Korean J Schizophr Res.
2017 Apr;20(1):23-27. 10.16946/kjsr.2017.20.1.23.
A Case of Catatonia Later Diagnosed with NMDA Receptor Encephalitis
- Affiliations
-
- 1Department of Psychiatry, Daejeon Hankook Hospital, Daejeon, Korea.
- 2Department of Psychiatry, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea. cykim@amc.seoul.kr
- KMID: 2387929
- DOI: http://doi.org/10.16946/kjsr.2017.20.1.23
Abstract
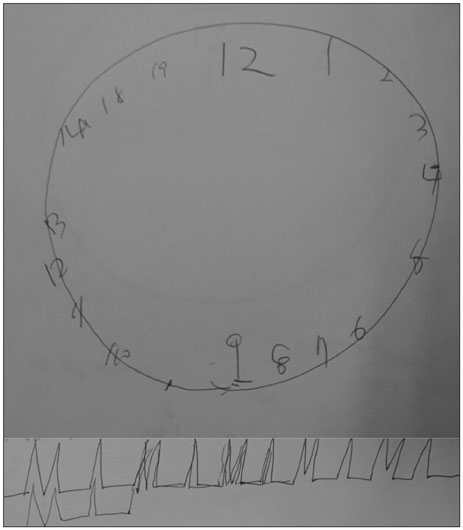
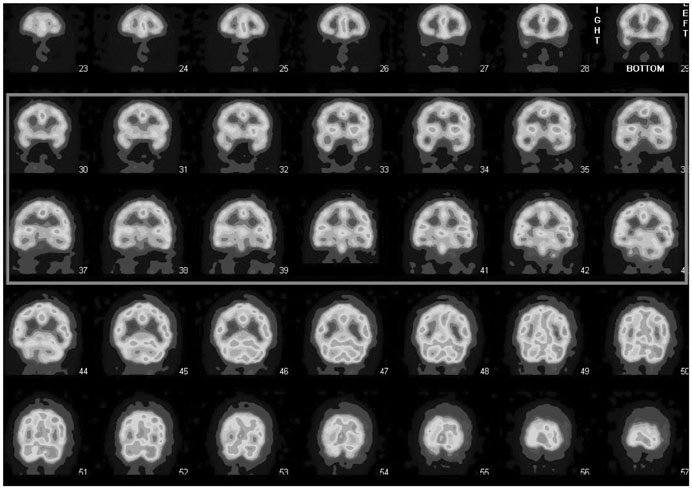
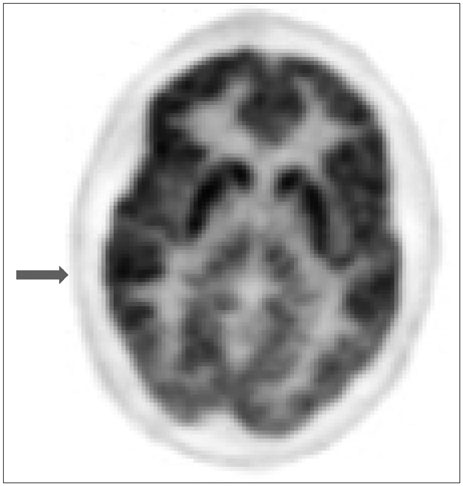
- We report a case of a young female patient with catatonic features who later turned out to be suffering from an anti-NMDA (N-methyl-D-aspartate)-receptor-antibody encephalitis. A previously healthy 21-year-old woman was admitted to psychiatric inpatient care presenting with acute psychotic behavior with catatonic features. Laboratory tests of serum and CSF (Cerebrospinal fluid), EEG (Electroencephalogram), brain MRI (Magnetic Resonance Imaging) were unremarkable except vague slow wave on EEG. However, subtle cognitive impairment at the bedside examination suggested further imaging studies to rule out possible organic etiology like autoimmune encephalitis. Brain PET (Positron Emission Tomography) and SPECT (Single Photon Emission Computed Tomography) suggested probable inflammation in the brain. In case of autoimmune encephalitis, given the severity of symptoms and worsening course, steroid pulse therapy was initiated promptly even though the diagnosis was not confirmed but presumed at that time. She recovered completely with steroid therapy. Later her disease turned out to be anti-NMDA-receptor-antibody encephalitis by the antibody test which was not available at the time of admission. Psychiatrists need to be aware of autoimmune encephalitis like anti-NMDA-receptor-antibody encephalitis in the differential diagnosis of acute psychosis with catatonic features. Subtle cognitive impairment which tends to be overlooked due to catatonic features might be a clue to suspect the organic etiology.
