Korean Circ J.
2017 May;47(3):366-376. 10.4070/kcj.2016.0384.
Antiplatelet Therapy Combinations and Thrombogenicity in Patients with Non-Valvular Atrial Fibrillation
- Affiliations
-
- 1Department of Internal Medicine, Gyeongsang National University School of Medicine, Cardiovascular Center, Gyeongsang National University Changwon Hospital, Changwon, Korea. cwakch@naver.com
- 2Department of Internal Medicine, Gyeongsang National University School of Medicine, Gyeongsang National University Hospital, Jinju, Korea.
- 3Department of Laboratory Medicine, Gyeongsang National University Hospital, Gyeongsang National University School of Medicine, Jinju, Korea.
- KMID: 2385391
- DOI: http://doi.org/10.4070/kcj.2016.0384
Abstract
- BACKGROUND AND OBJECTIVES
Combination antiplatelet therapy reduces the risk of ischemic stroke compared with aspirin monotherapy in non-valvular atrial fibrillation (NVAF) patients. The underlying mechanism, however, remains unclear. In addition, the association between platelet inhibition and thrombogenicity in NVAF has not been evaluated.
SUBJECTS AND METHODS
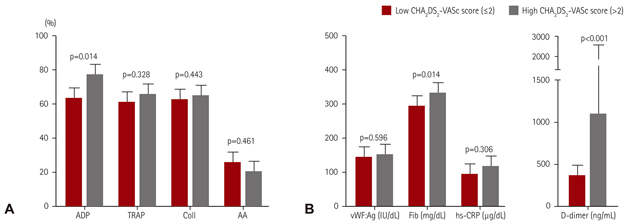
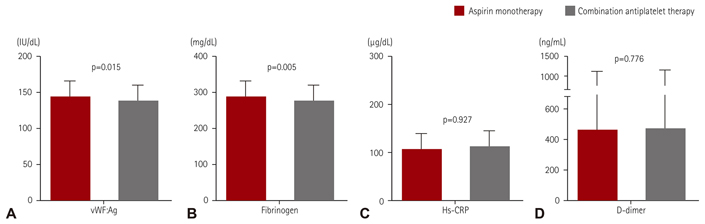
We randomized 60 patients with NVAF that were taking 100 mg of aspirin daily (>1 month) to adding 75 mg of clopidogrel daily (CLPD group), 100 mg of cilostazol twice daily (CILO group), or 1000 mg of omega-3 polyunsaturated fatty acid twice daily (PUFA group). Biomarkers (von Willebrand factor antigen [vWF:Ag], fibrinogen, D-dimer, and high-sensitivity C-reactive protein [hs-CRP]) and platelet reactivity (PR), which were the levels stimulated by adenosine diphosphate (ADP), thrombin-receptor agonist peptide, collagen, and arachidonic acid, were measured at baseline and 30-day follow-up.
RESULTS
Combination antiplatelet therapy significantly reduced vWF:Ag and fibrinogen levels (7.7 IU/dL, p=0.015 and 15.7 mg/dL, p=0.005, respectively), but no changes were found in D-dimer and hs-CRP levels. The CLPD and CILO groups showed fibrinogen and vWF:Ag level reductions (24.9 mg/dL, p=0.015 and 9.3 IU/dL, p=0.044, respectively), whereas the PUFA group did not show any differences in biomarkers. Irrespective of regimen, the changes in fibrinogen and vWF:Ag levels were mainly associated with the change in ADP-mediated PR (r=0.339, p=0.008 and r=0.322, p=0.012, respectively).
CONCLUSION
In patients with NVAF, combination antiplatelet therapy showed reductions for vWF:Ag and fibrinogen levels, which may be associated with the inhibitory levels of ADP-mediated PR. The clinical implications of these findings need to be evaluated in future trials.
