J Korean Acad Prosthodont.
2016 Oct;54(4):431-437. 10.4047/jkap.2016.54.4.431.
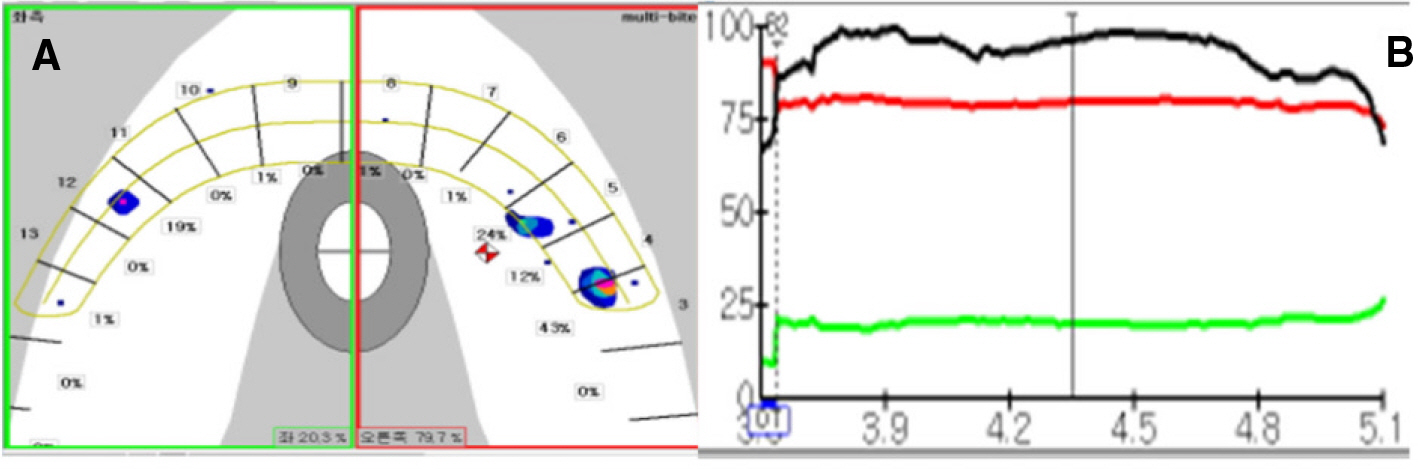
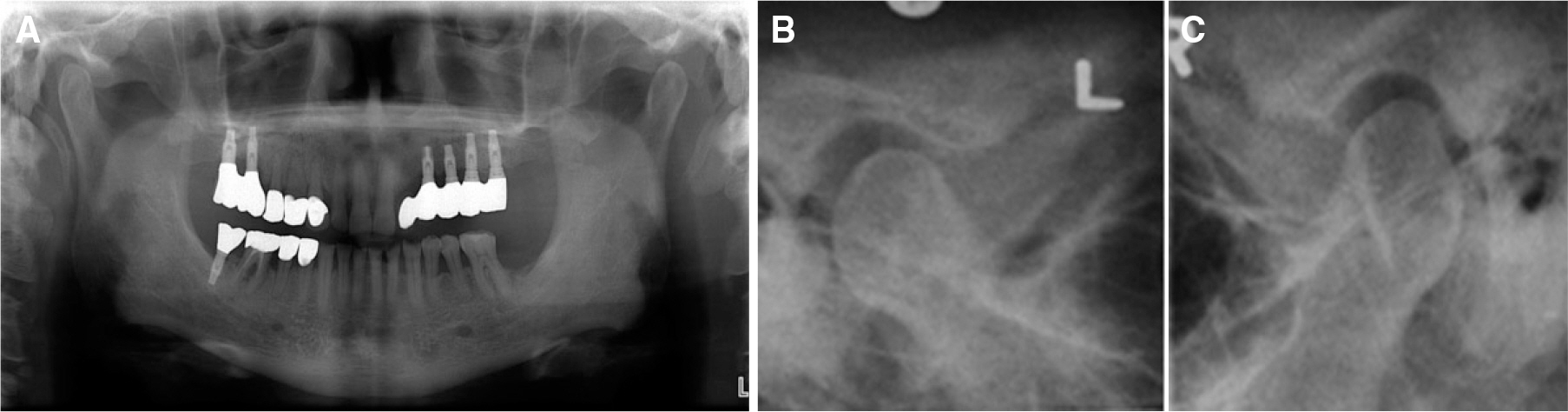
Re-restoration of temporomandibular joint disorder acquired after implant prosthetic restoration using T-Scan: A case report
- Affiliations
-
- 1Department of Prosthodontics, School of Dentistry, Chosun University, Gwangju, Republic of Korea. lkj1998@chosun.ac.kr
- KMID: 2388223
- DOI: http://doi.org/10.4047/jkap.2016.54.4.431
Abstract
- In cases of extensive prosthetic restoration, correction of occlusal contact is often needed, as it is the essential component for a successful restoration. If occlusal contact is given incorrectly, various symptoms of occlusal trauma can occur of which temporomandibular joint disorder (TMD) is one of them. As one of the common symptoms of TMD, patients may suffer with masticatory muscle disorder and temporomandibular joint pain. This case presents satisfactory results for the improvement of masticatory muscles and temporomandibular joint pain of a TMD patient, caused by incorrect occlusal contact of the restoration, by replacing the prosthesis after occlusion correction.
