Investig Magn Reson Imaging.
2017 Sep;21(3):154-161. 10.13104/imri.2017.21.3.154.
Diagnostic Performance of Diffusion-Weighted Steady-State Free Precession in Differential Diagnosis of Neoplastic and Benign Osteoporotic Vertebral Compression Fractures: Comparison to Diffusion-Weighted Echo-Planar Imaging
- Affiliations
-
- 1Department of Radiology, Yeouido St. Mary's Hospital, The Catholic University of Korea, Medical College, Seoul, Korea.
- KMID: 2392686
- DOI: http://doi.org/10.13104/imri.2017.21.3.154
Abstract
- PURPOSE
To evaluate the diagnostic performance of diffusion-weighted steady-state free precession (DW-SSFP) in comparison to diffusion-weighted echo-planar imaging (DW-EPI) for differentiating the neoplastic and benign osteoporotic vertebral compression fractures.
MATERIALS AND METHODS
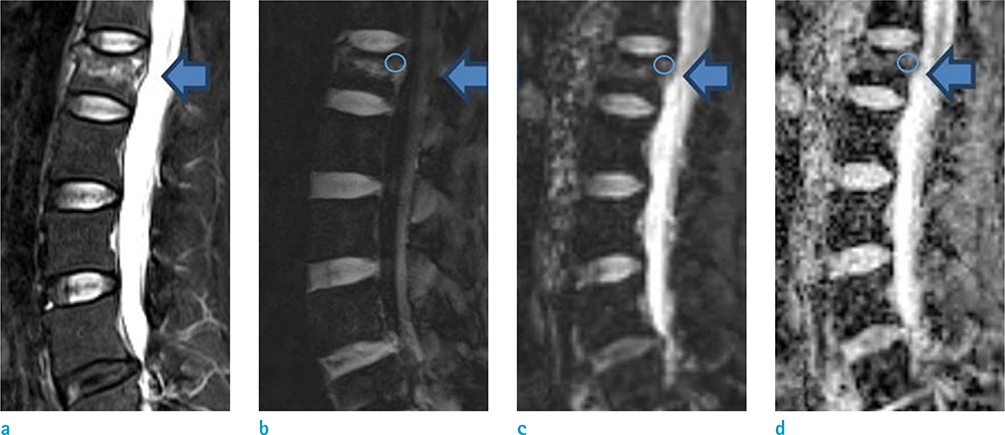
The subjects were 40 patients with recent vertebral compression fractures but no history of vertebroplasty, spine operation, or chemotherapy. They had received 3-Tesla (T) spine magnetic resonance imaging (MRI), including both DW-SSFP and DW-EPI sequences. The 40 patients included 20 with neoplastic vertebral fracture and 20 with benign osteoporotic vertebral fracture. In each fracture lesion, we obtained the signal intensity normalized by the signal intensity of normal bone marrow (SI norm) on DW-SSFP and the apparent diffusion coefficient (ADC) on DW-EPI. The correlation between the SI norm and the ADC in each lesion was analyzed using linear regression. The optimal cut-off values for the diagnosis of neoplastic fracture were determined in each sequence using Youden's J statistics and receiver operating characteristic curve analyses.
RESULTS
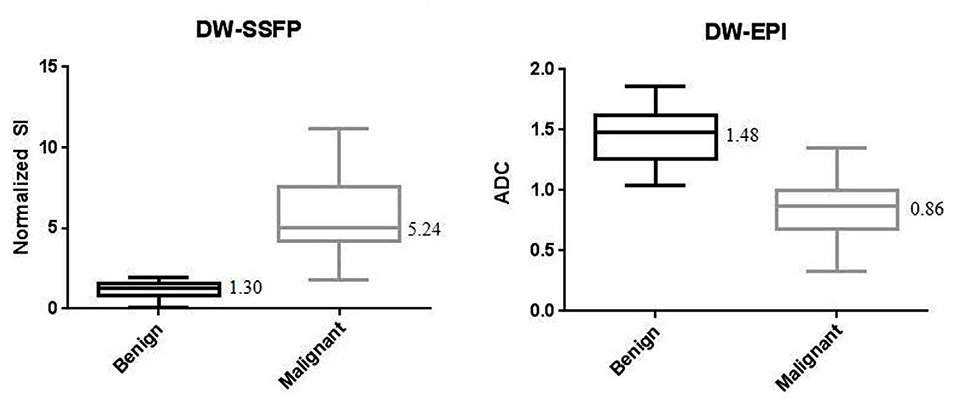
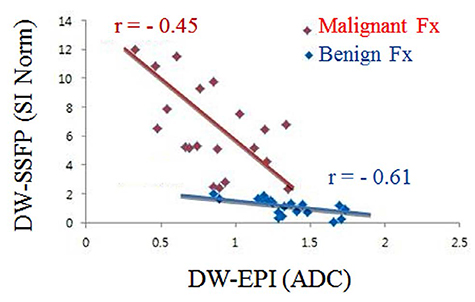
In the neoplastic fracture, the median SI norm on DW-SSFP was higher and the median ADC on DW-EPI was lower than the benign osteoporotic fracture (5.24 vs. 1.30, P = 0.032, and 0.86 vs. 1.48, P = 0.041, respectively). Inverse linear correlations were evident between SI norm and ADC in both neoplastic and benign osteoporotic fractures (r = −0.45 and −0.61, respectively). The optimal cut-off values for diagnosis of neoplastic fracture were SI norm of 3.0 in DW-SSFP with the sensitivity and specificity of 90.4% (95% confidence interval [CI]: 81.0-99.0) and 95.3% (95% CI: 90.0-100.0), respectively, and ADC of 1.3 in DW-EPI with the sensitivity and specificity of 90.5% (95% CI: 80.0-100.0) and 70.4% (95% CI: 60.0-80.0), respectively.
