J Breast Cancer.
2017 Jun;20(2):212-216. 10.4048/jbc.2017.20.2.212.
A Case of Breast Cancer Brain Metastasis with a 16-Year Time Interval without Evidence of Cancer Recurrence
- Affiliations
-
- 1Department of Neurosurgery, Teikyo University Mizonokuchi Hospital, Kawasaki, Japan. merrityamada@hotmail.co.jp
- 2Department of Neurology, Teikyo University Mizonokuchi Hospital, Kawasaki, Japan.
- KMID: 2389761
- DOI: http://doi.org/10.4048/jbc.2017.20.2.212
Abstract
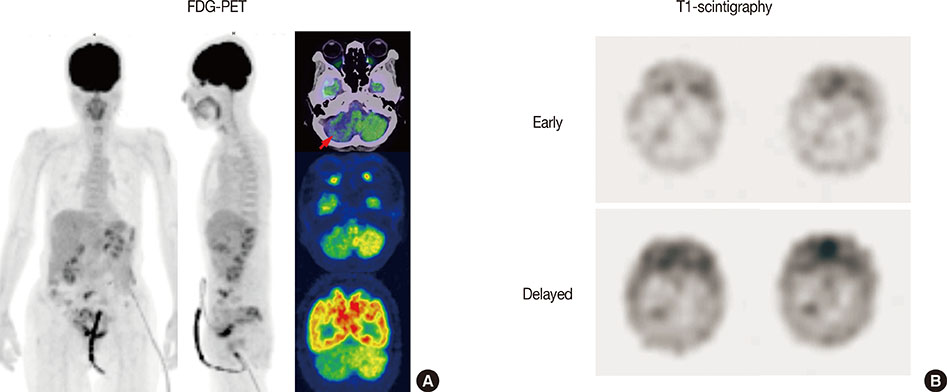
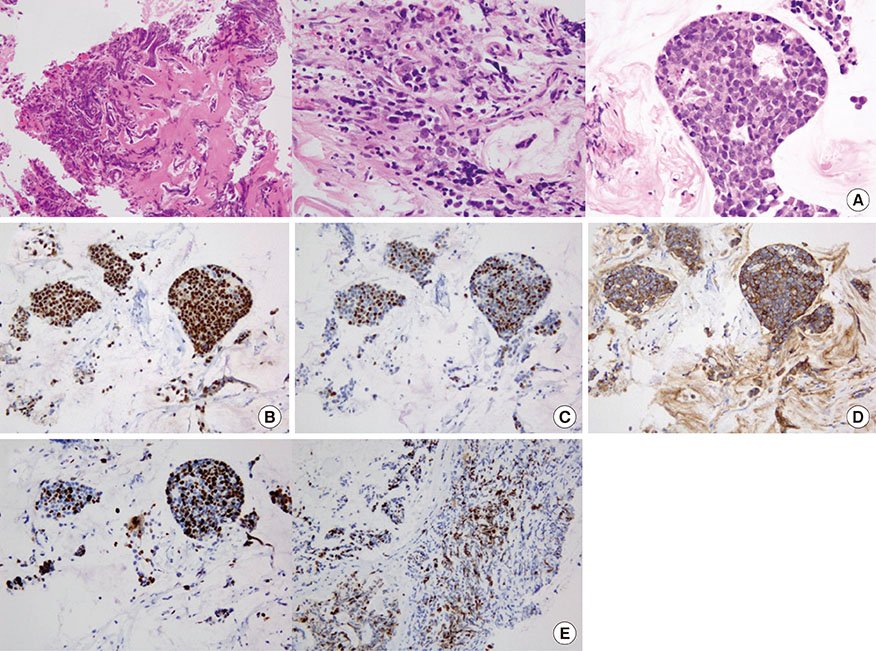
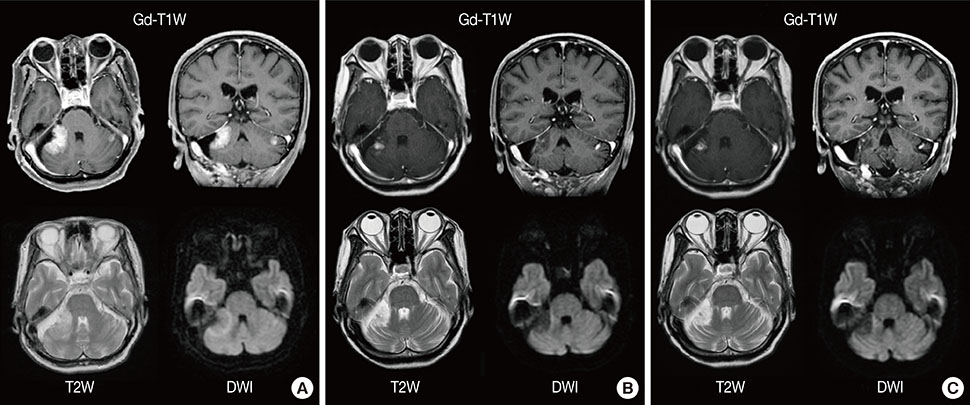
- The median time of brain metastasis from the diagnosis of breast cancer is approximately 3 years. In this case report, a 69-year-old woman demonstrated cerebellar ataxia. Brain magnetic resonance imaging revealed enhanced lesions in bilateral cerebellar hemispheres. She had undergone surgery, radiation, and chemotherapy for uterine and breast cancer 24 years prior and 16 years prior, respectively. Although she had not received any anticancer treatment for 10 years, no recurrences were identified using whole body scans. A partial tumor resection was performed and the histological diagnosis was an adenocarcinoma from breast cancer. As no extracranial lesions were found, gamma-knife irradiation was performed, without additional systemic chemotherapy. One month posttreatment, the tumors dramatically reduced in size and the patient completely recovered from cerebellar ataxia. Systemic chemotherapy is not always required for brain metastasis from breast cancer with a long interval period, as long as no evidence of extracranial recurrence is detected.
