Investig Clin Urol.
2017 Sep;58(5):353-358. 10.4111/icu.2017.58.5.353.
Evaluation of the incidence and risk factors associated with persistent frequency in interstitial cystitis/bladder pain syndrome and the efficacy of antimuscarinic treatment
- Affiliations
-
- 1Department of Urology, Konkuk University Medical Center, Konkuk University School of Medicine, Seoul, Korea.
- 2Department of Urology, Asan Medical Center, Ulsan University College of Medicine, Seoul, Korea. mschoo@amc.seoul.kr
- KMID: 2388052
- DOI: http://doi.org/10.4111/icu.2017.58.5.353
Abstract
- PURPOSE
To investigate the incidence and risk factors associated with persistent urinary frequency, and to evaluate the efficacy of antimuscarinic treatment.
MATERIALS AND METHODS
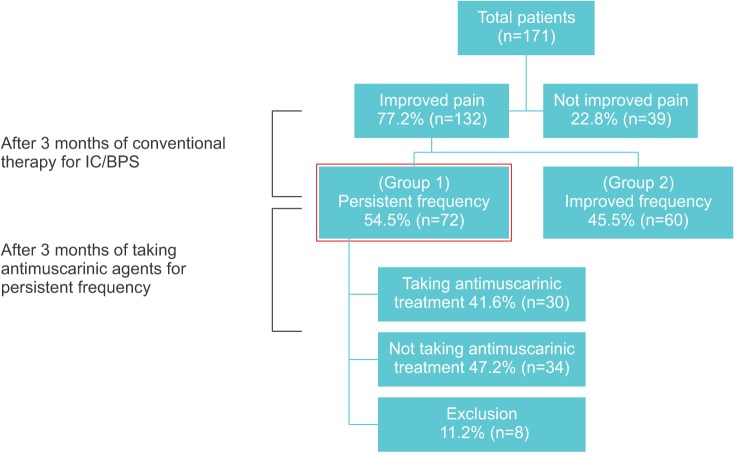
Interstitial cystitis/bladder pain syndrome (IC/BPS) patients complaining of persistent urinary frequency despite improved pain were evaluated. Before initial conventional treatment, each patient completed a voiding diary and symptom questionnaires. After conventional treatment, patients were divided according to the presence of pain and frequency. Improved pain was defined as lesser than 3 points in visual analogue scale, and persistent urinary frequency as >10 times/d. Risk factors for persistent frequency were identified through multivariate analysis. The efficacy of antimuscarinic treatment was assessed by the mean change of frequency.
RESULTS
Of 171 IC/BPS patients treated with conventional therapy, 132 had improved pain after 3 months, but 72 had persistent frequency (72 of 132, 54.5%). Patients with persistent frequency had lower voided volume (p=0.008), lower maximal flow rate (p<0.001), lower maximal bladder capacity (p=0.003), and more frequent micturition (p<0.001) at baseline compared to those with improved frequency. Patients who took antimuscarinic agents showed slightly decreased urinary frequency, from 14.6 times/d to 13.5 times/d (p=0.438) after 3 months of medication. No patients showed more than a 20% decrease in frequency with antimuscarinics.
CONCLUSIONS
About half of the patients with IC/BPS showed persistent frequency, with poor voiding function identified as a risk factor; antimuscarinic treatment was not effective in these patients.
Keyword
MeSH Terms
Figure
Reference
-
1. Hanno PM, Erickson D, Moldwin R, Faraday MM. American Urological Association. Diagnosis and treatment of interstitial cystitis/bladder pain syndrome: AUA guideline amendment. J Urol. 2015; 193:1545–1553. PMID: 25623737.
Article2. Liu HT, Jiang YH, Kuo HC. Alteration of urothelial inflammation, apoptosis, and junction protein in patients with various bladder conditions and storage bladder symptoms suggest common pathway involved in underlying pathophysiology. Low Urin Tract Symptoms. 2015; 7:102–107. PMID: 26663690.
Article3. Elliott CS, Payne CK. Interstitial cystitis and the overlap with overactive bladder. Curr Urol Rep. 2012; 13:319–326. PMID: 22965225.
Article4. Kim TH, Lee KS. Persistence and compliance with medication management in the treatment of overactive bladder. Investig Clin Urol. 2016; 57:84–93.
Article5. Warren JW, Meyer WA, Greenberg P, Horne L, Diggs C, Tracy JK. Using the International Continence Society's definition of painful bladder syndrome. Urology. 2006; 67:1138–1142. PMID: 16765165.
