J Korean Orthop Assoc.
2017 Jun;52(3):279-284. 10.4055/jkoa.2017.52.3.279.
Glomus Tumor Causing Knee Pain
- Affiliations
-
- 1Department of Orthopaedic Surgery, Dankook University Medical College, Cheonan, Korea. lovebio1ogy@naver.com
- KMID: 2384559
- DOI: http://doi.org/10.4055/jkoa.2017.52.3.279
Abstract
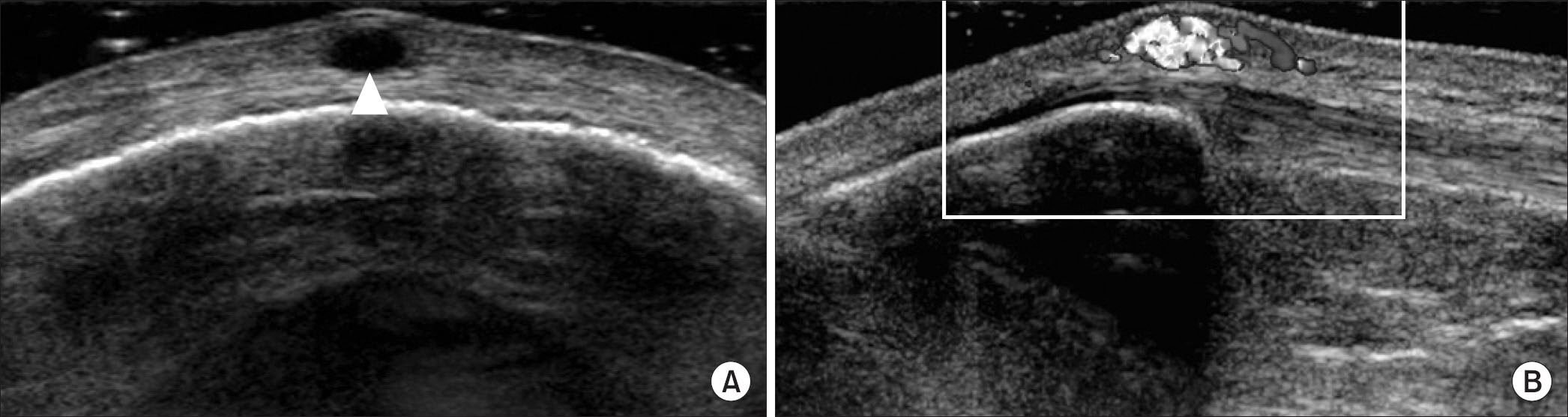
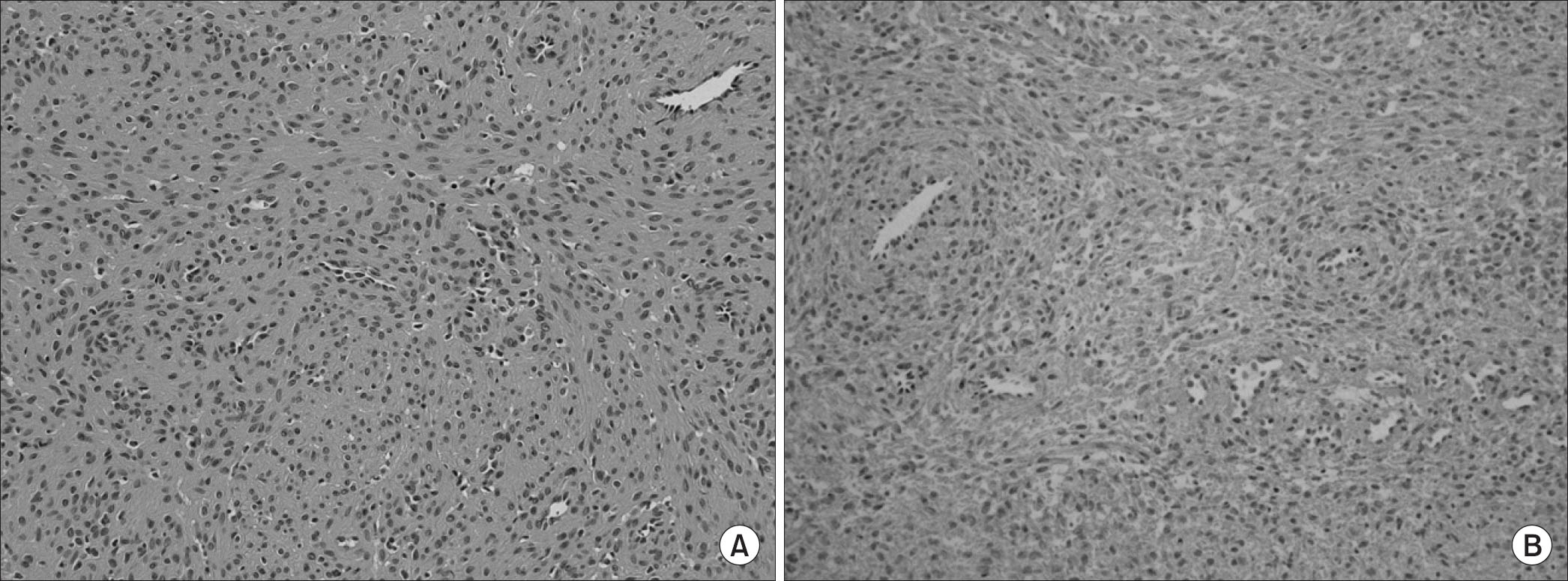
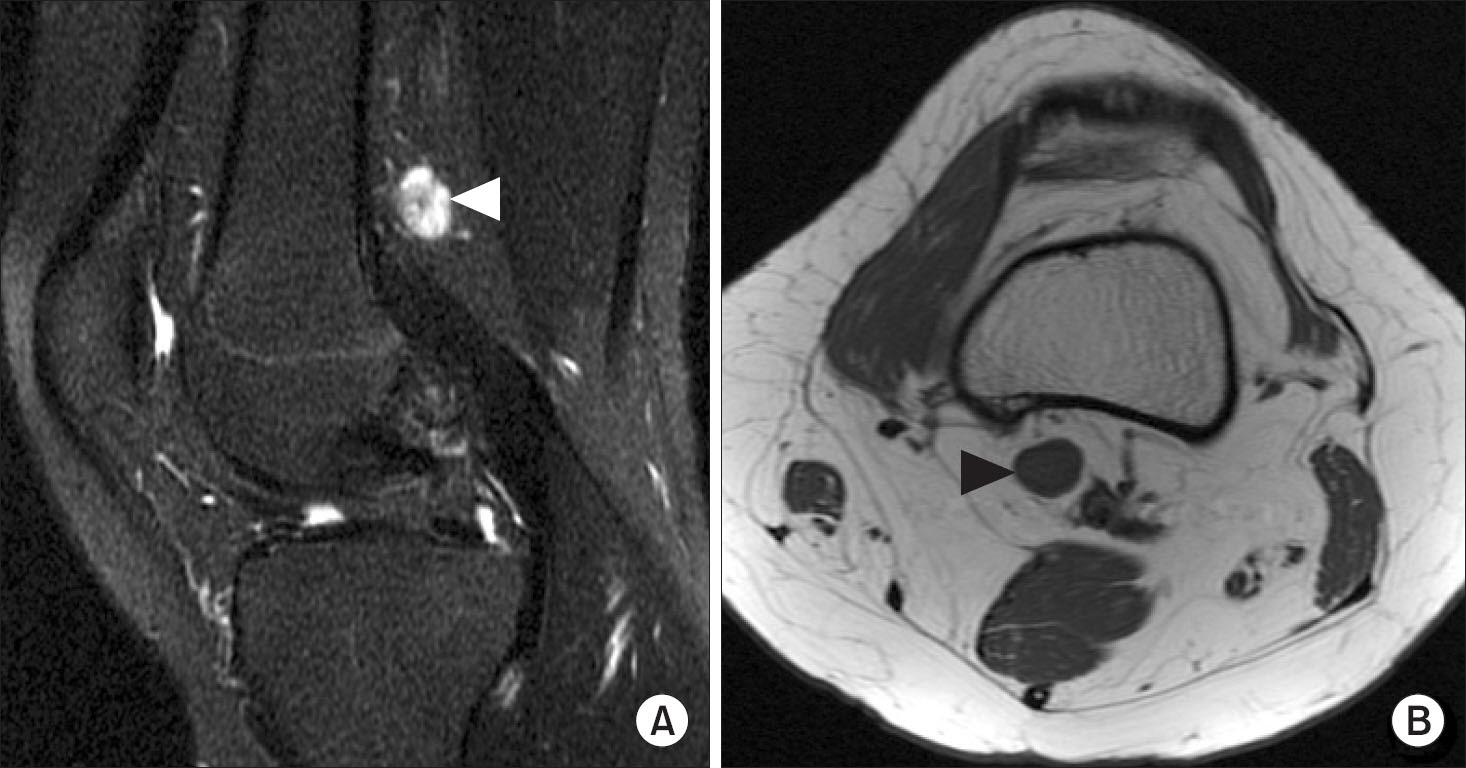
- Glomus tumor is a kind of hemangioma that occurs at the glomerulus in the subcutaneous layer. It mainly occurs at the distal hand and subungual area, and rarely at the knee joint. Pain, tenderness, and cold intolerance are known symptoms; however, symptoms in practice are not so easily detectable, and the diagnosis can be delayed if it is presented at areas other than the hand. If the diagnosis is delayed, patients could suffer extreme pain. Therefore, early diagnosis and surgical