Ann Dermatol.
2017 Oct;29(5):578-585. 10.5021/ad.2017.29.5.578.
A Study of the Changes of T Helper 17 Cells and Regulatory T Cells in Herpes Zoster
- Affiliations
-
- 1Department of Dermatology, Chosun University School of Medicine, Gwangju, Korea. derm75@chosun.ac.kr
- KMID: 2388909
- DOI: http://doi.org/10.5021/ad.2017.29.5.578
Abstract
- BACKGROUND
Immunosuppression and age-related deficiencies in cell-mediated immunity are important factors for the reactivation of latent varicella-zoster virus (VZV). CD4âºCD25âºFoxp3⺠regulatory T (Treg) cells and T helper 17 (Th17) cells are closely associated with various viral infections.
OBJECTIVE
We analyzed Treg cells and Th17 cells in patients with herpes zoster and investigated their relationship with the reactivation of latent VZV.
METHODS
Treg and Th17 cells in peripheral blood and the ratio of Th17 to Treg cells were examined in patients with herpes zoster and healthy controls. Changes between pre-treatment and post-treatment estimates of Treg and Th17 cells and clinical parameters in patients with herpes zoster were also analyzed.
RESULTS
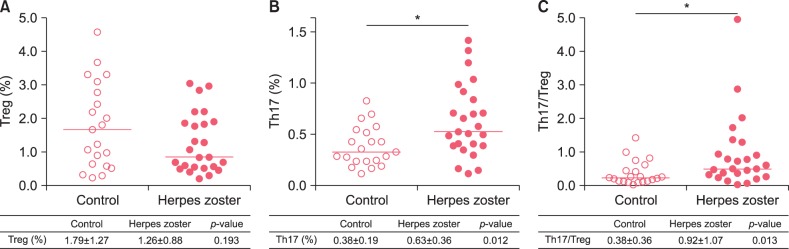
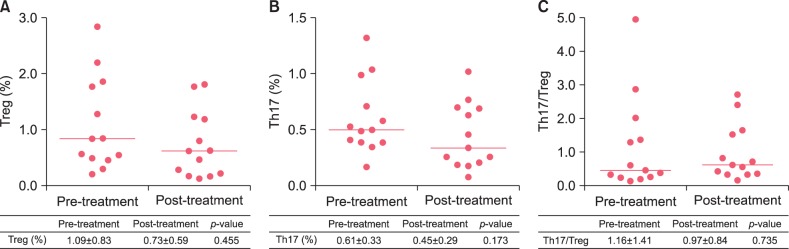
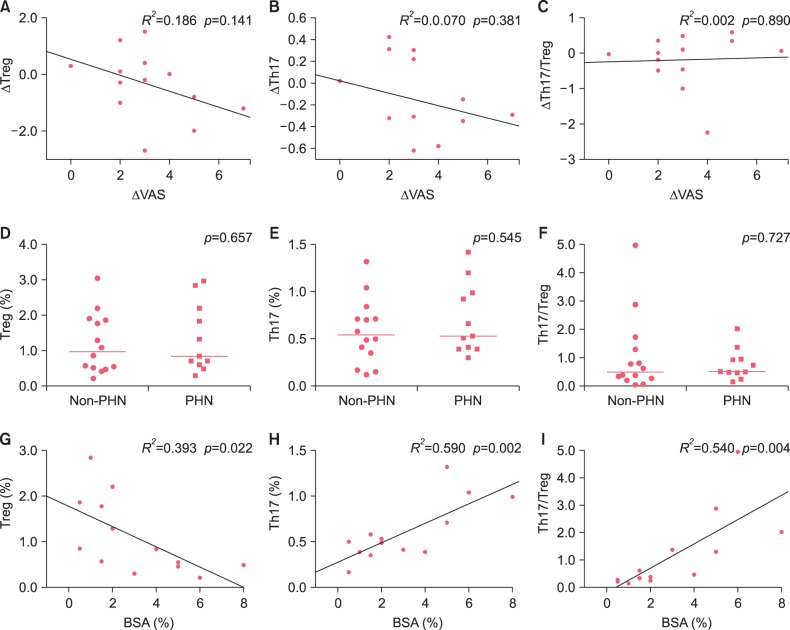
The proportion of circulating Th17 cells and the Th17/Treg cell ratio were significantly higher in patients with herpes zoster than controls (p=0.012, 0.013), but there was no significant difference in the proportion of Treg cells between groups. There was no significant difference in the proportions of Treg and Th17 cells and the Th17/Treg cell ratio before and after treatment and between the non-postherpetic neuralgia and postherpetic neuralgia groups. Changes in Treg and Th17 cells and the Th17/Treg cell ratio were not significantly correlated with changes in the visual analog scale. Body surface area was significantly correlated with Treg cells, Th17 cells, and the Th17/Treg cell ratio (p=0.022, 0.002, 0.004).
CONCLUSION
An imbalance between Th17 and Treg cells is associated with the reactivation of VZV, which may contribute to pathogenesis of herpes zoster.
