Ann Rehabil Med.
2012 Oct;36(5):713-718.
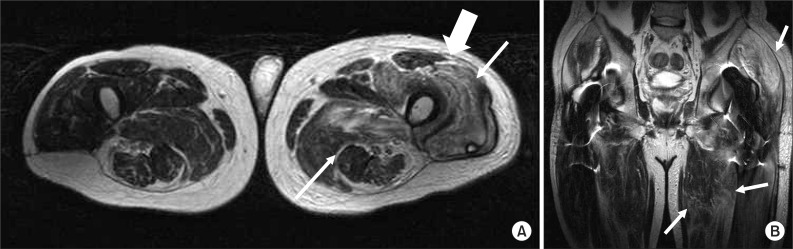
Early Presentation of Heterotopic Ossification Mimicking Pyomyositis: Two Case Reports
- Affiliations
-
- 1Department of Rehabilitation Medicine, Seoul National University College of Medicine, Seoul National University Bundang Hospital, Seongnam 463-707, Korea. drlim1@snu.ac.kr
- 2Department of Rehabilitation Medicine, Armed Forces Capital Hospital, Seongnam 463-040, Korea.
Abstract
- Early diagnosis and treatment of heterotopic ossification (HO) is essential to the prevention of complications. It is difficult to diagnose HO in its initial phase because non-specific clinical manifestations, laboratory findings and imaging findings of immature HO may mimic other diseases such as cellulitis, osteomyelitis, thrombophlebitis, deep vein thrombosis and local infection with abscess. We experienced two cases of HO, which were misdiagnosed as pyomyositis at first by clinical signs and MRI findings indicating the deep infection; the extensive intramuscular ossification appeared later on. We observed an increase of C-reactive protein and creatine kinase followed by the elevation of alkaline phosphatase with abnormal triphasic bone scan. The trajectory of these biomarkers was analyzed to get more insight into the early stages of HO along with the imaging findings. Although our cases cannot be generalized as typical of immature HO, they clearly demonstrate that the change of specific biomarkers with a careful history taking and physical examination should be noted to detect HO as early as possible while avoiding confusion with other mimicking conditions.
Keyword
MeSH Terms
Figure
Reference
-
1. Shehab D, Elgazzar AH, Collier BD. Heterotopic ossification. J Nucl Med. 2002; 43:346–353. PMID: 11884494.2. Shirkhoda A, Armin AR, Bis KG, Makris J, Irwin RB, Shetty AN. MR imaging of myositis ossificans: variable patterns at different stages. J Magn Reson Imaging. 1995; 5:287–292. PMID: 7633105.
Article3. Singh RS, Craig MC, Katholi CR, Jackson AB, Mountz JM. The predictive value of creatine phosphokinase and alkaline phosphatase in identification of heterotopic ossification in patients after spinal cord injury. Arch Phys Med Rehabil. 2003; 84:1584–1588. PMID: 14639555.4. Taly AB, Nair KP, Jayakumar PN, Ravishankar D, Kalaivani PL, Indiradevi B, Murali T. Neurogenic heterotopic ossification: a diagnostic and therapeutic challenge in neurorehabilitation. Neurol India. 2001; 49:37–40. PMID: 11303239.5. McCarthy EF, Sundaram M. Heterotopic ossification: a review. Skeletal Radiol. 2005; 34:609–619. PMID: 16132978.
Article6. Al-Najar M, Obeidat F, Ajlouni J, Mithqal A, Hadidy A. Primary extensive pyomyositis in an immunocompetent patient: case report and literature review. Clin Rheumatol. 2010; 29:1469–1472. PMID: 20857159.
Article7. Sherman AL, Williams J, Patrick L, Banovac K. The value of serum creatine kinase in early diagnosis of heterotopic ossification. J Spinal Cord Med. 2003; 26:227–230. PMID: 14997963.
Article8. Wick L, Berger M, Knecht H, Glucker T, Ledermann HP. Magnetic resonance signal alterations in the acute onset of heterotopic ossification in patients with spinal cord injury. Eur Radiol. 2005; 15:1867–1875. PMID: 15856244.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Osteomyelitis in Heterotopic Ossification after Trochanteric Pressure Sore Reconstruction: A Case Report
- Heterotopic Ossification of a Partially Ruptured Achilles Tendon (A Case Report)
- Heterotopic Ossification Mimics Neurogenic Tumor: A Case Report
- Heterotopic Ossification of the Elbow after Medial Epicondylectomy
- Heterotopic Ossification Combined with Infection in the Hand: A Case Report