J Breast Cancer.
2017 Jun;20(2):160-169. 10.4048/jbc.2017.20.2.160.
Prognostic Impact of Progesterone Receptor Status in Chinese Estrogen Receptor Positive Invasive Breast Cancer Patients
- Affiliations
-
- 1Department of General Surgery, Aerospace Central Hospital, Beijing, China.
- 2Breast Diseases Treatment Center, Fourth Hospital of Hebei Medical University, Shijiazhuang, China. songzhch@hotmail.com
- KMID: 2389753
- DOI: http://doi.org/10.4048/jbc.2017.20.2.160
Abstract
- PURPOSE
Estrogen receptor (ER) and progesterone receptor (PR) have been used as indicators of endocrine system status since the mid-1970s in the clinical management of breast cancer. The predictive role of ER in endocrine therapy is undisputed, but the prognostic value of PR is still debated. The aim of this study was to investigate the clinical characteristics and prognosis of ER positive breast cancer with different PR expression levels.
METHODS
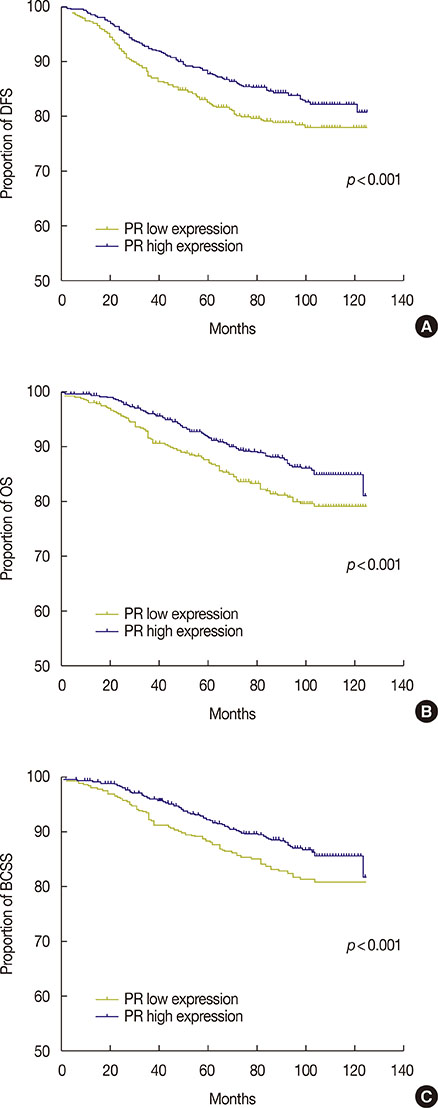
A population cohort of 3,030 primary invasive ER positive breast cancer patients from a single cancer center underwent surgery and received adjuvant endocrine therapy from 2004 to 2010. The clinical and biological features of these patients with high PR-expressing tumors were compared with those of patients with low PR-expressing tumors. The follow-up data for disease-free survival (DFS), overall survival (OS), and breast cancer specific survival (BCSS) was obtained from 2,778 patients. Cox regression analysis was used to correlate biomarkers and tumor characteristics with DFS, OS, and BCSS.
RESULTS
Tumors with low PR expression had more invasive pathological features and biological indexes than those with high PR expression. Low PR expression was an independent poor prognostic factor for DFS (p=0.014; hazard ratio [HR], 0.781; 95% confidence interval [CI], 0.641-0.950), OS (p=0.002; HR, 0.699; 95% CI, 0.560-0.873), and BCSS (p=0.005; HR, 0.714; 95% CI, 0.566-0.902). Furthermore, in low PR expressing tumors, patients who received chemotherapy had better DFS (p=0.002; HR, 0.449; 95% CI, 0.268-0.751), OS (p<0.001; HR, 0.341; 95% CI, 0.192-0.606), and BCSS (p<0.001; HR, 0.292; 95% CI, 0.156-0.549) than patients who did not received chemotherapy.
CONCLUSION
Patients with ER positive invasive breast cancer with low PR expressing tumors have a worse prognosis than those with high PR expressing tumors, and these patients can benefit from chemotherapy.
Keyword
MeSH Terms
Figure
Reference
-
1. Palmieri C, Patten DK, Januszewski A, Zucchini G, Howell SJ. Breast cancer: current and future endocrine therapies. Mol Cell Endocrinol. 2014; 382:695–723.
