J Cardiovasc Ultrasound.
2017 Jun;25(2):63-69. 10.4250/jcu.2017.25.2.63.
Echocardiographic, Electrocardiographic Changes and Clinical Outcomes of Patients Who Respond to Cardiac Resynchronization Therapy after One Year
- Affiliations
-
- 1Division of Cardiology, Department of Internal Medicine, Seoul St. Mary's Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea. younhj@catholic.ac.kr
- 2Cardiovascular Center, Chuncheon Sacred Heart Hospital, Hallym University College of Medicine, Chuncheon, Korea.
- KMID: 2385077
- DOI: http://doi.org/10.4250/jcu.2017.25.2.63
Abstract
- BACKGROUND
Response to cardiac resynchronization therapy (CRT) is commonly assessed after 6 or 12 months. We evaluated subsequent echocardiographic changes, serial QRS duration, and clinical outcomes in patients showing delayed responses to CRT after 12 months.
METHODS
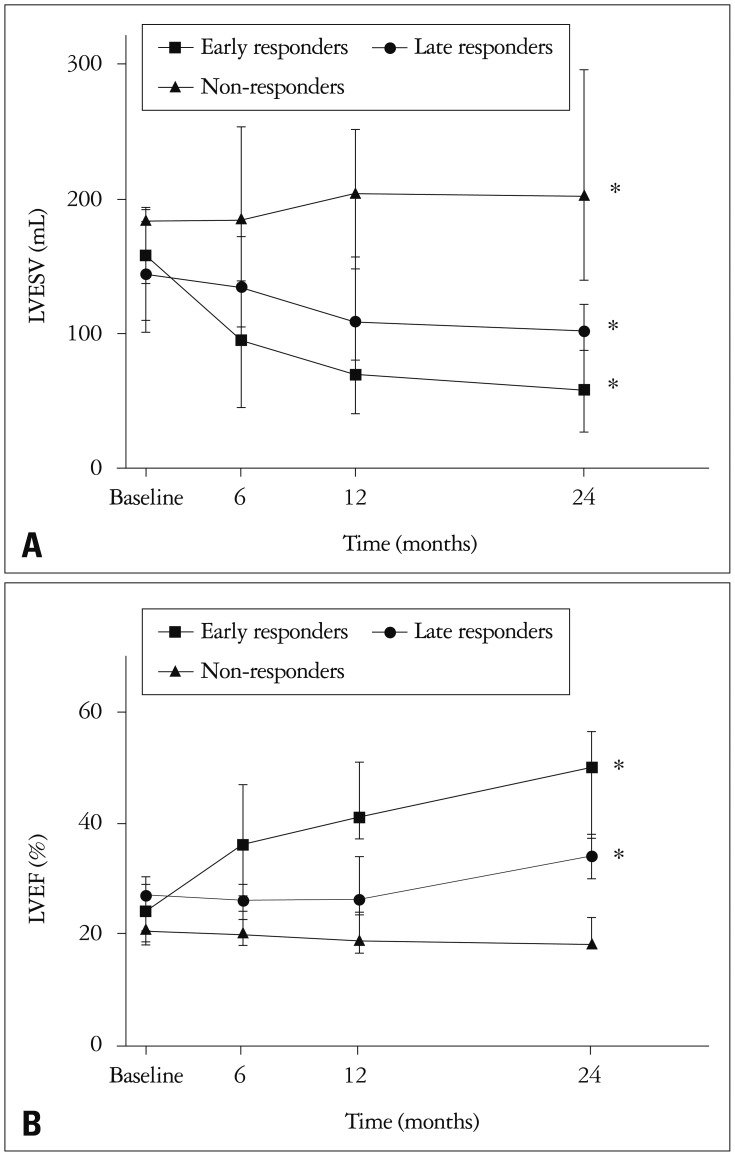
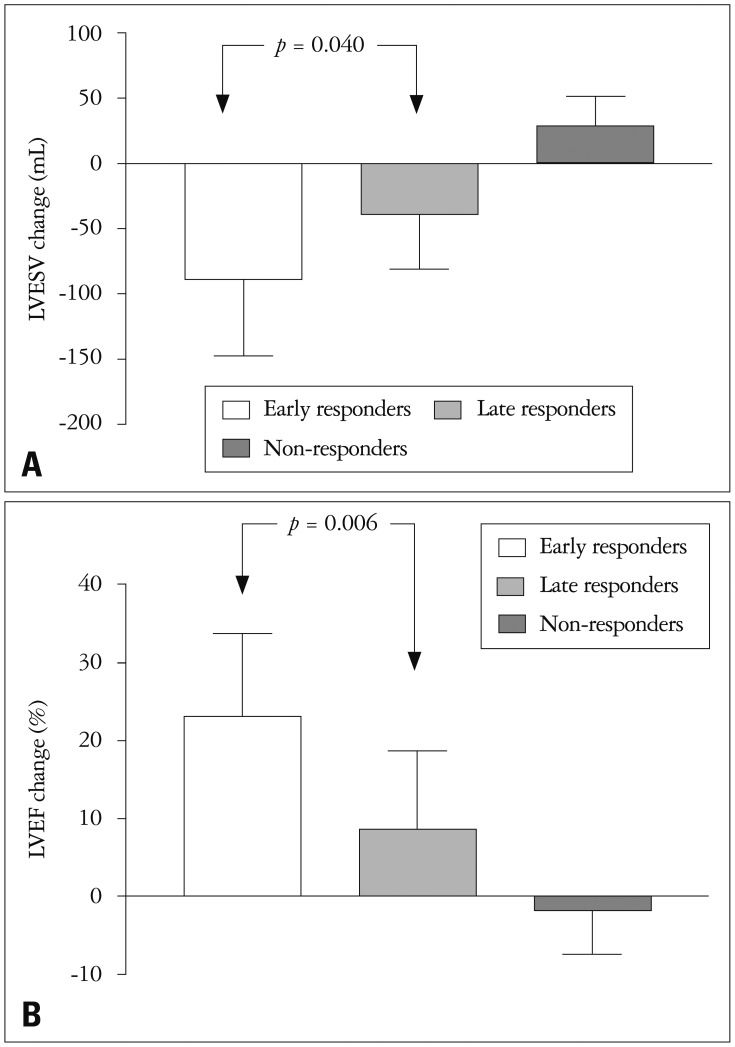
Among all patients who received CRT in Seoul St. Mary's Hospital, 36 one-year survivors were enrolled. Indicators of a positive CRT response were ≥ 15% reduction in left ventricular end-systolic volume (LVESV) or ≥ 10% increase