Obstet Gynecol Sci.
2016 Sep;59(5):407-410. 10.5468/ogs.2016.59.5.407.
Fetal neuroblastoma: ultrasonography and magnetic resonance imaging findings in the prenatal and postnatal IV-S stage
- Affiliations
-
- 1Department of Radiology, ClÃnica de Diagnóstico por Imagem (CDPI), Rio de Janeiro, Brazil.
- 2Department of Obstetrics, Paulista School of Medicine-Federal University of São Paulo (EPM-UNIFESP), São Paulo, Brazil. araujojred@terra.com.br
- KMID: 2391693
- DOI: http://doi.org/10.5468/ogs.2016.59.5.407
Abstract
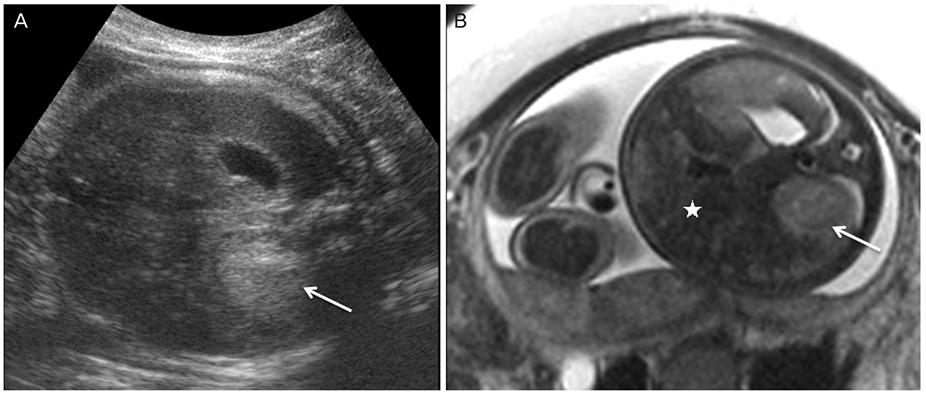
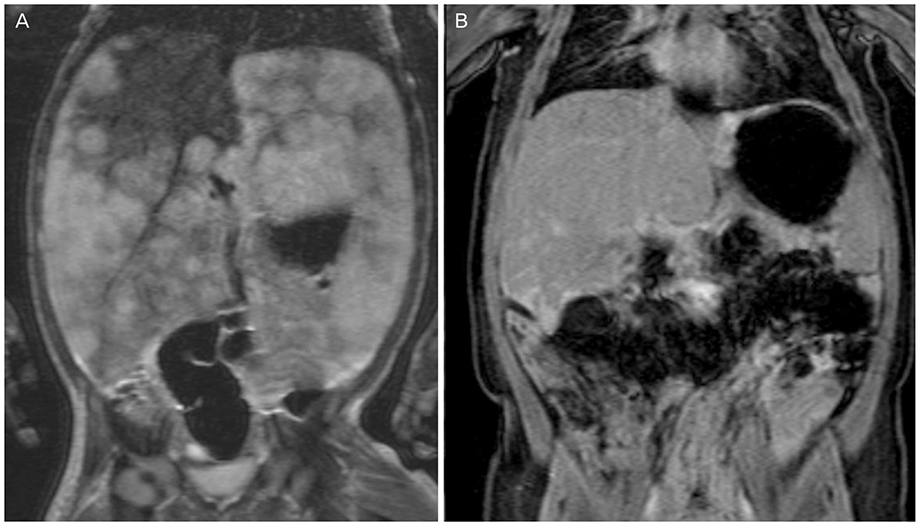
- We report a case of a fetus with an ultrasonography diagnosis of a neuroblastoma during a routine third trimester fetal scan, which presented as a hyperechogenic nodule located above the right kidney. No other abnormalities were found in the ultrasonography scan; however, the follow-up ultrasonography during the 36th week of gestation revealed that the lesion had doubled in size. At the same time, magnetic resonance imaging demonstrated a round mass in the topography of the right adrenal gland with a low signal on T1-weighted images and slightly high signal on T2-weighted images, causing a slight inferior displacement of the kidney. The liver had enlarged and had heterogeneous signal intensity, predominantly hypointense on T2-weighted sequences. Based on these findings, a diagnosis of congenital adrenal neuroblastoma with liver metastases was suggested. A newborn male was delivered by cesarean section 2 weeks later. The physical examination of the neonate revealed abdominal distention and hepatomegaly. The infant had a clinical follow-up in which no surgical or medical intervention was required. At 5 months of age, the infant was asymptomatic with a normal physical examination.