MeSH Terms
-
Brain
Catatonia*
Cognition Disorders
Diagnosis
Diagnosis, Differential
Electroencephalography
Encephalitis*
Female
Glycogen Storage Disease Type VI
Humans
Inflammation
Inpatients
Magnetic Resonance Imaging
N-Methylaspartate*
Psychiatry
Psychotic Disorders
Tomography, Emission-Computed, Single-Photon
Young Adult
N-Methylaspartate
Figure
Reference
-
1. Kahlbaum K. Catatonia. Baltimore: Johns Hopkins University Press;1973.2. Kraepelin E. Dementia praecox and paraphrenia. Krieger Publishing Company;1971.3. Blueler E. Dementia Praecox or The Group of Schizophrenias. New York: International Universities Press;1911.4. American Psychiatric Association. Association AP. Diagnostic and statistical manual of mental disorders. 1980.5. Morrison JR. Catatonia: retarded and excited types. Arch Gen Psychiatry. 1973; 28:39–41.6. Morrison JR. Karl Kahlbaum and catatonia. Compr Psychiatry. 1974; 15:315–316.
Article7. Taylor MA, Abrams R. Catatonia: prevalence and importance in the manic phase of manic-depressive illness. Arch Gen Psychiatry. 1977; 34:1223–1225.8. Abrams R, Taylor MA, Stolurow KC. Catatonia and mania: patterns of cerebral dysfunction. Biol Psychiatry. 1979.9. Abrams R, Taylor MA. Catatonia: a prospective clinical study. Arch Gen Psychiatry. 1976; 33:579–581.10. Gelenberg A. The catatonic syndrome. Lancet. 1976; 307:1339–1341.
Article11. Fink M, Taylor MA. Catatonia: a separate category in DSM-IV? 1991.12. Association AP. Diagnostic and statistical manual of mental disorders (DSM). Washington, DC: American Psychiatric Association;1994. p. 143–147.13. Tandon AP, Heckers S, Bustillo J, Barch DM, Gaebel W, Gur RE, et al. Catatonia in DSM-5. Schizophr Res. 2013; 150:26–30.
Article14. Association AP. Diagnostic and Statistical Manual of Mental Disorders (DSM-5®). Am Psychiatr Pub. 2013.15. Fink M, Taylor M. Catatonia: A Clinician's Guide to Diagnosis and Treatment. Camb Univ Press. 2003.16. Rao NP, Kasal V, Mutalik NR, Behere RV, Venkatasubramanian G, Varambally S, et al. Has Kahlbaum syndrome disappeared or is it underdiagnosed? Reexamining the nosology of catatonia. J ECT. 2012; 28:62–63.17. Daniels J. Catatonia: clinical aspects and neurobiological correlates. J Neuropsychiatry Clin Neurosci. 2009; 21:371–380.
Article18. Kroll KE, Kroll DS, Pope JV, Tibbles CD. Catatonia in the Emergency Department. J Emerg Med. 2012.
Article19. Ungvari GS, Kau LS, Wai-Kwong T, Shing NF. The pharmacological treatment of catatonia: an overview. Eur Arch Psychiatry Clin Neurosci. 2001; 251:31–34.
Article20. Rohland BM, Carroll BT, Jacoby RG, ECT in. ECT in the treatment of the catatonic syndrome. J Affect Disord. 1993; 29:255–261.