MeSH Terms
-
Adenosine Diphosphate
Arachidonic Acid
Aspirin
Atrial Fibrillation*
Biomarkers
Blood Platelets
C-Reactive Protein
Collagen
Fibrinogen
Follow-Up Studies
Humans
Platelet Aggregation Inhibitors
Stroke
Adenosine Diphosphate
Arachidonic Acid
Aspirin
Biomarkers
C-Reactive Protein
Collagen
Fibrinogen
Platelet Aggregation Inhibitors
Figure
Cited by 1 articles
-
Aspirin for Primary Prevention of Cardiovascular Disease
Ji Hye Kim, Min Jung Shim, So-Young Lee, Jisu Oh, Sang Hoon Kim
J Lipid Atheroscler. 2019;8(2):162-172. doi: 10.12997/jla.2019.8.2.162.
Reference
-
1. Watson T, Shantsila E, Lip GY. Mechanisms of thrombogenesis in atrial fibrillation: Virchow's triad revisited. Lancet. 2009; 373:155–166.2. Furie B, Furie BC. Mechanisms of thrombus formation. N Engl J Med. 2008; 359:938–949.3. McFadyen JD, Jackson SP. Differentiating haemostasis from thrombosis for therapeutic benefit. Thromb Haemost. 2013; 110:859–867.4. Kirchhof P, Benussi S, Kotecha D, et al. 2016 ESC guidelines for the management of atrial fibrillation developed in collaboration with EACTS. Eur Heart J. 2016; 37:2893–2962.5. January CT, Wann LS, Alpert JS, et al. 2014 AHA/ACC/HRS guideline for the management of patients with atrial fibrillation: executive summary: a report of the American College of Cardiology/American Heart Association task force on practice guidelines and the Heart Rhythm Society. Circulation. 2014; 130:2071–2104.6. Ruff CT, Giugliano RP, Braunwald E, et al. Comparison of the efficacy and safety of new oral anticoagulants with warfarin in patients with atrial fibrillation: a meta-analysis of randomised trials. Lancet. 2014; 383:955–962.7. Bassand JP, Accetta G, Camm AJ, et al. Two-year outcomes of patients with newly diagnosed atrial fibrillation: results from GARFIELD-AF. Eur Heart J. 2016; 37:2882–2889.8. Son MK, Lim NK, Cho MC, Park HY. Incidence and risk factors for atrial fibrillation in Korea: the national health insurance service database (2002–2010). Korean Circ J. 2016; 46:515–521.9. Sabir I, Khavandi K, Brownrigg J, Camm AJ. Oral anticoagulants for Asian patients with atrial fibrillation. Nat Rev Cardiol. 2014; 11:290–303.10. Suzuki S, Yamashita T, Kato T, et al. Incidence of major bleeding complication of warfarin therapy in Japanese patients with atrial fibrillation. Circ J. 2007; 71:761–765.11. Oh S, Goto S, Accetta G, et al. Vitamin K antagonist control in patients with atrial fibrillation in Asia compared with other regions of the world: real-world data from the GARFIELD-AF registry. Int J Cardiol. 2016; 223:543–547.12. Choi JH, Cha JK, Huh JT. Adenosine diphosphate-induced platelet aggregation might contribute to poor outcomes in atrial fibrillation-related ischemic stroke. J Stroke Cerebrovasc Dis. 2014; 23:e215–e220.13. Järemo P, Eriksson M, Lindahl TL, Nilsson S, Milovanovic M. Platelets and acute cerebral infarction. Platelets. 2013; 24:407–411.14. ACTIVE Investigators. Connolly SJ, Pogue J, et al. Effect of clopidogrel added to aspirin in patients with atrial fibrillation. N Engl J Med. 2009; 360:2066–2078.15. Kim D, Lee SH, Kim BJ, et al. Secondary prevention by stroke subtype: a nationwide follow-up study in 46108 patients after acute ischaemic stroke. Eur Heart J. 2013; 34:2760–2767.16. Shinohara Y, Katayama Y, Uchiyama S, et al. Cilostazol for prevention of secondary stroke (CSPS 2): an aspirin-controlled, double-blind, randomised non-inferiority trial. Lancet Neurol. 