Kosin Med J.
2016 Jun;31(1):56-65. 10.7180/kmj.2016.31.1.56.
Endovascular treatment of acute limb ischemia due to thrombotic occlusion of the suprainguinal artery
- Affiliations
-
- 1Division of Cardiology, Department of Internal Medicine, Dongguk University College of Medicine, Gyeongju-si, Gyeongsangbuk-do, Korea. junhodr@naver.com
- KMID: 2328718
- DOI: http://doi.org/10.7180/kmj.2016.31.1.56
Abstract
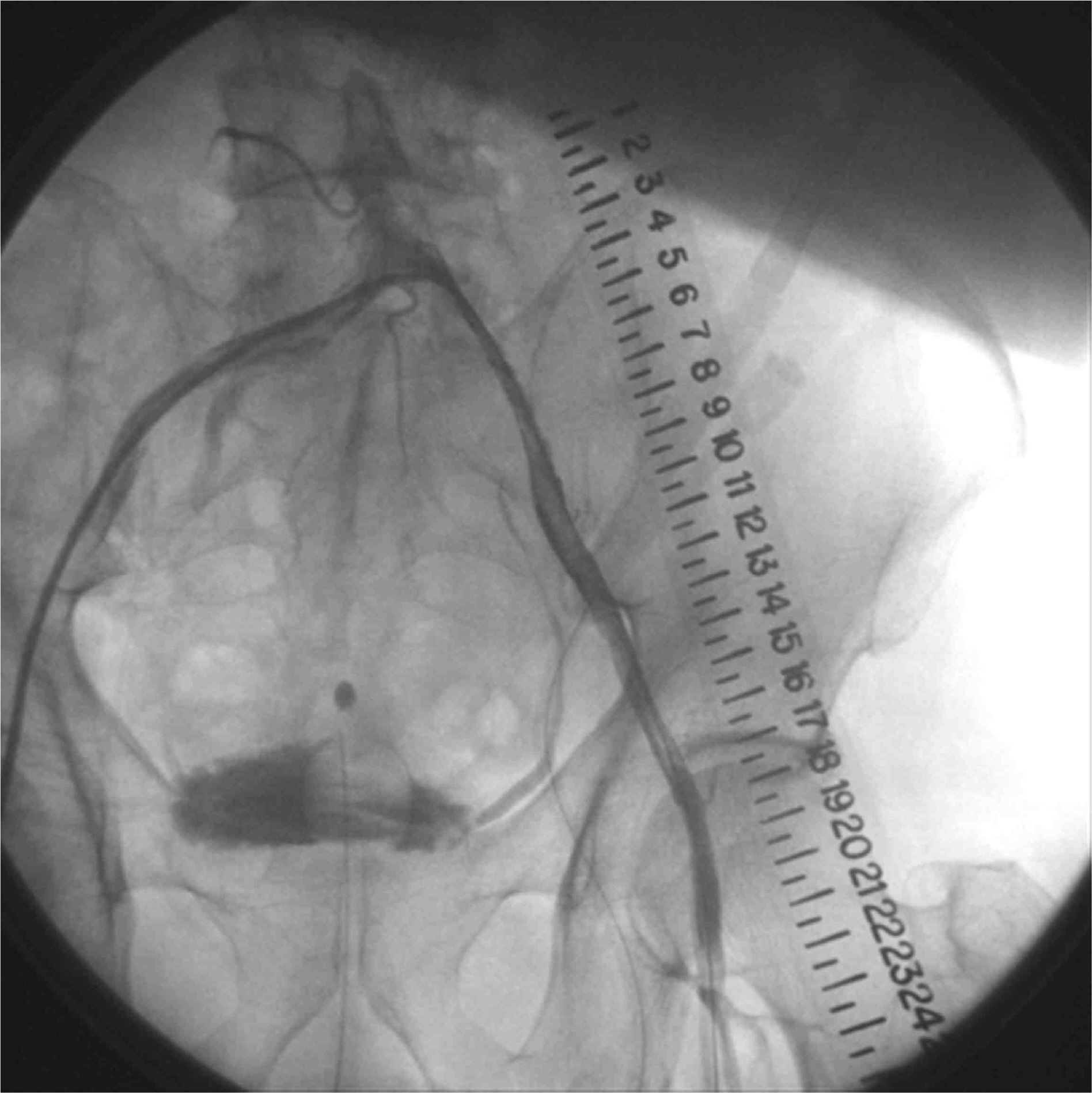
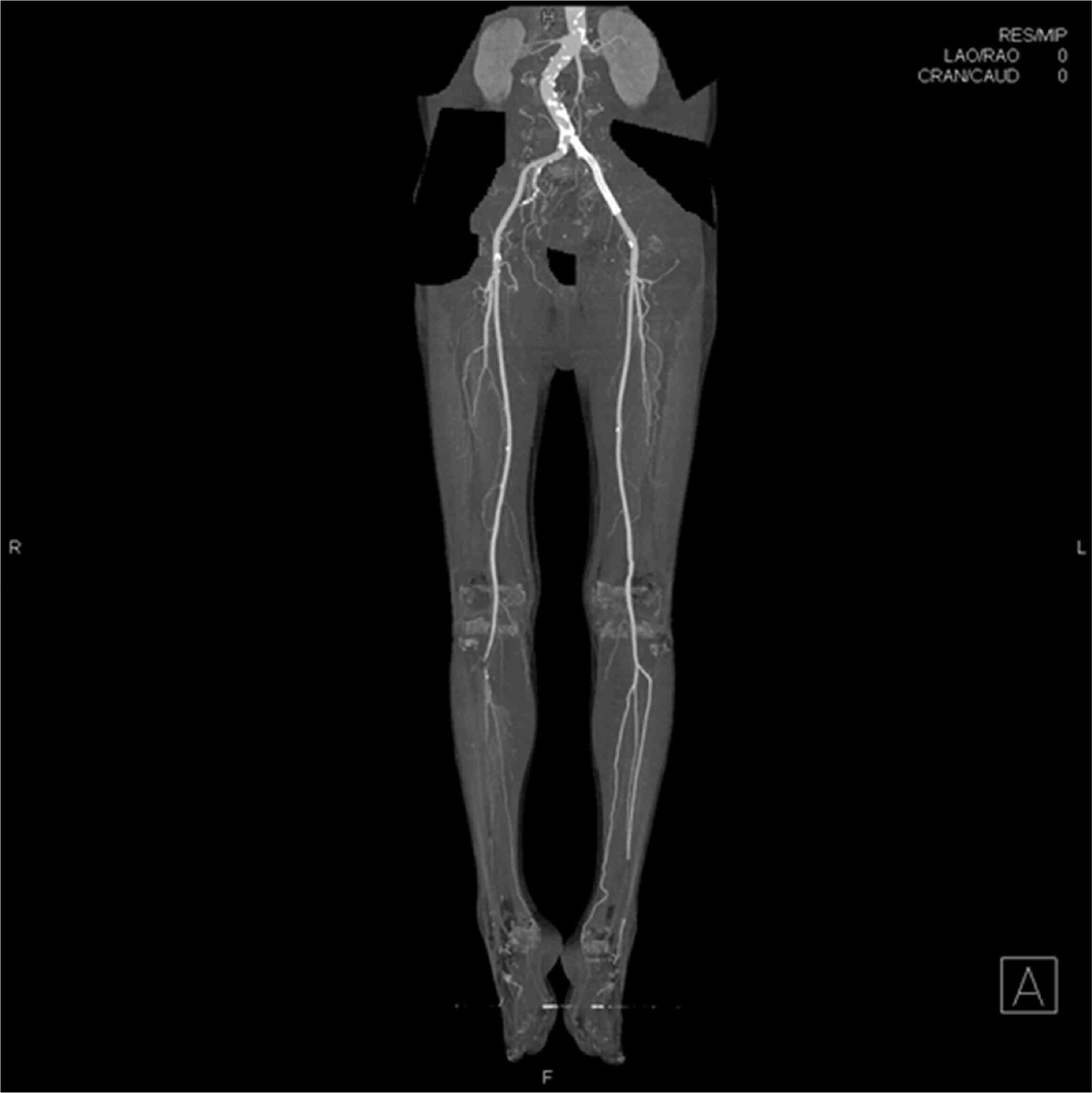
- Acute limb ischemia (ALI) is a serious condition requiring prompt intervention due to a sudden decrease in limb perfusion threatening limb viability. Treatment of ALI depends on the clinical status of the affected limb and patient comorbidities. Surgical therapy has been the historical standard of care for restoring limb perfusion; however, percutaneous endovascular intervention has been shown to be a promising treatment option in selected patients of ALI at high surgical risk. We report on a case of a 75-year-old man with ALI caused by thrombotic occlusion of the suprainguinal artery, successfully treated with endovascular therapy including stent insertion and thrombus aspiration and catheter-directed urokinase infusion in view of the clinical findings and imaging studies.
