Ann Hepatobiliary Pancreat Surg.
2017 Aug;21(3):107-113. 10.14701/ahbps.2017.21.3.107.
Clinicopathological features and post-resection outcomes of biliary cystadenoma and cystadenocarcinoma of the liver
- Affiliations
-
- 1Department of Surgery, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea. shwang@amc.seoul.kr
- KMID: 2389986
- DOI: http://doi.org/10.14701/ahbps.2017.21.3.107
Abstract
- BACKGROUNDS/AIMS
Biliary cystadenoma (BCA) and biliary cystadenocarcinoma (BCAC) account for 5%-10% of liver cystic diseases. In this study, we analysed the clinical presentation and surgical management of patients with BCA and BCAC.
METHODS
We retrospectively analysed the medical records of 23 BCA and 7 BCAC cases diagnosed between January 2007 and December 2013.
RESULTS
There was a statistically significant difference in age (p=0.044) and sex (p=0.048) between BCA and BCAC groups. In the BCA group, 17 patients showed no symptoms (74%), 5 had abdominal pain (22%) and 1 showed abdominal distension (4%). In the BCAC group, two patients were without any symptoms (29%), three had abdominal pain (43%), one showed abdominal distension (14%) and one had fever and chills (14%). The cystic lesion size was widely variable; thus, there was no statistical difference (p=0.84). Complete resection was performed in all patients with BCA and BCAC. No tumour recurrence developed in patients with BCA. In patients with BCAC, 1-, 3- and 5-year disease-free survival rates were 100%, 85.7% and 57.1%, respectively, and 1-, 3- and 5-year overall patient survival rates were 100%, 100% and 75.0%, respectively.
CONCLUSIONS
It is difficult to distinguish between BCA and BCAC via clinical manifestations and diagnostic imaging findings. Surgical resection is the treatment of choice for BCA and BCAC, and patient prognosis after complete resection was very favourable.
MeSH Terms
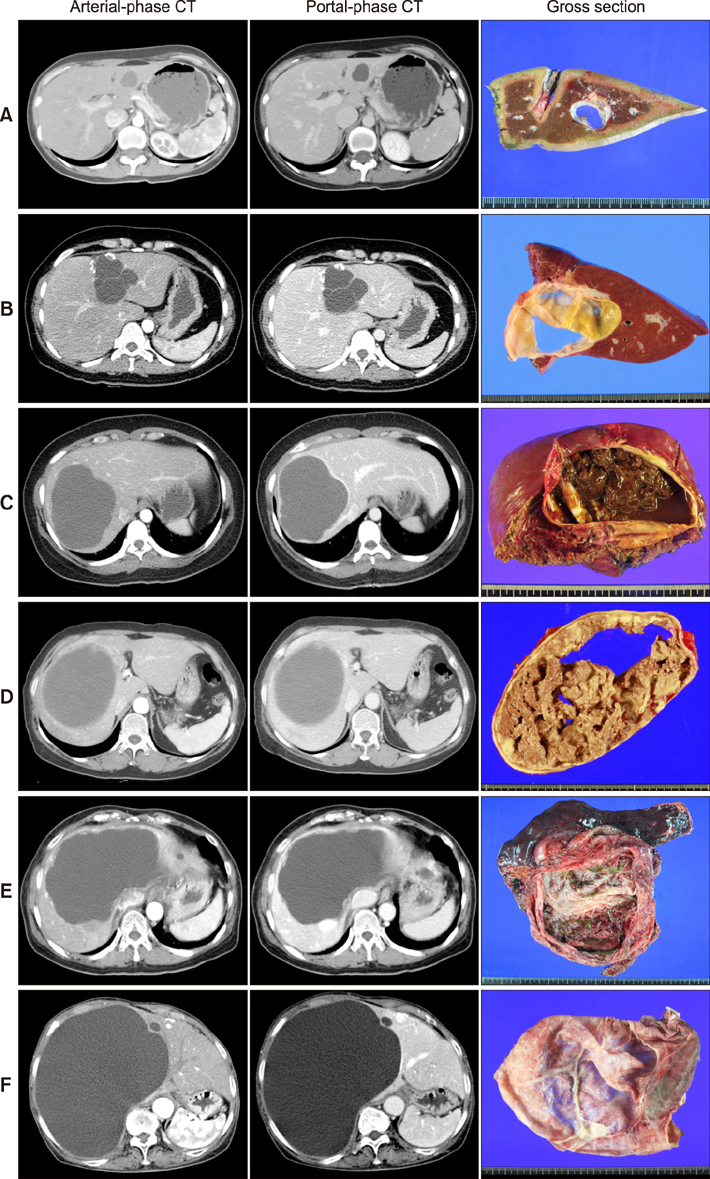
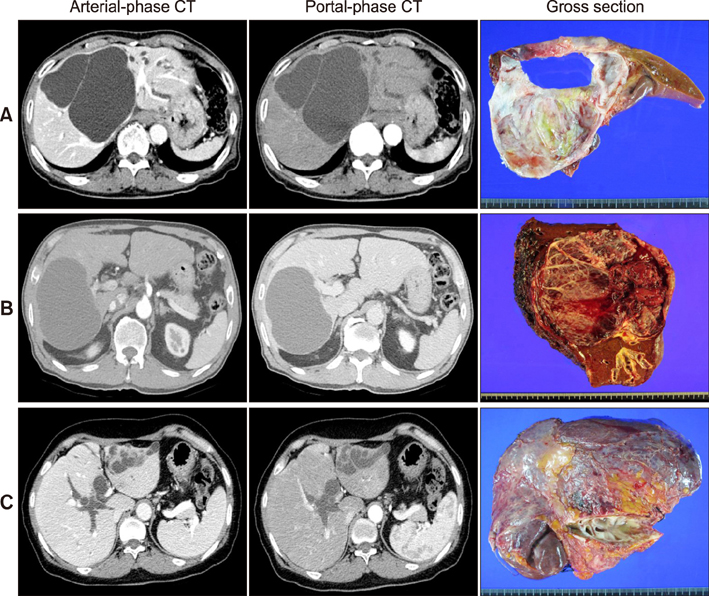
Figure
Cited by 1 articles
-
Pedunculated mucinous cystic neoplasm of the liver: a case report
Sang-Woo Ha, Shin Hwang, Hyejin Han, Song Ie Han, Seung-Mo Hong
J Yeungnam Med Sci. 2021;39(3):250-255. doi: 10.12701/yujm.2021.01256.
