Anesth Pain Med.
2017 Jul;12(3):261-265. 10.17085/apm.2017.12.3.261.
Optimal dose of dexmedetomidine for sedation during epidural anesthesia
- Affiliations
-
- 1Department of Anesthesia and Pain Medicine, Pusan National University Yangsan Hospital, Yangsan, Korea. md.baeksh@gmail.com
- KMID: 2388844
- DOI: http://doi.org/10.17085/apm.2017.12.3.261
Abstract
- BACKGROUND
Sedation during epidural anesthesia can reduce patients' anxiety and discomfort. Dexmedetomidine has sedative, hypnotic, and analgesic effects, with minimal respiratory depression. However, the use of dexmedetomidine is associated with prolonged recovery. This study investigated the optimal dose of intravenous dexmedetomidine for proper sedation with minimal recovery time in epidural anesthesia.
METHODS
Sixty-three patients (American Society of Anesthesiologists physical status I/II) were randomized into two groups. Following epidural anesthesia, a loading dose (1 µg/kg) of dexmedetomidine was administered for 10 min followed by maintenance infusion as follows: Group A (n = 32; dexmedetomidine 0.6 µg/kg/h) and Group B (n = 31; dexmedetomidine 1.0 µg/kg/h). Heart rate, blood pressure, and bispectral index score (BIS) were recorded during surgery. The length of stay and modified Aldrete score (MAS) were measured in the postanesthesia care unit (PACU).
RESULTS
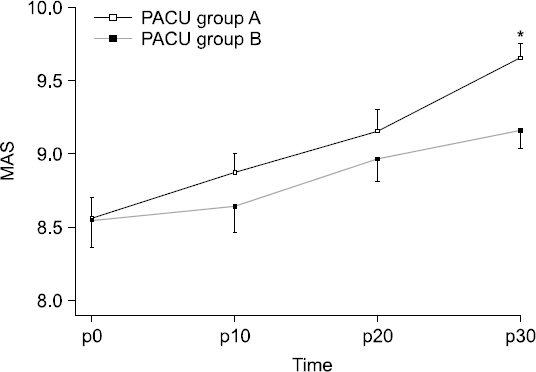
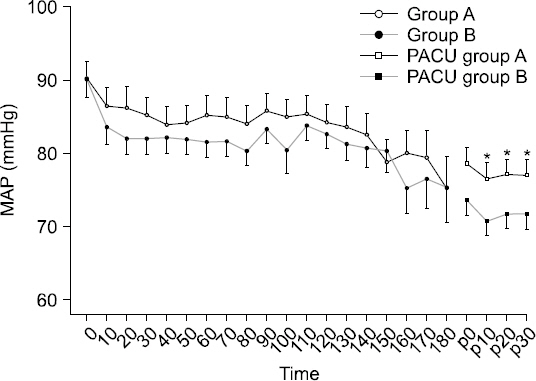
Length of stay in the PACU was longer in Group B than in Group A (P < 0.05). The MAS was higher in Group A after 30 min in the PACU (P < 0.05). The BIS did not significantly differ between the two groups from baseline to 150 min after infusion of dexmedetomidine. BIS values were significantly higher in Group A at 160 min (P < 0.05). The mean arterial pressure in Group B was significantly lower in the PACU.
CONCLUSIONS
Length of stay in the PACU was longer in Group B than in Group A (P < 0.05). The MAS was higher in Group A after 30 min in the PACU (P < 0.05). The BIS did not significantly differ between the two groups from baseline to 150 min after infusion of dexmedetomidine. BIS values were significantly higher in Group A at 160 min (P < 0.05). The mean arterial pressure in Group B was significantly lower in the PACU.