MeSH Terms
Figure
Reference
-
1. Delahaye S, Doz F, Sonigo P, Saada J, Mitanchez D, Sarnacki S, et al. Prenatal diagnosis of dumbbell neuroblastoma. Ultrasound Obstet Gynecol. 2008; 31:92–95.2. DeMarco RT, Casale AJ, Davis MM, Yerkes EB. Congenital neuroblastoma: a cystic retroperitoneal mass in a 34-week fetus. J Urol. 2001; 166:2375.3. Koksal Y, Varan A, Kale G, Tanyel FC, Buyukpamukcu M. Bilateral adrenal cystic neuroblastoma with hepatic and splenic involvement in a newborn. J Pediatr Hematol Oncol. 2005; 27:670–671.4. Chen CP, Chen SH, Chuang CY, Lee HC, Hwu YM, Chang PY, et al. Clinical and perinatal sonographic features of congenital adrenal cystic neuroblastoma: a case report with review of the literature. Ultrasound Obstet Gynecol. 1997; 10:68–73.5. Lee SY, Chuang JH, Huang CB, Hsiao CC, Wan YL, Ng SH, et al. Congenital bilateral cystic neuroblastoma with liver metastases and massive intracystic haemorrhage. Br J Radiol. 1998; 71:1205–1207.6. Luis AL, Martinez L, Hernandez F, Sastre A, Garcia P, Queizan A, et al. Congenital neuroblastomas. Cir Pediatr. 2004; 17:89–92.7. Amler LC, Bauer A, Corvi R, Dihlmann S, Praml C, Cavenee WK, et al. Identification and characterization of novel genes located at the t(1;15)(p36.2;q24) translocation breakpoint in the neuroblastoma cell line NGP. Genomics. 2000; 64:195–202.8. Koesters R, Adams V, Betts D, Moos R, Schmid M, Siermann A, et al. Human eukaryotic initiation factor EIF2C1 gene: cDNA sequence, genomic organization, localization to chromosomal bands 1p34-p35, and expression. Genomics. 1999; 61:210–218.9. Sul HJ, Kang Dy. Congenital neuroblastoma with multiple metastases: a case report. J Korean Med Sci. 2003; 18:618–620.10. Elsayes KM, Mukundan G, Narra VR, Lewis JS Jr, Shirkhoda A, Farooki A, et al. Adrenal masses: mr imaging features with pathologic correlation. Radiographics. 2004; 24:Suppl 1. S73–S86.11. Forman HP, Leonidas JC, Berdon WE, Slovis TL, Wood BP, Samudrala R. Congenital neuroblastoma: evaluation with multimodality imaging. Radiology. 1990; 175:365–368.12. Daltro PA, Werner H. Fetal MRI of the chest. In : Lucaya J, Strife JL, editors. Pediatric chest imaging. Heidelberg: Springer-Verlag;2008. p. 397–416.13. Castel V, Garcia-Miguel P, Canete A, Melero C, Navajas A, Ruiz-Jimenez JI, et al. Prospective evaluation of the International Neuroblastoma Staging System (INSS) and the International Neuroblastoma Response Criteria (INRC) in a multicentre setting. Eur J Cancer. 1999; 35:606–611.14. Lonergan GJ, Schwab CM, Suarez ES, Carlson CL. Neuroblastoma, ganglioneuroblastoma, and ganglioneuroma: radiologic-pathologic correlation. Radiographics. 2002; 22:911–934.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Imaging Diagnosis of Fetal Abdominal Solid Tumor
- Spnontaneous Regrssion of liver metastasis in Stage IV-S neuroblastoma after adrenalectomy: One Case Report
- Comparison of fetal magnetic resonance imaging and ultrasonography for the diagnosis of fetal anomalies
- Prenatal diagnosis of fetal adrenal hemorrhage and endocrinologic evaluation
- A Case of Congenital Neuroblastoma Detected by Prenatal Ultrasonography