Korean J Radiol.
2011 Oct;12(5):595-601. 10.3348/kjr.2011.12.5.595.
Acute Upper Limb Ischemia due to Cardiac Origin Thromboembolism: the Usefulness of Percutaneous Aspiration Thromboembolectomy via a Transbrachial Approach
- Affiliations
-
- 1Department of Radiology, Chonbuk National University Hospital & Medical School, Jeonbuk 561-712, Korea. kwak8140@chonbuk.ac.kr
- 2Department of Radiology and the Institute for Medical Science, Chonbuk National University Hospital & Medical School, Jeonbuk 561-712, Korea.
- KMID: 1116445
- DOI: http://doi.org/10.3348/kjr.2011.12.5.595
Abstract
OBJECTIVE
To evaluate the usefulness of percutaneous aspiration thromboembolectomy (PAT) via a transbrachial approach in patients with acute upper limb ischemia.
MATERIALS AND METHODS
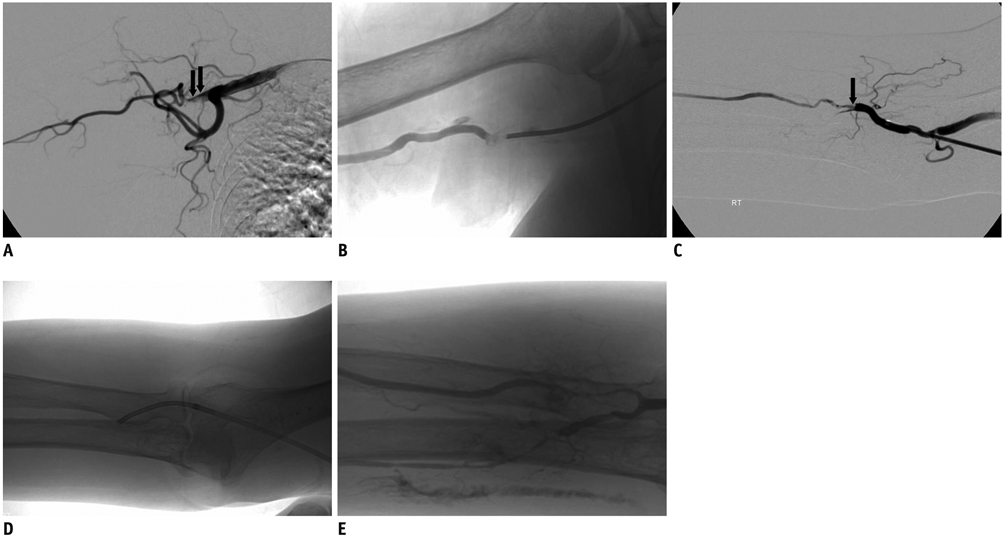
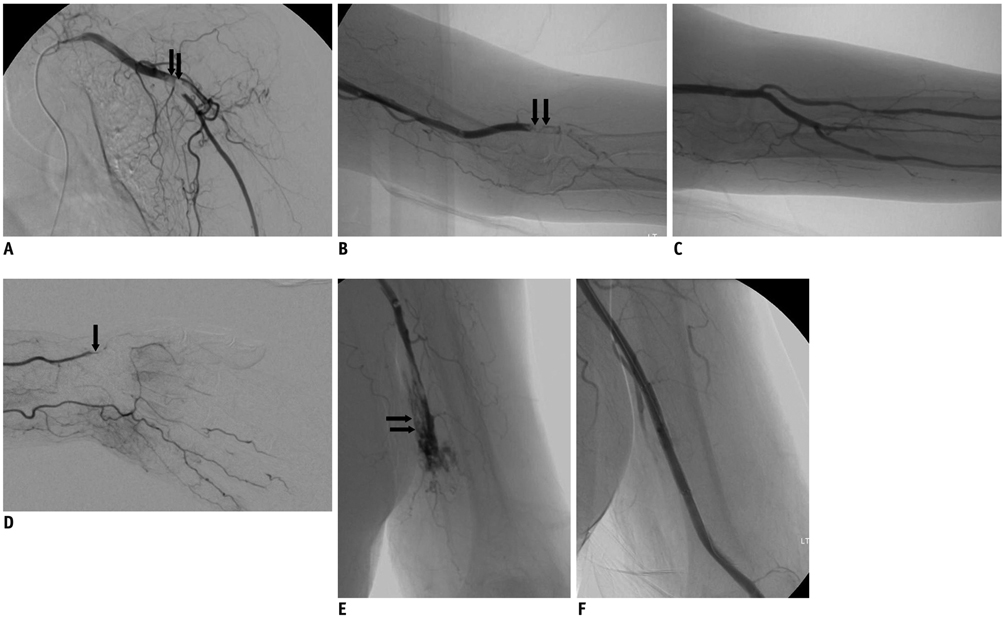
From July 2004 to March 2008, eleven patients with acute upper limb ischemia were enrolled in this study. They were initially treated with thrombolysis (n = 1), PAT (n = 6), or both (n = 4) via a femoral artery approach. However, all of the patients had residual thrombus in the brachial artery, which was subsequently managed by PAT via the transbrachial approach for removal of residual emboli.