MeSH Terms
Figure
Reference
-
References
1. Norgren L, Hiatt WR, Dormandy JA, Nehler MR, Harris KA, Fowkes FG, et al. Inter-society consensus for the management of peripheral arterial disease (TASC II). J Vasc Surg. 2007; 45:S5–67.
Article2. Hirsch AT, Haskal ZJ, Hertzer NR, Bakal CW, Creager MA, Halperin JL, et al. ACC/AHA 2005 practice guidelines for the management of patients with peripheral arterial disease (lower extremity, renal, mesenteric, and abdominal aortic): a collaborative report from the American Association for Vascular Surgery/Society for Vascular Surgery, Society for Cardiovascular Angiography and Interventions, Society for Vascular Medicine and Biology, Society of Interventional Radiology. Circulation. 2006; 113:e463–654.
Article3. Creager MA, Kaufman JA, Conte MS. Acute limb ischemia. N Engl J Med. 2012; 366:2198–206.
Article4. Dormandy J, Heeck L, Vig S. Acute limb ischemia. Semin Vasc Surg. 1999; 12:148–53.5. Walker TG. Acute Limb Ischemia. Tech Vasc Interv Radiol. 2009; 12:117–29.
Article6. Costantini V, Lenti M. Treatment of acute occlusion of peripheral arteries. Thromb Res. 2002; 106:V285–94.
Article7. Lowe GD. Common risk factors for both arterial and venous thrombosis. Br J Haematol. 2008; 140:488–95.
Article8. Franchini M, Mannucci PM. Association between venous and arterial thrombosis: clinical implications. Eur J Intern Med. 2012; 23:333–7.
Article9. Patel NH, Krishnamurthy VN, Kim S, Saad WE, Ganguli S, Gregory Walker T, et al. Quality improvement guidelines for percutaneous management of acute lower-extremity ischemia. J Vasc Interv Radiol. 2013; 24:3–15.
Article10. Rutherford RB, Baker JD, Ernst C, Johnston KW, Porter JM, Ahn S, et al. Recommended standards for reports dealing with lower extremity ischemia: revised version. J Vasc Surg. 1997; 26:517–38.
Article11. Ouriel K, Veith FJ, Sasahara AA. A comparison of recombinant urokinase with vascular surgery as initial treatment for acute arterial occlusion of the legs. N Engl J Med. 1998; 338:1105–11.
Article12. Karnabatidis D, Spiliopoulos S, Tsetis D, Siablis D. Quality improvement guidelines for percutaneous catheter-directed intra-arterial thrombolysis and mechanical thrombectomy for acute low-er-limb ischemia. Cardiovasc Intervent Radiol. 2011; 34:1123–36.
Article13. Cragg AH, Smith TP, Corson JD, Nakagawa N, Castaneda F, Kresowik TF, et al. Two urokinase dose regimens in native arterial and graft occlusions: Initial results of a prospective, randomized clinical trial. Radiology. 1991; 178:681–6.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Catheter-Directed Thrombolysis for Persistent Sciatic Artery Presenting with Acute Limb Ischemia
- Role of surgical treatment for peripheral arterial disease in endovascular era
- Successful Endovascular Therapy for Bilateral Popliteal Thrombotic Occlusions
- Acute Upper Limb Ischemia due to Cardiac Origin Thromboembolism: the Usefulness of Percutaneous Aspiration Thromboembolectomy via a Transbrachial Approach
- A novel hybrid technique to treat flush mesenteric arterial occlusion in acute-on-chronic mesenteric ischemia