPIC Stents for the Treatment of Iliac Artery Disease: K-EPIC Registry
Dae-Young Kim, Young-Guk Ko, Seung-Jun Lee, Chul-Min Ahn, Seung-Woon Rha, Cheol Ung Choi, Jong Kwan Park, Chang-Hwan Yoon, Seung-Hyuk Choi, Pil-Ki Min, Jang-Whan Bae, Jung-Kyu Han, Sang Ho Park, Donghoon Choi
Korean Circ J. 2021;51(5):441-451. doi: 10.4070/kcj.2020.0420.Association between Body Mass Index and Clinical Outcomes of Peripheral Artery Disease after Endovascular Therapy: Data from K-VIS ELLA Registry
Chewan Lim, Hoyoun Won, Young-Guk Ko, Seung-Jun Lee, Chul-Min Ahn, Pil-Ki Min, Jae-Hwan Lee, Chang-Hwan Yoon, Cheol Woong Yu, Seung Whan Lee, Sang-Rok Lee, Seung Hyuk Choi, In-Ho Chae, Donghoon Choi,
Korean Circ J. 2021;51(8):696-707. doi: 10.4070/kcj.2021.0040.Clinical Outcomes of Atherectomy Plus Drug-coated Balloon Versus Drug-coated Balloon Alone in the Treatment of Femoropopliteal Artery Disease
Jung-Joon Cha, Jae-Hwan Lee, Young-Guk Ko, Jae-Hyung Roh, Yong-Hoon Yoon, Yong-Joon Lee, Seung-Jun Lee, Sung-Jin Hong, Chul-Min Ahn, Jung-Sun Kim, Byeong-Keuk Kim, Donghoon Choi, Myeong-Ki Hong, Yangsoo Jang
Korean Circ J. 2021;52(2):123-133. doi: 10.4070/kcj.2021.0246.Long-term Clinical Outcomes and Prognostic Factors After Endovascular Treatment in Patients With Chronic Limb Threatening Ischemia
Jung-Joon Cha, Jong-Youn Kim, Hyoeun Kim, Young-Guk Ko, Donghoon Choi, Jae-Hwan Lee, Chang-Hwan Yoon, In-Ho Chae, Cheol Woong Yu, Seung Whan Lee, Sang-Rok Lee, Seung Hyuk Choi, Yoon Seok Koh, Pil-Ki Min,
Korean Circ J. 2022;52(6):429-440. doi: 10.4070/kcj.2021.0342.Endovascular Therapy for Complex Iliac Lesions: There Is Much More to Be Defined
Yahya Alansari, Pil Hyung Lee
Korean Circ J. 2022;52(7):541-543. doi: 10.4070/kcj.2022.0145.Long-Term Clinical Outcomes of Iliac Artery Endovascular Therapy in the Korean Vascular Intervention Society Endovascular Therapy in Lower Limb Artery Diseases (K-VIS ELLA) Registry
Ji Woong Roh, Sanghoon Shin, Young-Guk Ko, Nak-Hoon Son, Chul-Min Ahn, Pil-Ki Min, Jae-Hwan Lee, Chang-Hwan Yoon, Cheol Woong Yu, Seung Whan Lee, Sang-Rok Lee, Seung Hyuk Choi, In-Ho Chae, Donghoon Choi
Korean Circ J. 2022;52(7):529-540. doi: 10.4070/kcj.2021.0390.
Reference
-
1. Norgren L, Hiatt WR, Dormandy JA, et al. Inter-society consensus for the management of peripheral arterial disease (TASC II). J Vasc Surg. 2007; 45(Suppl S):S5–S67. PMID: 17223489.2. European Stroke Organisation. Tendera M, Aboyans V, et al. ESC guidelines on the diagnosis and treatment of peripheral artery diseases: document covering atherosclerotic disease of extracranial carotid and vertebral, mesenteric, renal, upper and lower extremity arteries: the task force on the diagnosis and treatment of peripheral artery diseases of the European Society of Cardiology (ESC). Eur Heart J. 2011; 32:2851–2906. PMID: 21873417.3. Hirsch AT, Haskal ZJ, Hertzer NR, et al. ACC/AHA 2005 practice guidelines for the management of patients with peripheral arterial disease (lower extremity, renal, mesenteric, and abdominal aortic): a collaborative report from the American Association for Vascular Surgery/Society for Vascular Surgery, Society for Cardiovascular Angiography and Interventions, Society for Vascular Medicine and Biology, Society of Interventional Radiology, and the ACC/AHA task force on practice guidelines (writing committee to develop guidelines for the management of patients with peripheral arterial disease): endorsed by the American Association of Cardiovascular and Pulmonary Rehabilitation; National Heart, Lung, and Blood Institute; Society for Vascular Nursing; TransAtlantic Inter-society Consensus; and Vascular Disease Foundation. Circulation. 2006; 113:e463–e654. PMID: 16549646.4. Bhatt DL, Steg PG, Ohman EM, et al. International prevalence, recognition, and treatment of cardiovascular risk factors in outpatients with atherothrombosis. JAMA. 2006; 295:180–189. PMID: 16403930.5. Heald CL, Fowkes FG, Murray GD, Price JF. Ankle Brachial Index Collaboration. Risk of mortality and cardiovascular disease associated with the ankle-brachial index: systematic review. Atherosclerosis. 