in left ventricular ejection fraction (LVEF) on any follow up echocardiogram. We defined the early responders as patients responding before one year, the late responders as patients responding after one year, and the non-responders as patients who did not respond on any follow-up echocardiogram.
RESULTS
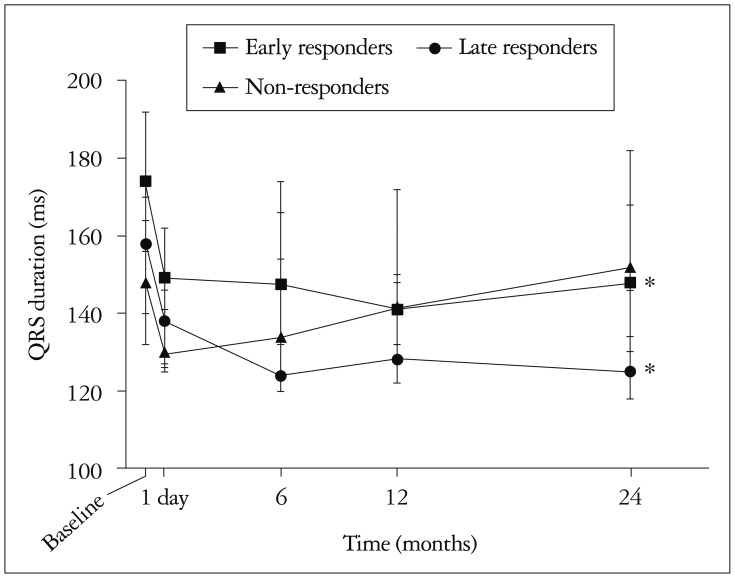
We identified 17 early responders, 10 late responders, and 9 non-responders. The late responders showed modest improvement in LVESV and LVEF at two years after CRT. QRS duration was shortened the day after CRT in all three groups. Narrowed QRS was maintained for two years in early and late responders, whereas it was continuously prolonged over time in non-responders. Incidence of all-cause death or heart failure hospitalization was comparable between early and late responders, while non-responders showed worst prognosis.
CONCLUSION
Patients responding to CRT after one year show modest echocardiographic improvement but clinical outcome is similar to early responders. Shorter baseline QRS duration and long-term maintenance of QRS duration shortening are important features of the late responders to CRT.