2010; 9:959–968.17. Chowdhury R, Stevens S, Gorman D, et al. Association between fish consumption, long chain omega 3 fatty acids, and risk of cerebrovascular disease: systematic review and meta-analysis. BMJ. 2012; 345:e6698.18. Larson MK, Ashmore JH, Harris KA, et al. Effects of omega-3 acid ethyl esters and aspirin, alone and in combination, on platelet function in healthy subjects. Thromb Haemost. 2008; 100:634–641.19. Lee JH, Cha JK, Lee SJ, Ha SW, Kwon SU. Addition of cilostazol reduces biological aspirin resistance in aspirin users with ischaemic stroke: a double-blind randomized clinical trial. Eur J Neurol. 2010; 17:434–442.20. Moshfegh K, Redondo M, Julmy F, et al. Antiplatelet effects of clopidogrel compared with aspirin after myocardial infarction: enhanced inhibitory effects of combination therapy. J Am Coll Cardiol. 2000; 36:699–705.21. Kim IS, Jeong YH, Kang MK. Correlation of high post-treatment platelet reactivity assessed by light transmittance aggregometry and the VerifyNow P2Y12 assay. J Thromb Thrombolysis. 2010; 30:486–495.22. ACTIVE Writing Group of the ACTIVE Investigators. Connolly S, Pogue J, et al. Clopidogrel plus aspirin versus oral anticoagulation for atrial fibrillation in the Atrial fibrillation Clopidogrel Trial with Irbesartan for prevention of Vascular Events (ACTIVE W): a randomised controlled trial. Lancet. 2006; 367:1903–1912.23. Siegbahn A, Oldgren J, Andersson U, et al. D-dimer and factor VIIa in atrial fibrillation - prognostic values for cardiovascular events and effects of anticoagulation therapy. A RE-LY substudy. Thromb Haemost. 2016; 115:921–930.24. Wu N, Chen X, Cai T, et al. Association of inflammatory and hemostatic markers with stroke and thromboembolic events in atrial fibrillation: a systematic review and meta-analysis. Can J Cardiol. 2015; 31:278–286.25. Lip GY, Nieuwlaat R, Pisters R, Lane DA, Crijns HJ. Refining clinical risk stratification for predicting stroke and thromboembolism in atrial fibrillation using a novel risk factor-based approach: the euro heart survey on atrial fibrillation. Chest. 2010; 137:263–272.26. Dewilde WJ, Oirbans T, Verheugt FW, et al. Use of clopidogrel with or without aspirin in patients taking oral anticoagulant therapy and undergoing percutaneous coronary intervention: an open-label, randomised, controlled trial. Lancet. 2013; 381:1107–1115.27. Park Y, Franchi F, Rollini F, Angiolillo DJ. Update on oral antithrombotic therapy for secondary prevention following non-ST segment elevation myocardial infarction. Trends Cardiovasc Med. 2016; 26:321–334.28. Hori M, Connolly SJ, Zhu J, et al. Dabigatran versus warfarin: effects on ischemic and hemorrhagic strokes and bleeding in Asians and non-Asians with atrial fibrillation. Stroke. 2013; 44:1891–1896.29. Patel MR, Mahaffey KW, Garg J, et al. Rivaroxaban versus warfarin in nonvalvular atrial fibrillation. N Engl J Med. 2011; 365:883–891.30. Hori M, Matsumoto M, Tanahashi N, et al. Rivaroxaban vs. warfarin in Japanese patients with atrial fibrillation - the J-ROCKET AF study -. Circ J. 2012; 76:2104–2111.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Clinical Characteristics and Management in Elderly Patients with Atrial Fibrillation
- Relation of Right Atrial Pathology to Atrial Fibrillation in Mitral Valvular Disease
- Relation between Left Atrial Size and Atrial Fibrillation
- Anticoagulation in Atrial Fibrillation
- Is Lighter Intensity of Warfarin Therapy Enough for Korean Patients with Non-Valvular Atrial Fibrillation?