treatment are important. Ultrasound and magnetic resonance imaging were used to diagnose glomus tumor in our cases, which were found in subcutaneous tissue and muscle fascia. We claim that, for patients with persistent pain, known symptoms"”extreme pain, cold intolerance, and tenderness"”should be examined carefully and rule out glomus tumor. We report 2 cases of glomus tumors around the knee joint, which is not a common location of occurrence.
Keyword
MeSH Terms
Figure
Reference
-
1. Carroll RE, Berman AT. Glomus tumors of the hand: review of the literature and report on twenty-eight cases. J Bone Joint Surg Am. 1972; 54:691–703.2. Gombos Z, Zhang PJ. Glomus tumor. Arch Pathol Lab Med. 2008; 132:1448–52.
Article3. Takei TR, Nalebuff EA. Extradigital glomus tumour. J Hand Surg Br. 1995; 20:409–12.
Article4. Prabhakar S, Dhillon MS, Vasishtha RK, Bali K. Glomus tumor of Hoffa's fat pad and its management by arthroscopic excision. Clin Orthop Surg. 2013; 5:334–7.
Article5. Kim SH, Suh HS, Choi JH, Sung KJ, Moon KC, Koh JK. Glomus tumor: a clinical and histopathologic analysis of 17 cases. Ann Dermatol. 2000; 12:95–101.6. Seo BC, Oh DY, Park KS. . Glomus tumor in soleus muscle: a case report. J Korean Soc Plast Reconstr Surg. 2006; 33:518–20.7. Baek HJ, Lee SJ, Cho KH. . Subungual tumors: clinicopathologic correlation with US and MR imaging findings. Radiographics. 2010; 30:1621–36.
Article8. Lee MC, Seong SC, Moon YW, Park YK. Glomus tumor adjacent to patellar tendon, a case report. J Korean Knee Soc. 1996; 8:263–7.9. Lee SH, Lee MC, Seong SC, Jeong GI. Glomus tumor in the infrapatellar fat pad, a case report. J Korean Knee Soc. 2001; 13:236–9.10. Shaikh R, Alomari AI, Mulliken JB, Fishman SJ, Kozakewich HP, Chaudry G. Subfascial involvement in glomuvenous malformation. Skeletal Radiol. 2014; 43:895–7.
Article