MeSH Terms
Figure
Reference
-
1. Schmader KE, Oxman MN. Varicella and herpes zoster. In : Goldsmith LA, Katz SI, Gilchrest BA, Paller AS, Leffell DJ, Wolff K, editors. Fitzpatrick's dermatology in general medicine. 8th ed. New York: McGraw-Hill;2012. p. 2386.2. Vukmanovic-Stejic M, Sandhu D, Seidel JA, Patel N, Sobande TO, Agius E, et al. The characterization of varicella zoster virus-specific T cells in skin and blood during aging. J Invest Dermatol. 2015; 135:1752–1762. PMID: 25734814.
Article3. Xing Q, Hu D, Shi F, Chen F. Role of regulatory T cells in patients with acute herpes zoster and relationship to postherpetic neuralgia. Arch Dermatol Res. 2013; 305:715–722. PMID: 23689682.
Article4. Steain M, Sutherland JP, Rodriguez M, Cunningham AL, Slobedman B, Abendroth A. Analysis of T cell responses during active varicella-zoster virus reactivation in human ganglia. J Virol. 2014; 88:2704–2716. PMID: 24352459.
Article5. Martinez NE, Sato F, Kawai E, Omura S, Chervenak RP, Tsunoda I. Regulatory T cells and Th17 cells in viral infections: implications for multiple sclerosis and myocarditis. Future Virol. 2012; 7:593–608. PMID: 23024699.
Article6. Xue-Song L, Cheng-Zhong L, Ying Z, Mo-Bin W. Changes of Treg and Th17 cells balance in the development of acute and chronic hepatitis B virus infection. BMC Gastroenterol. 2012; 12:43. PMID: 22548790.
Article7. Hao C, Zhou Y, He Y, Fan C, Sun L, Wei X, et al. Imbalance of regulatory T cells and T helper type 17 cells in patients with chronic hepatitis C. Immunology. 2014; 143:531–538. PMID: 24903732.
Article8. Falaki F, Nejat AH, Dalirsani Z. The effect of low-level laser therapy on trigeminal neuralgia: a review of literature. J Dent Res Dent Clin Dent Prospects. 2014; 8:1–5. PMID: 25024832.9. Arvin A, Abendroth A. VZV: immunobiology and host response. In : Arvin A, Campadelli-Fiume G, Mocarski E, Moore PS, Roizman B, Whitley R, editors. Human herpesviruses: biology, therapy, and immunoprophylaxis. Cambridge: Cambridge University Press;2007. p. 700–712.10. Roh NK, Park YM, Kang H, Choi GS, Kim BJ, Lee YW, et al. Awareness, knowledge, and vaccine acceptability of herpes zoster in Korea: a multicenter survey of 607 patients. Ann Dermatol. 2015; 27:531–538. PMID: 26512167.11. Chen Y, Fang J, Chen X, Pan C, Liu X, Liu J. Effects of the Treg/Th17 cell balance and their associated cytokines in patients with hepatitis B infection. Exp Ther Med. 2015; 9:573–578. PMID: 25574237.
Article12. Li S, Gowans EJ, Chougnet C, Plebanski M, Dittmer U. Natural regulatory T cells and persistent viral infection. J Virol. 2008; 82:21–30. PMID: 17855537.
Article13. Rushbrook SM, Ward SM, Unitt E, Vowler SL, Lucas M, Klenerman P, et al. Regulatory T cells suppress in vitro proliferation of virus-specific CD8+ T cells during persistent hepatitis C virus infection. J Virol. 2005; 79:7852–7859. PMID: 15919939.14. Vukmanovic-Stejic M, Sandhu D, Sobande TO, Agius E, Lacy KE, Riddell N, et al. Varicella zoster-specific CD4+Foxp3+ T cells accumulate after cutaneous antigen challenge in humans. J Immunol. 2013; 190:977–986. PMID: 23284056.
Article15. Hou W, Kang HS, Kim BS. Th17 cells enhance viral persistence and inhibit T cell cytotoxicity in a model of chronic virus infection. J Exp Med. 2009; 206:313–328. PMID: 19204109.
Article16. Zajkowska A, Garkowski A, Świerzbińska R, KułZakowska A, Król ME, Ptaszyńska-Sarosiek I, et al. Evaluation of chosen cytokine levels among patients with herpes zoster as ability to provide immune response. PLoS One. 2016; 11:e0150301. PMID: 26934574.
Article17. Weinberg A, Huang S, Song LY, Fenton T, Williams P, Patterson J, et al. Immune correlates of herpes zoster in HIV-infected children and youth. J Virol. 2012; 86:2878–2881. PMID: 22171274.
Article18. Xu L, Kitani A, Fuss I, Strober W. Cutting edge: regulatory T cells induce CD4+CD25-Foxp3- T cells or are self-induced to become Th17 cells in the absence of exogenous TGF-beta. J Immunol. 2007; 178:6725–6729. PMID: 17513718.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Study of Cellular and Humoral Immunity in Patients with Herpes Zoster
- Herpes Zoster in the Patients with Malignant Tumor
- Herpes Zoster Duplex Symmetricus in a Healthy Patient
- A Case of Herpes Zoster Duplex Unilateralis with Herpes Zoster Generalisatus
- Herpes Zoster Treated with Vidarabine-5-Monophosphate