MeSH Terms
Figure
Reference
-
1. St John Sutton MG, Plappert T, Abraham WT, Smith AL, DeLurgio DB, Leon AR, Loh E, Kocovic DZ, Fisher WG, Ellestad M, Messenger J, Kruger K, Hilpisch KE, Hill MR; Multicenter InSync Randomized Clinical Evaluation (MIRACLE) Study Group. Effect of cardiac resynchronization therapy on left ventricular size and function in chronic heart failure. Circulation. 2003; 107:1985–1990. PMID: 12668512.2. Yu CM, Bleeker GB, Fung JW, Schalij MJ, Zhang Q, van der, Chan YS, Kong SL, Bax JJ. Left ventricular reverse remodeling but not clinical improvement predicts long-term survival after cardiac resynchronization therapy. Circulation. 2005; 112:1580–1586. PMID: 16144994.3. Chung ES, Leon AR, Tavazzi L, Sun JP, Nihoyannopoulos P, Merlino J, Abraham WT, Ghio S, Leclercq C, Bax JJ, Yu CM, Gorcsan J 3rd, St John Sutton M, De Sutter J, Murillo J. Results of the Predictors of Response to CRT (PROSPECT) trial. Circulation. 2008; 117:2608–2616. PMID: 18458170.4. Friedman DJ, Upadhyay GA, Rajabali A, Altman RK, Orencole M, Parks KA, Moore SA, Park MY, Picard MH, Ruskin JN, Singh JP, Heist EK. Progressive ventricular dysfunction among nonresponders to cardiac resynchronization therapy: baseline predictors and associated clinical outcomes. Heart Rhythm. 2014; 11:1991–1998. PMID: 25106864.5. Marfella R, Di Filippo C, Potenza N, Sardu C, Rizzo MR, Siniscalchi M, Musacchio E, Barbieri M, Mauro C, Mosca N, Solimene F, Mottola MT, Russo A, Rossi F, Paolisso G, D'Amico M. Circulating microRNA changes in heart failure patients treated with cardiac resynchronization therapy: responders vs. non-responders. Eur J Heart Fail. 2013; 15:1277–1288. PMID: 23736534.6. Ghio S, Freemantle N, Scelsi L, Serio A, Magrini G, Pasotti M, Shankar A, Cleland JG, Tavazzi L. Long-term left ventricular reverse remodelling with cardiac resynchronization therapy: results from the CARE-HF trial. Eur J Heart Fail. 2009; 11:480–488. PMID: 19287017.7. van't Sant J, Fiolet AT, ter Horst IA, Cramer MJ, Mastenbroek MH, van Everdingen WM, Mast TP, Doevendans PA, Versteeg H, Meine M. Volumetric response beyond six months of cardiac resynchronization therapy and clinical outcome. PLoS One. 2015; 10:e0124323. PMID: 25933068.8. Molhoek SG, VAN Erven L, Bootsma M, Steendijk P, Van Der Wall EE, Schalij MJ. QRS duration and shortening to predict clinical response to cardiac resynchronization therapy in patients with end-stage heart failure. Pacing Clin Electrophysiol. 2004; 27:308–313. PMID: 15009855.9. Abraham WT, Fisher WG, Smith AL, Delurgio DB, Leon AR, Loh E, Kocovic DZ, Packer M, Clavell AL, Hayes DL, Ellestad M, Trupp RJ, Underwood J, Pickering F, Truex C, McAtee P, Messenger J. MIRACLE Study Group. Multicenter InSync Randomized Clinical Evaluation. Cardiac resynchronization in chronic heart failure. N Engl J Med. 2002; 346:1845–1853. PMID: 12063368.10. Birnie DH, Tang AS. The problem of non-response to cardiac resynchronization therapy. Curr Opin Cardiol. 2006; 21:20–26. PMID: 16355025.11. Bleeker GB, Bax JJ, Fung JW, van der Wall EE, Zhang Q, Schalij MJ, Chan JY, Yu CM. Clinical versus echocardiographic parameters to assess response to cardiac resynchronization therapy. Am J Cardiol. 2006; 97:260–263. PMID: 16442375.12. Burns KV, Gage RM, Curtin AE, Bank AJ. Long-term echocardiographic response to cardiac resynchronization therapy in initial nonresponders. JACC Heart Fail. 2015; 3:990–997. PMID: 26577619.13. Zhang J, Zhang Y, Zhou X, Li J, Li Y, Zhang Y, Xu G, Xing Q, Lin S, Tang B. QRS duration shortening predicts left ventricular reverse remodelling in patients with dilated cardiomyopathy after cardiac resynchronization therapy. Acta Cardiol. 2015; 70:307–313. PMID: 26226704.14. Brabham WW, Gold MR. The role of AV and VV optimization for CRT. J Arrhythm. 2013; 29:153–161.15. Ellenbogen KA, Gold MR, Meyer TE, Fernndez Lozano I, Mittal S, Waggoner AD, Lemke B, Singh JP, Spinale FG, Van Eyk JE, Whitehill J, Weiner S, Bedi M, Rapkin J, Stein KM. Primary results from the SmartDelay determined AV optimization: a comparison to other AV delay methods used in cardiac resynchronization therapy (SMART-AV) trial: a randomized trial comparing empirical, echocardiography-guided, and algorithmic atrioventricular delay programming in cardiac resynchronization therapy. Circulation. 2010; 122:2660–2668. PMID: 21098426.16. Kosmala W, Marwick TH. Meta-analysis of effects of optimization of cardiac resynchronization therapy on left ventricular function, exercise capacity, and quality of life in patients with heart failure. Am J Cardiol. 2014; 113:988–994. PMID: 24461769.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Left Atrial Enlargement: Echocardiographic Assessment of Electrocardiographic Criteria
- Myocardial Dyssynchronicity and Cardiac Resynchronization Therapy
- Cardiac Resynchronization Therapy Defibrillator Treatment in a Child with Heart Failure and Ventricular Arrhythmia
- Implantable Cardioverter-Defibrillator and Cardiac Resynchronization Therapy
- Mid-Term Outcomes in Patients Implanted with Cardiac Resynchronization Therapy