RESULTS
Successful re-canalization after PAT via a transbrachial approach was achieved in all patients. Two patients experienced early complications: one experienced a massive hematoma of the upper arm due to incomplete compression and was treated by stent deployment. The other patient experienced a re-occlusion of the brachial artery the day after the procedure due to excessive manual compression of the puncture site, but did not show recurrence of ischemic symptoms in the artery of the upper arm. Clinical success with complete resolution of ischemic symptoms was achieved in all patients.
CONCLUSION
PAT via a transbrachial approach is a safe and effective treatment for patients with acute upper limb ischemia.
Keyword
MeSH Terms
-
Acute Disease
Aged
Aged, 80 and over
Arm/*blood supply
Atrial Fibrillation/complications
Axillary Artery
*Brachial Artery
*Catheterization, Peripheral
*Embolectomy/methods
*Endovascular Procedures
Female
Heart Failure/complications
Humans
Ischemia/*etiology
Male
Middle Aged
*Thrombectomy/methods
Thromboembolism/etiology/*therapy
Thrombolytic Therapy
Figure
Reference
-
1. Galbraith K, Collin J, Morris PJ, Wood RF. Recent experience with arterial embolism of the limbs in a vascular unit. Ann R Coll Surg Engl. 1985. 67:30–33.2. Thompson JE, Sigler L, Raut PS, Austin DJ, Patman RD. Arterial embolectomy: a 20 year experience with 163 cases. Surgery. 1970. 67:212–220.3. Fogarty TJ, Cranley JJ, Krause RJ, Strasser ES, Hafner CD. A method for extraction of arterial emboli and thrombi. Surg Gynecol Obstet. 1963. 116:241–244.4. Thompson JE. Acute peripheral arterial occlusions. N Engl J Med. 1974. 290:950–952.5. Schmidt FE, Hewitt RL. Severe upper limb ischemia. Arch Surg. 1980. 115:1188–1191.6. Ouriel K, Veith FJ, Sasahara AA. A comparison of recombinant urokinase with vascular surgery as initial treatment for acute arterial occlusion of the legs. Thrombolysis or Peripheral Arterial Surgery (TOPAS) Investigators. N Engl J Med. 1998. 338:1105–1111.7. Tepe G, Hopfenzitz C, Dietz K, Wiskirchen J, Heller S, Ouriel K, et al. Peripheral arteries: treatment with antibodies of platelet receptors and reteplase for thrombolysis--APART trial. Radiology. 2006. 239:892–900.8. Valji K, Bookstein JJ, Roberts AC, Sanchez RB. Occluded peripheral arteries and bypass grafts: lytic stagnation as an end point for pulse-spray pharmacomechanical thrombolysis. Radiology. 1993. 188:389–394.9. Muller-Hulsbeck S, Jahnke T. Peripheral arterial applications of percutaneous mechanical thrombectomy. Tech Vasc Interv Radiol. 2003. 6:22–34.10. Ansel GM, Botti CF Jr, Silver MJ. Treatment of acute limb ischemia with a percutaneous mechanical thrombectomy-based endovascular approach: 5-year limb salvage and survival results from a single center series. Catheter Cardiovasc Interv. 2008. 72:325–330.11. Ouriel K. Endovascular techniques in the treatment of acute limb ischemia: thrombolytic agents, trials, and percutaneous mechanical thrombectomy techniques. Semin Vasc Surg. 2003. 