J Endocr Surg.
2017 Jun;17(2):57-62. 10.16956/jes.2017.17.2.57.
Cohexisting Medullary and Papillary Thyroid Cancer
- Affiliations
-
- 1Division of Surgery, Department of Medicine and Surgery, University of Insubria, Varese, Italy. davide.inversini@gmail.com
- 2Division of Endocrinology, Department of Clinical Medicine, University of Insubria, Varese, Italy.
- 3Division of Histopathology, Department of Medicine and Surgery, University of Insubria, Varese, Italy.
- 4Institute of Pathology, Lausanne University Hospital (CHUV), Lausanne, Switzerland.
- 5Division of Thyroid Surgery, Jilin Provincial Key Laboratory of Surgical Translational Medicine, China-Japan Union Hospital of Jilin University, Changchun, China.
- KMID: 2383822
- DOI: http://doi.org/10.16956/jes.2017.17.2.57
Abstract
- PURPOSE
Papillary thyroid carcinomas (PTCs) and medullary thyroid carcinomas (MTCs) have always been considered different in terms of their incidence rates, cell origins, and histopathological features. Simultaneous occurrence of both disease entities is very rare.
METHODS
We describe a series of cases with simultaneous MTC and PTC occurrences in the thyroid gland.
RESULTS
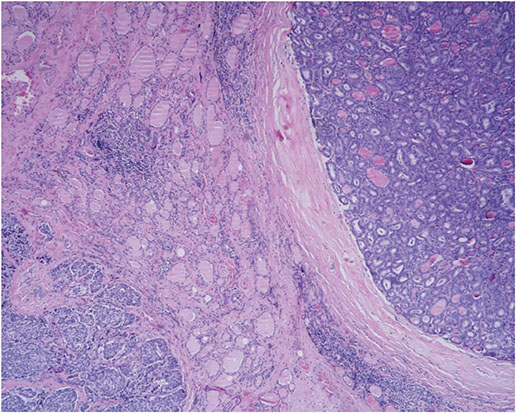
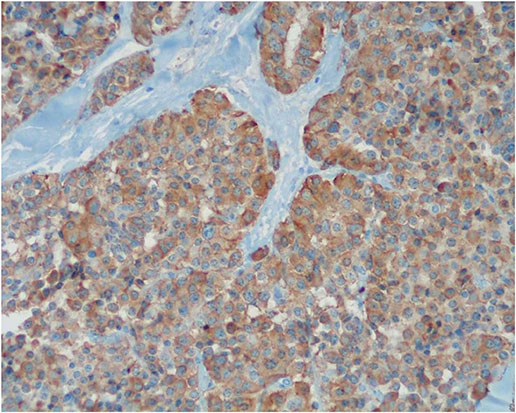
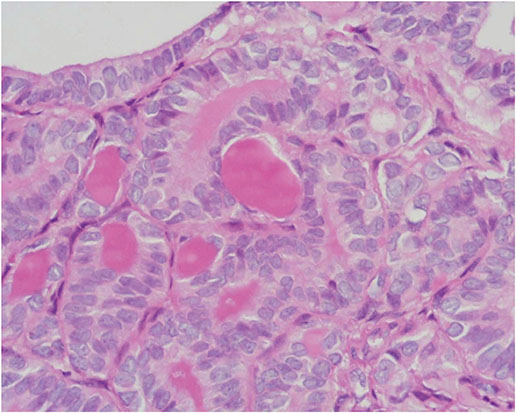
From 2,897 patients (mean age, 49.2±12.5; 81% women) who underwent thyroidectomy for cancer between 2000 and 2015, we reviewed 11 cases of simultaneous occurrence of MTCs and PTCs. Multifocal PTC with simultaneous MTC was detected in 5 of the 11 cases (45%). Of these PTC patients, 2 had 2 foci, 2 had 3 foci, and 1 had 4 foci. There was 1 case of multifocal MTC with solitary PTC. One patient presented with "composite thyroid carcinoma" with mixed features of MTCs and PTCs. Eight patients (72%) presented an association with diffuse lymphocytic thyroiditis. The sizes of the tumors were 1.95±0.23 cm vs. 1.20±0.20 cm for PTCs and MTCs, respectively (P=0.531). The prevalence of extrathyroidal extension was 33.1% vs. 30.2% for PTCs and MTCs, respectively (P=0.282). All patients underwent total thyroidectomy and central neck node dissection. Radio iodine was delivered to 44% of patients. Follow-up review revealed 9 disease-free patients and 1 with local neck recurrence, while 1 patient died due to non-thyroid reasons.