Article2. Bae SY, Kim S, Lee JH, Lee HC, Lee SK, Kil WH, et al. Poor prognosis of single hormone receptor-positive breast cancer: similar outcome as triple-negative breast cancer. BMC Cancer. 2015; 15:138.3. Viale G, Regan MM, Maiorano E, Mastropasqua MG, Dell'Orto P, Rasmussen BB, et al. Prognostic and predictive value of centrally reviewed expression of estrogen and progesterone receptors in a randomized trial comparing letrozole and tamoxifen adjuvant therapy for postmenopausal early breast cancer: BIG 1-98. J Clin Oncol. 2007; 25:3846–3852.
Article4. Arpino G, Weiss H, Lee AV, Schiff R, De Placido S, Osborne CK, et al. Estrogen receptor-positive, progesterone receptor-negative breast cancer: association with growth factor receptor expression and tamoxifen resistance. J Natl Cancer Inst. 2005; 97:1254–1261.
Article5. Elledge RM, Green S, Pugh R, Allred DC, Clark GM, Hill J, et al. Estrogen receptor (ER) and progesterone receptor (PgR), by ligand-binding assay compared with ER, PgR and pS2, by immuno-histochemistry in predicting response to tamoxifen in metastatic breast cancer: a Southwest Oncology Group Study. Int J Cancer. 2000; 89:111–117.
Article6. Dowsett M, Cuzick J, Wale C, Howell T, Houghton J, Baum M. Retrospective analysis of time to recurrence in the ATAC trial according to hormone receptor status: an hypothesis-generating study. J Clin Oncol. 2005; 23:7512–7517.
Article7. Hammond ME, Hayes DF, Wolff AC, Mangu PB, Temin S. American Society of Clinical Oncology/College of American Pathologists guideline recommendations for immunohistochemical testing of estrogen and progesterone receptors in breast cancer. J Oncol Pract. 2010; 6:195–197.
Article8. Goldhirsch A, Winer EP, Coates AS, Gelber RD, Piccart-Gebhart M, Thürlimann B, et al. Personalizing the treatment of women with early breast cancer: highlights of the St Gallen international expert consensus on the primary therapy of early breast cancer 2013. Ann Oncol. 2013; 24:2206–2223.
Article9. Wolff AC, Hammond ME, Hicks DG, Dowsett M, McShane LM, Allison KH, et al. Recommendations for human epidermal growth factor receptor 2 testing in breast cancer: American Society of Clinical Oncology/College of American Pathologists clinical practice guideline update. J Clin Oncol. 2013; 31:3997–4013.
Article10. Chao WR, Lee MY, Lin WL, Chen CK, Lin JC, Koo CL, et al. HER2 amplification and overexpression are significantly correlated in mucinous epithelial ovarian cancer. Hum Pathol. 2014; 45:810–816.
Article11. Parkin DM, Bray F, Ferlay J, Pisani P. Global cancer statistics, 2002. CA Cancer J Clin. 2005; 55:74–108.
Article12. de Bono JS, Tolcher AW, Rowinsky EK. The future of cytotoxic therapy: selective cytotoxicity based on biology is the key. Breast Cancer Res. 2003; 5:154–159.
Article13. Carey LA, Perou CM, Livasy CA, Dressler LG, Cowan D, Conway K, et al. Race, breast cancer subtypes, and survival in the Carolina Breast Cancer Study. JAMA. 2006; 295:2492–2502.
Article14. Li FY, Wu SG, Zhou J, Sun JY, Lin Q, Lin HX, et al. Prognostic value of Ki-67 in breast cancer patients with positive axillary lymph nodes: a retrospective cohort study. PLoS One. 2014; 9:e87264.
Article15. Kabos P, Finlay-Schultz J, Li C, Kline E, Finlayson C, Wisell J, et al. Patient-derived luminal breast cancer xenografts retain hormone receptor heterogeneity and help define unique estrogen-dependent gene signatures. Breast Cancer Res Treat. 2012; 135:415–432.
Article16. Zheng ZY, Bay BH, Aw SE, Lin VC. A novel antiestrogenic mechanism in progesterone receptor-transfected breast cancer cells. J Biol Chem. 2005; 280:17480–17487.