Article21. Rosebush PI, Mazurek MF. Current Clinical Neurology: Psychiatry for Neurologists. Totowa: Humana Press Inc;2006. p. 81–92.22. Fawcett RG. Acute psychosis associated with anti-NMDA-receptor antibodies and bilateral ovarian teratomas: a case report. J Clin Psychiatry. 2010; 71:504.
Article23. Consoli A, Ronen K, An-Gourfinkel I, Barbeau M, Marra D, Costedoat-Chalumeau N, et al. Malignant catatonia due to anti-NMDA-receptor encephalitis in a 17-year-old girl: case report. Child Adolesc Psychiatry Ment Health. 2011; 5:15.
Article24. Waxman EA, Lynch DR. N-methyl-D-aspartate receptor subtypes: multiple roles in excitotoxicity and neurological disease. Neuroscientist. 2005; 11:37–49.
Article25. Coyle JT. Glutamate and schizophrenia: beyond the dopamine hypothesis. Cell Mol Neurobiol. 2006; 26:365–384.
Article26. Vincent A, Bien CG. Anti-NMDA-receptor encephalitis: a cause of psychiatric, seizure, and movement disorders in young adults. Lancet Neurol. 2008; 7:1074–1075.
Article27. Wandinger KP, Saschenbrecker S, Stoecker W, Dalmau J. Anti-NMDA-receptor encephalitis: a severe, multistage, treatable disorder presenting with psychosis. J Neuroimmunol. 2011; 231:86–91.
Article28. Manahan-Vaughan D, von Haebler D, Winter C, Juckel G, Heinemann U. A single application of MK801 causes symptoms of acute psychosis, deficits in spatial memory, and impairment of synaptic plasticity in rats. Hippocampus. 2008; 18:125–134.
Article29. Dalmau J, Gleichman AJ, Hughes EG, Rossi JE, Peng X, Lai M, et al. Anti-NMDA-receptor encephalitis: case series and analysis of the effects of antibodies. Lancet Neurol. 2008; 7:1091–1098.
Article30. Dalmau J, Lancaster E, Martinez-Hernandez E, Rosenfeld MR, Balice-Gordon R. Clinical experience and laboratory investigations in patients with anti-NMDAR encephalitis. Lancet Neurol. 2011; 10:63–74.
Article31. Titulaer MJ, McCracken L, Gabilondo I, Armangué T, Glaser C, Iizuka T, et al. Treatment and prognostic factors for long-term outcome in patients with anti-NMDA receptor encephalitis: an observational cohort study. Lancet Neurol. 2013; 12:157–165.
Article32. Padma S, Sundaram PS, Marmattom BV. PET/CT in the evaluation of anti-NMDA-receptor encephalitis: What we need to know as a NM physician. Indian J Nucl Med. 2011; 26:99–101.
Article33. Frechette ES, Zhou L, Galetta SL, Chen L, Dalmau J. Prolonged follow-up and CSF antibody titers in a patient with anti-NMDA receptor encephalitis. Neurology. 2011; 76:S64–S66.
Article34. Shin KS, Cheon EJ, Lee SJ. A Case of Paraneoplastic Limbic Encephalitis Presented with Schizophrenic Symptoms. J Korean Neuropsychiatr Assoc. 2015; 54:596–599.
Article35. Lee HS, Kim SW, Chung SJ, Yoo HS, Lee PH, Choi SA. Anti-NMDA receptor encephalitis which has shown clinical symptoms of schizophrenia. J Korean Neurol Assoc. 2013; 31:115–117.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- GABA(A)-NMDA Hypothesis and Pharmacotherapy of Catatonia
- Anesthesia for ovarian teratoma resection using remimazolam and remifentanil in a patient with anti-N-methyl-D-aspartate receptor encephalitis -two case reports-
- Anti-N-Methyl-D-Aspartate Receptor Encephalitis Presenting Progressive Dyslexia: A Case Report
- Anti-NMDA Receptor Encephalitis Which Has Shown Clinical Symptoms of Schizophrenia
- Anti-N-methyl-D-aspartate Receptor Encephalitis after Herpes Simplex Virus Infection