Reference
-
1. Yoshida N, Mitsufuji S, Okuda T, Yasukawa S, Sakagami J, Wakabayashi N, et al. Biliary cystadenocarcinoma from biliary cystadenoma. Nihon Shokakibyo Gakkai Zasshi. 2004; 101:1118–1122.2. Vogt DP, Henderson JM, Chmielewski E. Cystadenoma and cystadenocarcinoma of the liver: a single center experience. J Am Coll Surg. 2005; 200:727–733.3. Kubota E, Katsumi K, Iida M, Kishimoto A, Ban Y, Nakata K, et al. Biliary cystadenocarcinoma followed up as benign cystadenoma for 10 years. J Gastroenterol. 2003; 38:278–282.4. Hwang S, Ha TY, Song GW, Jung DH, Ahn CS, Moon DB, et al. Quantified risk assessment for major hepatectomy via the indocyanine green clearance rate and liver volumetry combined with standard liver volume. J Gastrointest Surg. 2015; 19:1305–1314.5. Korean Association for the Study of the Liver. KASL clinical practice guidelines: management of chronic hepatitis B. Clin Mol Hepatol. 2016; 22:18–75.6. Kinoshita H, Tanimura H, Onishi H, Kasano Y, Uchiyama K, Yamaue H. Clinical features and imaging diagnosis of biliary cystadenocarcinoma of the liver. Hepatogastroenterology. 2001; 48:250–252.7. Díaz de Liaño A, Olivera E, Artieda C, Yárnoz C, Ortiz H. Intrahepatic mucinous biliary cystadenoma. Clin Transl Oncol. 2007; 9:678–680.8. Guettier C. Intrahepatic biliary cystic lesions. Ann Pathol. 2010; 30:448–454. (in French).9. Kubota K, Nakanuma Y, Kondo F, Hachiya H, Miyazaki M, Nagino M, et al. Clinicopathological features and prognosis of mucin-producing bile duct tumor and mucinous cystic tumor of the liver: a multi-institutional study by the Japan Biliary Association. J Hepatobiliary Pancreat Sci. 2014; 21:176–185.10. Kim HH, Hur YH, Koh YS, Cho CK, Kim JW. Intrahepatic biliary cystadenoma: Is there really an almost exclusively female predominance? World J Gastroenterol. 2011; 17:3073–3074.11. Soares KC, Arnaoutakis DJ, Kamel I, Anders R, Adams RB, Bauer TW, et al. Cystic neoplasms of the liver: biliary cystadenoma and cystadenocarcinoma. J Am Coll Surg. 2014; 218:119–128.12. Lewin M, Mourra N, Honigman I, Fléjou JF, Parc R, Arrivé L, et al. Assessment of MRI and MRCP in diagnosis of biliary cystadenoma and cystadenocarcinoma. Eur Radiol. 2006; 16:407–413.13. Precetti S, Gandon Y, Vilgrain V. Imaging of cystic liver diseases. J Radiol. 2007; 88:1061–1072. (in French).14. Tanaka T, Gobara H, Tomita K, Hiraki T, Tanaka T, Kanazawa S. Hepatic intracystic organizing hematoma mimicking biliary cystadenocarcinoma in a patient with polycystic liver disease. Intern Med. 2015; 54:2001–2005.15. Wang C, Miao R, Liu H, Du X, Liu L, Lu X, et al. Intrahepatic biliary cystadenoma and cystadenocarcinoma: an experience of 30 cases. Dig Liver Dis. 2012; 44:426–431.16. Zhang FB, Zhang AM, Zhang ZB, Huang X, Wang XT, Dong JH. Preoperative differential diagnosis between intrahepatic biliary cystadenoma and cystadenocarcinoma: a single-center experience. World J Gastroenterol. 2014; 20:12595–12601.17. Horsmans Y, Laka A, Gigot JF, Geubel AP. Serum and cystic fluid CA 19-9 determinations as a diagnostic help in liver cysts of uncertain nature. Liver. 1996; 16:255–257.18. Chen YW, Li CH, Liu Z, Dong JH, Zhang WZ, Jiang K. Surgical management of biliary cystadenoma and cystadenocarcinoma of the liver. Genet Mol Res. 2014; 13:6383–6390.19. Pitchaimuthu M, Aidoo-Micah G, Coldham C, Sutcliffe R, Roberts JK, Muiesan P, et al. Outcome following resection of biliary cystadenoma: a single centre experience and literature review. Int J Hepatol. 2015; 2015:382315.20. Fragulidis GP, Vezakis AI, Konstantinidis CG, Chondrogiannis KK, Primetis ES, Kondi-Pafiti A, et al. Diagnostic and therapeutic challenges of intrahepatic biliary cystadenoma and cystadenocarcinoma: a report of 10 cases and review of the literature. Int Surg. 2015; 100:1212–1219.21. Banerjee A, Shah SR, Singh A, Joshi A, Desai D. Rare biliary cystic tumors: a case series of biliary cystadenomas and cystadenocarcinoma. Ann Hepatol. 2016; 15:448–452.