MeSH Terms
Figure
Reference
-
1. Crowninshield RD, Rosenberg AG, Sporer SM. Changing demographics of patients with total joint replacement. Clin Orthop Relat Res. 2006; 443:266–72. DOI: 10.1097/01.blo.0000188066.01833.4f. PMID: 16462450.2. Guay J, Choi P, Suresh S, Albert N, Kopp S, Pace NL. Neuraxial blockade for the prevention of postoperative mortality and major morbidity: an overview of Cochrane systematic reviews. Cochrane Database Syst Rev. 2014; 1:CD010108. DOI: 10.1002/14651858.CD010108.pub2.3. Liu J, Ma C, Elkassabany N, Fleisher LA, Neuman MD. Neuraxial anesthesia decreases postoperative systemic infection risk compared with general anesthesia in knee arthroplasty. Anesth Analg. 2013; 117:1010–6. DOI: 10.1213/ANE.0b013e3182a1bf1c. PMID: 24023024. PMCID: PMC3800057.4. Pugely AJ, Martin CT, Gao Y, Mendoza-Lattes S, Callaghan JJ. Differences in short-term complications between spinal and general anesthesia for primary total knee arthroplasty. J Bone Joint Surg Am. 2013; 95:193–9. DOI: 10.2106/JBJS.K.01682. PMID: 23269359.5. Farag E, Dilger J, Brooks P, Tetzlaff JE. Epidural analgesia improves early rehabilitation after total knee replacement. J Clin Anesth. 2005; 17:281–5. DOI: 10.1016/j.jclinane.2004.08.008. PMID: 15950853.6. Zeyneloglu P, Pirat A, Candan S, Kuyumcu S, Tekin I, Arslan G. Dexmedetomidine causes prolonged recovery when compared with midazolam/fentanyl combination in outpatient shock wave lithotripsy. Eur J Anaesthesiol. 2008; 25:961–7. DOI: 10.1017/S0265021508004699. PMID: 18538051.7. American Society of Anesthesiologists Task Force on Sedation and Analgesia by Non-Anesthesiologistss. Practice guidelines for sedation and analgesia by non-anesthesiologists. Anesthesiology. 2002; 96:1004–17. DOI: 10.1097/00000542-200204000-00031. PMID: 11964611.8. Arain SR, Ebert TJ. The efficacy, side effects, and recovery characteristics of dexmedetomidine versus propofol when used for intraoperative sedation. Anesth Analg. 2002; 95:461–6. DOI: 10.1097/00000539-200208000-00042.9. Park JW, Han JU, Shinn HK, Jung JK, Cha YD, Kang SA, et al. The effect of intravenous dexmedetomidine on the duration of brachial plexus block. Anesth Pain Med. 2012; 7:307–11.10. Phelps JR, Russell A, Lupa MC, McNaull P, Pittenger S, Ricketts K, et al. High-dose dexmedetomidine for noninvasive pediatric procedural sedation and discharge readiness. Paediatr Anaesth. 2015; 25:877–82. DOI: 10.1111/pan.12569. PMID: 25565076.11. Makary L, Vornik V, Finn R, Lenkovsky F, McClelland AL, Thurmon J, et al. Prolonged recovery associated with dexmedetomidine when used as a sole sedative agent in office-based oral and maxillofacial surgery procedures. J Oral Maxillofac Surg. 2010; 68:386–91. DOI: 10.1016/j.joms.2009.09.107. PMID: 20116712.12. Kuang Y, Zhang RR, Pei Q, Tan HY, Guo CX, Huang J, et al. Pharmacokinetic and pharmacodynamic study of dexmedetomidine in elderly patients during spinal anesthesia. Int J Clin Pharmacol Ther. 2015; 53:1005–14. DOI: 10.5414/CP202443. PMID: 26413731.13. Ok HG, Baek SH, Baik SW, Kim HK, Shin SW, Kim KH. Optimal dose of dexmedetomidine for sedation during spinal anesthesia. Korean J Anesthesiol. 2013; 64:426–31. DOI: 10.4097/kjae.2013.64.5.426. PMID: 23741565. PMCID: PMC3668104.14. Tufanogullari B, White PF, Peixoto MP, Kianpour D, Lacour T, Griffin J, et al. Dexmedetomidine infusion during laparoscopic bariatric surgery: the effect on recovery outcome variables. Anesth Analg. 2008; 106:1741–8. DOI: 10.1213/ane.0b013e318172c47c. PMID: 18499604.15. Lee S, Kim BH, Lim K, Stalker D, Wisemandle W, Shin SG, et al. Pharmacokinetics and pharmacodynamics of intravenous dexmedetomidine in healthy Korean subjects. J Clin Pharm Ther. 2012; 37:698–703. DOI: 10.1111/j.1365-2710.2012.01357.x. PMID: 22650799.16. Sentürk M, Güçyetmez B, Ozkan-Seyhan T, Karadeniz M, Dinçer S, Akpir D, et al. Comparison of the effects of thoracic and lumbar epidural anaesthesia on induction and maintenance doses of propofol during total i.v anaesthesia. Br J Anaesth. 2008; 101:255–60. DOI: 10.1093/bja/aen160. PMID: 18534970.17. Ishiyama T, Kashimoto S, Oguchi T, Yamaguchi T, Okuyama K, Kumazawa T. Epidural ropivacaine anesthesia decreases the bispectral index during the awake phase and sevoflurane general anesthesia. Anesth Analg. 2005; 100:728–32. DOI: 10.1213/01.ANE.0000159868.06847.47. PMID: 15728060.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Fatal pulmonary aspiration during balanced sedation with dexmedetomidine and midazolam: A case report
- Dexmedetomidine intravenous sedation using a patient-controlled sedation infusion pump: a case report
- Dexmedetomidine combined with midazolam vs. dexmedetomidine alone for sedation during spinal anesthesia
- Effect of Age on Optimal Clinical Dose of Dexmedetomidine Sedation
- Optimal dose of dexmedetomidine for sedation during spinal anesthesia