CONCLUSION
In 3-T MRI, DW-SSFP has comparable sensitivity and specificity to DW-EPI in differentiating the neoplastic vertebral fracture from the benign osteoporotic vertebral fracture.
Keyword
MeSH Terms
Figure
Reference
-
1. Kaloostian PE, Yurter A, Zadnik PL, Sciubba DM, Gokaslan ZL. Current paradigms for metastatic spinal disease: an evidence-based review. Ann Surg Oncol. 2014; 21:248–262.2. An HS, Andreshak TG, Nguyen C, Williams A, Daniels D. Can we distinguish between benign versus malignant compression fractures of the spine by magnetic resonance imaging? Spine (Phila Pa 1976). 1995; 20:1776–1782.3. Uetani M, Hashmi R, Hayashi K. Malignant and benign compression fractures: differentiation and diagnostic pitfalls on MRI. Clin Radiol. 2004; 59:124–131.4. Bhugaloo A, Abdullah B, Siow Y, Ng Kh. Diffusion weighted MR imaging in acute vertebral compression fractures: differentiation between malignant and benign causes. Biomed Imaging Interv J. 2006; 2:e12.5. Jung HS, Jee WH, McCauley TR, Ha KY, Choi KH. Discrimination of metastatic from acute osteoporotic compression spinal fractures with MR imaging. Radiographics. 2003; 23:179–187.6. Ho CS, Choi WM, Chen CY, Chen WY, Chan WP. Metastasis in vertebra mimicking acute compression fractures in a patient with osteoporosis: MRI findings. Clin Imaging. 2005; 29:64–67.7. Le Bihan DJ. Differentiation of benign versus pathologic compression fractures with diffusion-weighted MR imaging: a closer step toward the “holy grail” of tissue characterization? Radiology. 1998; 207:305–307.8. Shih TT, Huang KM, Li YW. Solitary vertebral collapse: distinction between benign and malignant causes using MR patterns. J Magn Reson Imaging. 1999; 9:635–642.9. Castillo M, Arbelaez A, Smith JK, Fisher LL. Diffusion-weighted MR imaging offers no advantage over routine noncontrast MR imaging in the detection of vertebral metastases. AJNR Am J Neuroradiol. 2000; 21:948–953.10. Baur A, Huber A, Ertl-Wagner B, et al. Diagnostic value of increased diffusion weighting of a steady-state free precession sequence for differentiating acute benign osteoporotic fractures from pathologic vertebral compression fractures. AJNR Am J Neuroradiol. 2001; 22:366–372.11. International Osteoporosis Foundation web site. The Asian Audit: Epidemiology, costs and burden of osteoporosis in Asia 2009. Accessed March 18, 2017. http://www.iofbonehealth.org/. Published September 2009.12. Park SH, Han PK, Choi SH. Physiological and functional magnetic resonance imaging using balanced steady-state free precession. Korean J Radiol. 2015; 16:550–559.13. Geith T, Schmidt G, Biffar A, et al. Comparison of qualitative and quantitative evaluation of diffusion-weighted MRI and chemical-shift imaging in the differentiation of benign and malignant vertebral body fractures. AJR Am J Roentgenol. 2012; 199:1083–1092.14. Biffar A, Baur-Melnyk A, Schmidt GP, Reiser MF, Dietrich O. Quantitative analysis of the diffusion-weighted steady-state free precession signal in vertebral bone marrow lesions. Invest Radiol. 2011; 46:601–609.15. Chavhan GB, Babyn PS, Jankharia BG, Cheng HL, Shroff MM. Steady-state MR imaging sequences: physics, classification, and clinical applications. Radiographics. 2008; 28:1147–1160.16. Thawait SK, Marcus MA, Morrison WB, Klufas RA, Eng J, Carrino JA. Research synthesis: what is the diagnostic performance of magnetic resonance imaging to discriminate benign from malignant vertebral compression fractures? Systematic review and meta-analysis. Spine (Phila Pa 1976). 2012; 37:E736–E774.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- In Vivo and In Vitro Studies of the Steady State Free Precession-Diffusion-Weighted MR Imagings on Low b-value: Validation and Application to Bone Marrow Pathology
- Diffusion-weighted MR Imaging of Bone Marrow in the Spine: Differentiations of Metastatic Compression Fracture,Benign Compression Fracture, & Spondylitis
- Single-Shot Echo-Planar Diffusion-Weighted MR Imaging at 3T and 1.5T for Differentiation of Benign Vertebral Fracture Edema and Tumor Infiltration
- The Usefulness of Diffusion-weighted MR Imaging for Differentiation between Degenerative Spines and Infectious Spondylitis
- Evaluation of Treatment Response Using Diffusion-Weighted MRI in Metastatic Spines