CONCLUSION
There are only 30 reports describing a total of 50 cases in the English literature regarding concurrent PTC and MTC in the same gland. This study represents one of the largest case series. Whether the incidence of another cancer in these patients is coincidental, or due to the possible activation of a common tumorigenic pathway for both follicular and parafollicular thyroid cells, remains to be elucidated.
Keyword
MeSH Terms
Figure
Reference
-
1. Hu MI, Ying AK, Jimenez C. Update on medullary thyroid cancer. Endocrinol Metab Clin North Am. 2014; 43:423–442.
Article2. Maia AL, Wajner SM, Vargas CV. Advances and controversies in the management of medullary thyroid carcinoma. Curr Opin Oncol. 2017; 29:25–32.
Article3. Merchant FH, Hirschowitz SL, Cohan P, Van Herle AJ, Natarajan S. Simultaneous occurrence of medullary and papillary carcinoma of the thyroid gland identified by fine needle aspiration. A case report. Acta Cytol. 2002; 46:762–766.
Article4. Mazziotti G, Rotondi M, Manganella G, Franco R, Capone PF, Colantuoni V, et al. Medullary thyroid cancer, papillary thyroid microcarcinoma and Graves’ disease: an unusual clinical coexistence. J Endocrinol Invest. 2001; 24:892–896.
Article5. Bounacer A, Wicker R, Caillou B, Cailleux AF, Sarasin A, Schlumberger M, et al. High prevalence of activating RET proto-oncogene rearrangements, in thyroid tumors from patients who had received external radiation. Oncogene. 1997; 15:1263–1273.
Article6. Apel RL, Alpert LC, Rizzo A. LiVolsi VA, Asa SL. A metastasizing composite carcinoma of the thyroid with distinct medullary and papillary components. Arch Pathol Lab Med. 1994; 118:1143–1147.7. Ljungberg O, Ericsson UB, Bondeson L, Thorell J. A compound follicular-parafollicular cell carcinoma of the thyroid: a new tumor entity? Cancer. 1983; 52:1053–1061.
Article8. Volante M, Papotti M, Roth J, Saremaslani P, Speel EJ, Lloyd RV, et al. Mixed medullary-follicular thyroid carcinoma. Molecular evidence for a dual origin of tumor components. Am J Pathol. 1999; 155:1499–1509.9. Rossi S, Fugazzola L, De Pasquale L, Braidotti P, Cirello V, Beck-Peccoz P, et al. Medullary and papillary carcinoma of the thyroid gland occurring as a collision tumour: report of three cases with molecular analysis and review of the literature. Endocr Relat Cancer. 2005; 12:281–289.
Article10. Tamimi DM. The association between chronic lymphocytic thyroiditis and thyroid tumors. Int J Surg Pathol. 2002; 10:141–146.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Concurrent Medullay and Papillary Carcinoma of the Thyroid
- Concurrent Papillary and Medullary Carcinoma of the Thyroid Gland
- A Case of Concurrent Papillary and Medullary Thyroid Carcinomas Detected as Recurrent Medullary Carcinoma after Initial Surgery for Papillary Carcinoma
- Medullary and Papillary Thyroid Carcinoma as a Collision Tumor: Report of Five Cases
- A Case of Concurrent Medullary and Papillary Carcinoma of the Thyroid Gland