Article17. Mohammed H, Russell IA, Stark R, Rueda OM, Hickey TE, Tarulli GA, et al. Progesterone receptor modulates ERalpha action in breast cancer. Nature. 2015; 523:313–317.
Article18. Rakha EA, El-Sayed ME, Green AR, Paish EC, Powe DG, Gee J, et al. Biologic and clinical characteristics of breast cancer with single hormone receptor positive phenotype. J Clin Oncol. 2007; 25:4772–4778.
Article19. Liu S, Chia SK, Mehl E, Leung S, Rajput A, Cheang MC, et al. Progesterone receptor is a significant factor associated with clinical outcomes and effect of adjuvant tamoxifen therapy in breast cancer patients. Breast Cancer Res Treat. 2010; 119:53–61.
Article20. Huang HJ, Neven P, Drijkoningen M, Paridaens R, Wildiers H, Van Limbergen E, et al. Association between tumour characteristics and HER-2/neu by immunohistochemistry in 1362 women with primary operable breast cancer. J Clin Pathol. 2005; 58:611–616.
Article21. Early Breast Cancer Trialists' Collaborative Group (EBCTCG). Davies C, Godwin J, Gray R, Clarke M, Cutter D, et al. Relevance of breast cancer hormone receptors and other factors to the efficacy of adjuvant tamoxifen: patient-level meta-analysis of randomised trials. Lancet. 2011; 378:771–784.
Article22. Xue C, Wang X, Peng R, Shi Y, Qin T, Liu D, et al. Distribution, clinicopathologic features and survival of breast cancer subtypes in Southern China. Cancer Sci. 2012; 103:1679–1687.
Article23. Rosa Mendoza ES, Moreno E, Caguioa PB. Predictors of early distant metastasis in women with breast cancer. J Cancer Res Clin Oncol. 2013; 139:645–652.
Article24. Xing P, Li JG, Jin F, Zhao TT, Liu Q, Dong HT, et al. Prognostic significance of body mass index in breast cancer patients with hormone receptor-positive tumours after curative surgery. Clin Invest Med. 2013; 36:E297–E305.
Article25. Dirier A, Burhanedtin-Zincircioglu S, Karadayi B, Isikdogan A, Aksu R. Characteristics and prognosis of breast cancer in younger women. J BUON. 2009; 14:619–623.26. Kakugawa Y, Minami Y, Tateno H, Inoue H, Fujiya T. Relation of serum levels of estrogen and dehydroepiandrosterone sulfate to hormone receptor status among postmenopausal women with breast cancer. Breast Cancer. 2007; 14:269–276.
Article27. Arafah BM, Finegan HM, Roe J, Manni A, Pearson OH. Hormone dependency in N-nitrosomethylurea-induced rat mammary tumors. Endocrinology. 1982; 111:584–588.
Article28. Chen XS, Wu JY, Huang O, Chen CM, Wu J, Lu JS, et al. Molecular subtype can predict the response and outcome of Chinese locally advanced breast cancer patients treated with preoperative therapy. Oncol Rep. 2010; 23:1213–1220.
Article29. Yao L, Zhang J, Liu Y, Ouyang T, Li J, Wang T, et al. Association between HER2 status and response to neoadjuvant anthracycline followed by paclitaxel plus carboplatin chemotherapy without trastuzumab in breast cancer. Chin J Cancer Res. 2015; 27:553–561.30. Kim HJ, Cui X, Hilsenbeck SG, Lee AV. Progesterone receptor loss correlates with human epidermal growth factor receptor 2 overexpression in estrogen receptor-positive breast cancer. Clin Cancer Res. 2006; 12(3 Pt 2):1013s–1018s.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Treatment Outcomes of Weakly Positive Hormone Receptor Breast Cancer and Triple-Negative Breast Cancer
- Expression of the pS2 Protein and Its Relation with Estrogen and Progesterone Receptor in Breast Cancer
- Relation Between Hormone Receptor (Enzyme-Immunoassay and Immunohistochemistry), Histologic Grade and Mammographic Findings in Patients with Primary Breast Cancer
- Correlation of Mammographic Findings and Hormonal Receptor in Patients with Breast Cancer
- Clinical Significance of DAX-1 Expression using Immunihistochemical Staining in Breast Cancer