MeSH Terms
Figure
Cited by 1 articles
-
An epidemiological study on the prevalence of temporomandibular disorder and associated history and problems in Nepalese subjects
Dinesh Rokaya, Kanokwan Suttagul, Shraddha Joshi, Bishwa Prakash Bhattarai, Pravin Kumar Shah, Shantanu Dixit
J Dent Anesth Pain Med. 2018;18(1):27-33. doi: 10.17245/jdapm.2018.18.1.27.
Reference
-
1.Dawson PE. Position paper regarding diagnosis, management, and treatment of temporomandibular disorders. The American Equilibration Society. J Prosthet Dent. 1999. 81:174–8.2.Report of the president's conference on the examination, diagnosis, and management of temporomandibular disorders. J Am Dent Assoc. 1983. 106:75–7.3.Goldstein BH. Temporomandibular disorders: a review of current understanding. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1999. 88:379–85.
Article4.Beard CC., Clayton JA. Effects of occlusal splint therapy on TMJ dysfunction. J Prosthet Dent. 1980. 44:324–35.
Article5.Mizui M., Nabeshima F., Tosa J., Tanaka M., Kawazoe T. Quantitative analysis of occlusal balance in intercuspal position using the T-Scan system. Int J Prosthodont. 1994. 7:62–71.6.Ekberg E., Vallon D., Nilner M. The efficacy of appliance therapy in patients with temporomandibular disorders of mainly myogenous origin. A randomized, controlled, short-term trial. J Orofac Pain. 2003. 17:133–9.7.Nilner M., Ekberg E., Doepel M., Andersson J., Selovuo K., Le Bell Y. Short-term effectiveness of a prefabricated occlusal appliance in patients with myofascial pain. J Orofac Pain. 2008. 22:209–18.8.Doepel M., Nilner M., Ekberg E., LE Bell Y. Long-term effectiveness of a prefabricated oral appliance for myofascial pain. J Oral Rehabil. 2012. 39:252–60.
Article9.Jung DW., Chung AY., Kim ST. Management of temporomandibular disorder. J Dent Rehabil Appl Sci. 2012. 28:441–52.10.Son MK., Kim HJ., Kang DW., Chung CH. Clinical application of T-scan III system. Oral Biol Res. 2011. 35:161–7.11.Hirano S., Okuma K., Hayakawa I. In vitro study on accuracy and repeatability of the T-Scan II system. Kokubyo Gakkai Zasshi. 2002. 69:194–201.
Article12.Yamamura M., Takahashi A., Aoki H., Takeuchi N., Endo Y., Tamaki K., Sano Y., Fujiwara S., Fujita T., Kusunoki S. A study on display and accuracy of occlusal contacts by means of T-Scan System. Kanagawa Shigaku. 1990. 25:236–41.13.Landi N., Manfredini D., Tognini F., Romagnoli M., Bosco M. Quantification of the relative risk of multiple occlusal variables for muscle disorders of the stomatognathic system. J Prosthet Dent. 2004. 92:190–5.
Article14.Troeltzsch M., Troeltzsch M., Cronin RJ., Brodine AH., Frankenberger R., Messlinger K. Prevalence and association of headaches, temporomandibular joint disorders, and occlusal interferences. J Prosthet Dent. 2011. 105:410–7.
Article15.Celic′ R., Jerolimov V. Association of horizontal and vertical overlap with prevalence of temporomandibular disorders. J Oral Rehabil. 2002. 29:588–93.
Article16.Gesch D., Bernhardt O., Kirbschus A. Association of malocclusion and functional occlusion with temporomandibular disorders (TMD) in adults: a systematic review of population-based studies. Quintessence Int. 2004. 35:211–21.17.Kirveskari P., Jamsa T., Alanen P. Occlusal adjustment and the incidence of demand for temporomandibular disorder treatment. J Prosthet Dent. 1998. 79:433–8.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Decoronation and implant restoration of ankylosed tooth resulted from anterior avulsion: A case report
- A case of removable partial denture restoration using implant supported surveyed crown in a maxillary edentulous patient
- Immediate restoration through gingiva conditioning of maxillary anterior implant installed labially: A case report
- Aesthetic prosthetic restoration through immediate implant placement and provisional restoration in the maxillary anterior region using a digital guide
- Usage of digital technique to facilitate communication between dentist, dental lab technician, and patients in diagnosis and restoration for maxillary anterior implant: a case report