Article6. Hanno PM, Burks DA, Clemens JQ, Dmochowski RR, Erickson D, Fitzgerald MP, et al. AUA guideline for the diagnosis and treatment of interstitial cystitis/bladder pain syndrome. J Urol. 2011; 185:2162–2170. PMID: 21497847.
Article7. Kim A, Lim B, Song M, Choo MS. Pretreatment features to influence effectiveness of intravesical hyaluronic acid instillation in refractory interstitial cystitis/painful bladder syndrome. Int Neurourol J. 2014; 18:163–167. PMID: 25279245.
Article8. Ryu J, Pak S, Song M, Chun JY, Hong S, Choo MS. Elimination of Hunner's ulcers by fulguration in patients with interstitial cystitis: is it effective and long lasting. Korean J Urol. 2013; 54:767–771. PMID: 24255759.
Article9. Tripp DA, Nickel JC, Shoskes D, Koljuskov A. A 2-year follow-up of quality of life, pain, and psychosocial factors in patients with chronic prostatitis/chronic pelvic pain syndrome and their spouses. World J Urol. 2013; 31:733–739. PMID: 23568443.
Article10. Abrams P, Hanno P, Wein A. Overactive bladder and painful bladder syndrome: there need not be confusion. Neurourol Urodyn. 2005; 24:149–150. PMID: 15578626.
Article11. Kuo YC, Kuo HC. The urodynamic characteristics and prognostic factors of patients with interstitial cystitis/bladder pain syndrome. Int J Clin Pract. 2013; 67:863–869. PMID: 23952465.
Article12. Choi BH, Jin LH, Kim KH, Han JY, Kang JH, Yoon SM, et al. Mast cell activation and response to tolterodine in the rat urinary bladder in a chronic model of intravesical protamine sulfate and bacterial endotoxin-induced cystitis. Mol Med Rep. 2014; 10:670–676. PMID: 24859757.
Article13. Mukerji G, Yiangou Y, Grogono J, Underwood J, Agarwal SK, Khullar V, et al. Localization of M2 and M3 muscarinic receptors in human bladder disorders and their clinical correlations. J Urol. 2006; 176:367–373. PMID: 16753445.14. Pontari MA, Braverman AS, Ruggieri MR Sr. The M2 muscarinic receptor mediates in vitro bladder contractions from patients with neurogenic bladder dysfunction. Am J Physiol Regul Integr Comp Physiol. 2004; 286:R874–R880. PMID: 14751843.
Article15. Frazier EP, Peters SL, Braverman AS, Ruggieri MR Sr, Michel MC. Signal transduction underlying the control of urinary bladder smooth muscle tone by muscarinic receptors and beta-adrenoceptors. Naunyn Schmiedebergs Arch Pharmacol. 2008; 377:449–462. PMID: 18060543.16. Sun Y, Chai TC. Augmented extracellular ATP signaling in bladder urothelial cells from patients with interstitial cystitis. Am J Physiol Cell Physiol. 2006; 290:C27–C34. PMID: 16107499.
Article17. Sant GR, Kempuraj D, Marchand JE, Theoharides TC. The mast cell in interstitial cystitis: role in pathophysiology and pathogenesis. Urology. 2007; 69(4 Suppl):34–40.
Article18. Kuo HC, Jiang YH, Tsai YC, Kuo YC. Intravesical botulinum toxin-A injections reduce bladder pain of interstitial cystitis/bladder pain syndrome refractory to conventional treatment - A prospective, multicenter, randomized, double-blind, placebo-controlled clinical trial. Neurourol Urodyn. 2016; 35:609–614. PMID: 25914337.
Article19. Kuo YC, Kuo HC. O'Leary-Sant symptom index predicts the treatment outcome for onabotulinumtoxinA injections for refractory interstitial cystitis/bladder pain syndrome. Toxins (Basel). 2015; 7:2860–2871. PMID: 26264022.
Article20. Song M, Heo J, Chun JY, Bae HS, Kang JW, Kang H, et al. The paracrine effects of mesenchymal stem cells stimulate the regeneration capacity of endogenous stem cells in the repair of a bladder-outlet-obstruction-induced overactive bladder. Stem Cells Dev. 2014; 23:654–663. PMID: 24192209.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Is Urethral Pain Syndrome Really Part of Bladder Pain Syndrome?
- Update on the Pathology and Diagnosis of Interstitial Cystitis/Bladder Pain Syndrome: A Review
- Diagnosis and Management of Interstitial Cystitis/ Painful Bladder Syndrome
- The Effect of Lumbar Sympathetic Block in Interstitial Cystitis: A case report
- Intravesical Bladder Treatment and Deep Learning Applications to Improve Irritative Voiding Symptoms Caused by Interstitial Cystitis: A Literature Review