16:270–279.12. Ricotta JJ, Scudder PA, McAndrew JA, De Weese JA, May AG. Management of acute ischemia of the upper extremity. Am J Surg. 1983. 145:661–666.13. Baguneid M, Dodd D, Fulford P, Hadjilucas Y, Bukhari M, Griffiths G, et al. Management of acute nontraumatic upper limb ischemia. Angiology. 1999. 50:715–720.14. Bergqvist D, Ericsson BF, Konrad P, Bergentz SE. Arterial surgery of the upper extremity. World J Surg. 1983. 7:786–791.15. Hernandez-Richter T, Angele MK, Helmberger T, Jauch KW, Lauterjung L, Schildberg FW. Acute ischemia of the upper extremity: long-term results following thrombembolectomy with the Fogarty catheter. Langenbecks Arch Surg. 2001. 386:261–266.16. Licht PB, Balezantis T, Wolff B, Baudier JF, Roder OC. Long-term outcome following thrombembolectomy in the upper extremity. Eur J Vasc Endovasc Surg. 2004. 28:508–512.17. Lienemann A, Werle K, Weigert F. [Transbrachial arterial catheter angiography. Technique, indications, complications]. Radiologe. 1993. 33:102–107.18. Watkinson AF, Hartnell GG. Complications of direct brachial artery puncture for arteriography: a comparison of techniques. Clin Radiol. 1991. 44:189–191.19. Lederer W, Dingler WH, Gaa J, Brand H, Zoller W, Deininger HK. [The value of the transbrachial approach for arterial visualization using a 4-F catheter]. Rofo. 1989. 151:674–677.20. Chatziioannou A, Ladopoulos C, Mourikis D, Katsenis K, Spanomihos G, Vlachos L. Complications of lower-extremity outpatient arteriography via low brachial artery. Cardiovasc Intervent Radiol. 2004. 27:31–34.21. Ernst S, Fischbach R, Brochhagen HG, Heindel W, Landwehr P. Transbrachial thrombolysis, PTA and stenting in the lower extremities. Cardiovasc Intervent Radiol. 2003. 26:516–521.22. Lupattelli T, Clerissi J, Clerici G, Minnella DP, Casini A, Losa S, et al. The efficacy and safety of closure of brachial access using the AngioSeal closure device: experience with 161 interventions in diabetic patients with critical limb ischemia. J Vasc Surg. 2008. 47:782–788.23. Kiemeneij F, Laarman GJ, Odekerken D, Slagboom T, van der Wieken R. A randomized comparison of percutaneous transluminal coronary angioplasty by the radial, brachial and femoral approaches: the access study. J Am Coll Cardiol. 1997. 29:1269–1275.24. Al-Mubarak N, Vitek JJ, Iyer SS, New G, Roubin GS. Carotid stenting with distal-balloon protection via the transbrachial approach. J Endovasc Ther. 2001. 8:571–575.25. Belenky A, Aranovich D, Greif F, Bachar G, Bartal G, Atar E. Use of a collagen-based device for closure of low brachial artery punctures. Cardiovasc Intervent Radiol. 2007. 30:273–275.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Percutaneous Aspiration Thromboembolectomy(PAT)
- Acute Upper Limb Ischemia Suspected to Have Originated from Staphylococcus Epidermidis Native Valve Endocarditis
- Functional Outcome of Surgical Management for Acute Lower Extremity Ischemia
- Mechanical Thrombectomy for Large Vessel Occlusion via the Transbrachial Approach: Case Series
- Acute ileofemoral artery thromboembolism due to left ventricle thrombi with spontaneous coronary artery dissection