2006; 189:61–69. PMID: 16620828.6. Park YY, Joh JH, Han SA, et al. National trends for the treatment of peripheral arterial disease in Korea between 2004 and 2013. Ann Surg Treat Res. 2015; 89:319–324. PMID: 26665127.7. Rutherford RB, Baker JD, Ernst C, et al. Recommended standards for reports dealing with lower extremity ischemia: revised version. J Vasc Surg. 1997; 26:517–538. PMID: 9308598.8. World Health Organization. Nutritional anemia. Report of a WHO scientific group. World Health Organ Tech Rep Ser. 1968; 405:5–37. PMID: 4975372.9. Kim MH, Ahn S, Kim JY, Jun KW, Yun SS, Won YS. Current trends of major arterial diseases in Korea: based on data from the health insurance review and assessment service. Ann Surg Treat Res. 2016; 90:218–223. PMID: 27073793.10. Howard DP, Banerjee A, Fairhead JF, et al. Population-based study of incidence, risk factors, outcome, and prognosis of ischemic peripheral arterial events: implications for prevention. Circulation. 2015; 132:1805–1815. PMID: 26350058.11. Farber A, Eberhardt RT. The current state of critical limb ischemia: a systematic review. JAMA Surg. 2016; 151:1070–1077. PMID: 27551978.12. Iida O, Nakamura M, Yamauchi Y, et al. Endovascular treatment for infrainguinal vessels in patients with critical limb ischemia: OLIVE registry, a prospective, multicenter study in Japan with 12-month follow-up. Circ Cardiovasc Interv. 2013; 6:68–76. PMID: 23362307.13. Soga Y, Mii S, Iida O, et al. Propensity score analysis of clinical outcome after bypass surgery vs. endovascular therapy for infrainguinal artery disease in patients with critical limb ischemia. J Endovasc Ther. 2014; 21:243–253. PMID: 24754284.14. Agarwal S, Sud K, Shishehbor MH. Nationwide trends of hospital admission and outcomes among critical limb ischemia patients: from 2003-2011. J Am Coll Cardiol. 2016; 67:1901–1913. PMID: 27012780.15. Bisdas T, Borowski M, Stavroulakis K, Torsello G. CRITISCH Collaborators. Endovascular therapy versus bypass surgery as first-line treatment strategies for critical limb ischemia: results of the interim analysis of the CRITISCH registry. JACC Cardiovasc Interv. 2016; 9:2557–2565. PMID: 28007205.16. Sigvant B, Kragsterman B, Falkenberg M, et al. Contemporary cardiovascular risk and secondary preventive drug treatment patterns in peripheral artery disease patients undergoing revascularization. J Vasc Surg. 2016; 64:1009–1017.e3. PMID: 27209402.17. Westin GG, Armstrong EJ, Bang H, et al. Association between statin medications and mortality, major adverse cardiovascular event, and amputation-free survival in patients with critical limb ischemia. J Am Coll Cardiol. 2014; 63:682–690. PMID: 24315911.18. Harris SK, Roos MG, Landry GJ. Statin use in patients with peripheral arterial disease. J Vasc Surg. 2016; 64:1881–1888. PMID: 27871503.19. Heart Protection. Randomized trial of the effects of cholesterol-lowering with simvastatin on peripheral vascular and other major vascular outcomes in 20,536 people with peripheral arterial disease and other high-risk conditions. J Vasc Surg. 2007; 45:645–654. discussion 653-4. PMID: 17398372.20. Antoniou GA, Fisher RK, Georgiadis GS, Antoniou SA, Torella F. Statin therapy in lower limb peripheral arterial disease: systematic review and meta-analysis. Vascul Pharmacol. 2014; 63:79–87. PMID: 25446168.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Long-Term Clinical Outcomes of Iliac Artery Endovascular Therapy in the Korean Vascular Intervention Society Endovascular Therapy in Lower Limb Artery Diseases (K-VIS ELLA) Registry
- Association between Body Mass Index and Clinical Outcomes of Peripheral Artery Disease after Endovascular Therapy: Data from K-VIS ELLA Registry
- Catheter-Directed Thrombolysis for Persistent Sciatic Artery Presenting with Acute Limb Ischemia
- Endovascular treatment of acute limb ischemia due to thrombotic occlusion of the suprainguinal artery
- Endovascular Treatment of Iliac & Femoral Artery Occlusive Disease