Keyword
MeSH Terms
Figure
Reference
-
1. De Ieso PB, Schick U, Rosenfelder N, Mohammed K, Ross GM. Breast cancer brain metastases: a 12 year review of treatment outcomes. Breast. 2015; 24:426–433.2. Rostami R, Mittal S, Rostami P, Tavassoli F, Jabbari B. Brain metastasis in breast cancer: a comprehensive literature review. J Neurooncol. 2016; 127:407–414.
Article3. Brogi E, Murphy CG, Johnson ML, Conlin AK, Hsu M, Patil S, et al. Breast carcinoma with brain metastases: clinical analysis and immunoprofile on tissue microarrays. Ann Oncol. 2011; 22:2597–2603.
Article4. Patanaphan V, Salazar OM, Risco R. Breast cancer: metastatic patterns and their prognosis. South Med J. 1988; 81:1109–1112.5. Park HS, Kim S, Kim K, Yoo H, Chae BJ, Bae JS, et al. Pattern of distant recurrence according to the molecular subtypes in Korean women with breast cancer. World J Surg Oncol. 2012; 10:4.
Article6. Pestalozzi BC, Zahrieh D, Price KN, Holmberg SB, Lindtner J, Collins J, et al. Identifying breast cancer patients at risk for central nervous system (CNS) metastases in trials of the International Breast Cancer Study Group (IBCSG). Ann Oncol. 2006; 17:935–944.
Article7. Swain SM, Baselga J, Kim SB, Ro J, Semiglazov V, Campone M, et al. Pertuzumab, trastuzumab, and docetaxel in HER2-positive metastatic breast cancer. N Engl J Med. 2015; 372:724–734.
Article8. Pors H, von Eyben FE, Sørensen OS, Larsen M. Longterm remission of multiple brain metastases with tamoxifen. J Neurooncol. 1991; 10:173–177.
Article9. Crivellari D, Pagani O, Veronesi A, Lombardi D, Nolè F, Thürlimann B, et al. High incidence of central nervous system involvement in patients with metastatic or locally advanced breast cancer treated with epirubicin and docetaxel. Ann Oncol. 2001; 12:353–356.
Article10. Larsen PB, Kümler I, Nielsen DL. A systematic review of trastuzumab and lapatinib in the treatment of women with brain metastases from HER2-positive breast cancer. Cancer Treat Rev. 2013; 39:720–727.
Article11. Nieder C, Oehlke O, Hintz M, Grosu AL. The challenge of durable brain control in patients with brain-only metastases from breast cancer. Springerplus. 2015; 4:585.
Article12. Madhup R, Kirti S, Bhatt ML, Srivastava PK, Srivastava M, Kumar S. Letrozole for brain and scalp metastases from breast cancer: a case report. Breast. 2006; 15:440–442.13. Ogawa K, Yoshii Y, Nishimaki T, Tamaki N, Miyaguni T, Tsuchida Y, et al. Treatment and prognosis of brain metastases from breast cancer. J Neurooncol. 2008; 86:231–238.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Pancreatic Metastasis from Invasive Ductal Carcinoma of the Breast
- The Impact of Local and Regional Recurrence on Distant Metastasis and Survival in Patients Treated with Breast Conservation Therapy
- Colon Obstruction due to Colonic Metastasis of a Breast Carcinoma
- Breast Cancer to Meningioma: A Rare Case of Tumor-to-Tumor Metastasis
- Rapid Progression of Duodenal Metastasis from Invasive Lobular Breast Carcinoma