Clin Endosc.
2017 Jan;50(1):81-86. 10.5946/ce.2016.027.
Laser Imaging Facilitates Early Detection of Synchronous Adenocarcinomas in Patients with Barrett's Esophagus
- Affiliations
-
- 1Division of Gastroenterology, Department of Internal Medicine, Jichi Medical University, Shimotsuke, Japan. osawa@jichi.ac.jp
- 2Department of Surgery, Jichi Medical University, Shimotsuke, Japan.
- KMID: 2383495
- DOI: http://doi.org/10.5946/ce.2016.027
Abstract
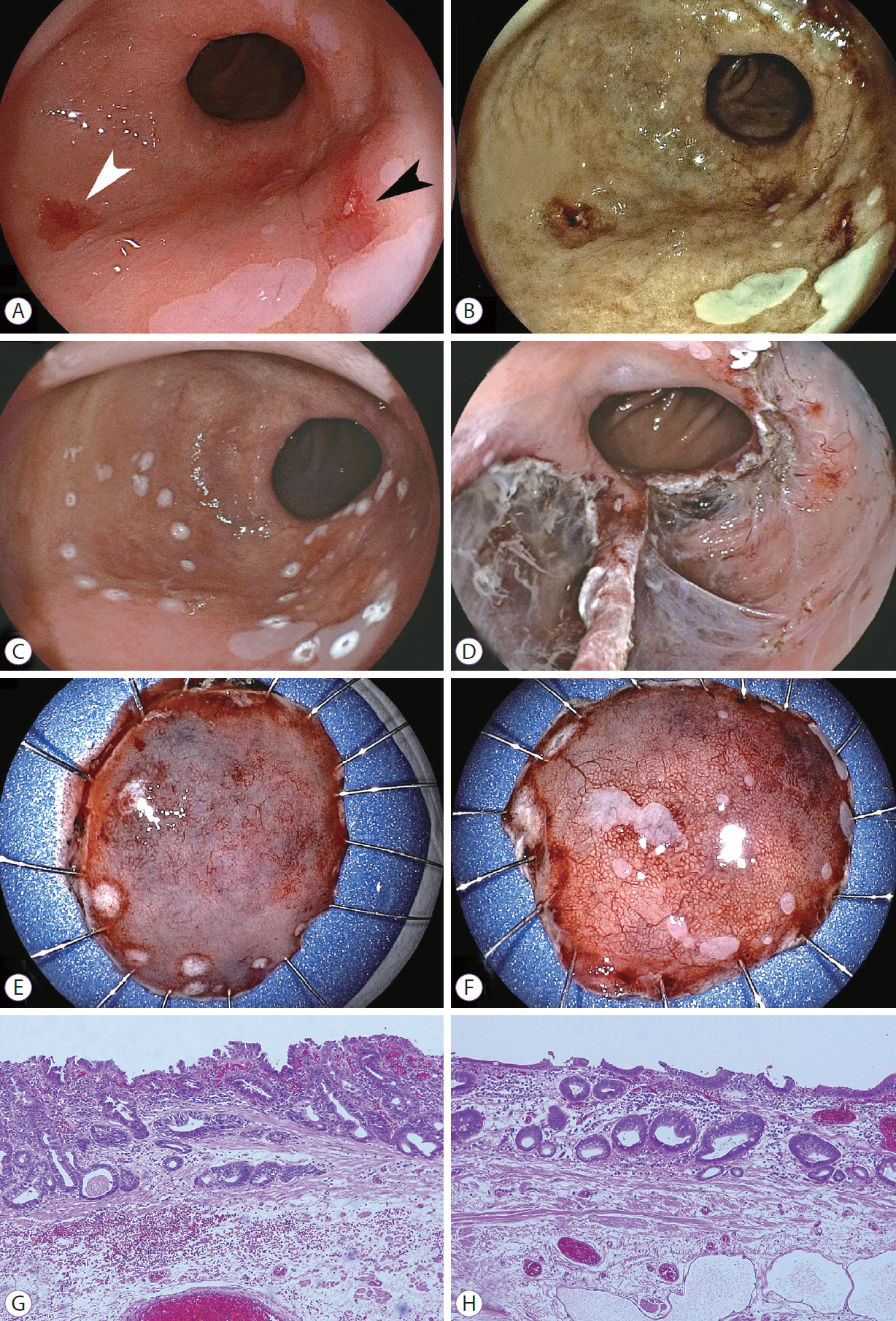
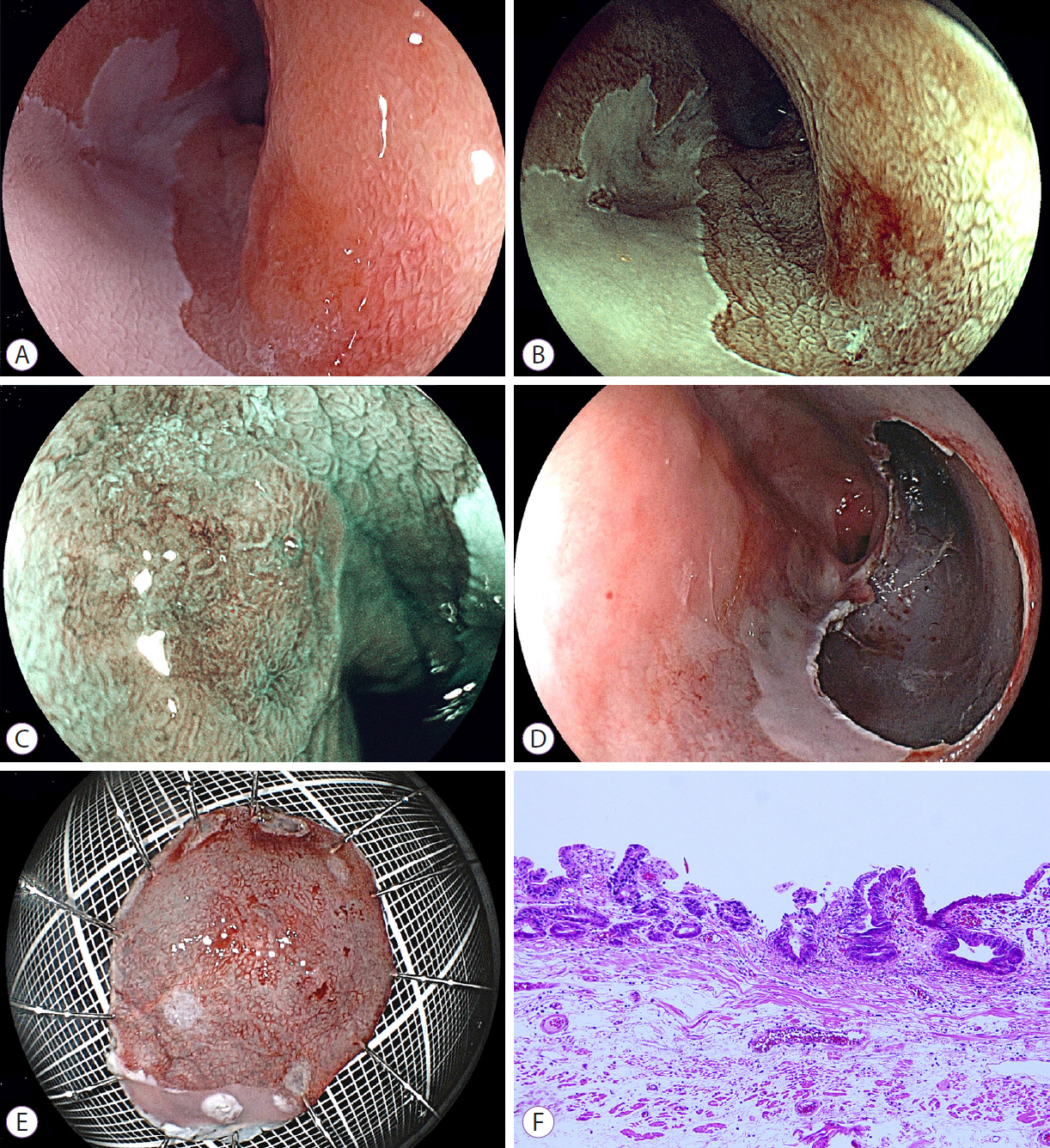
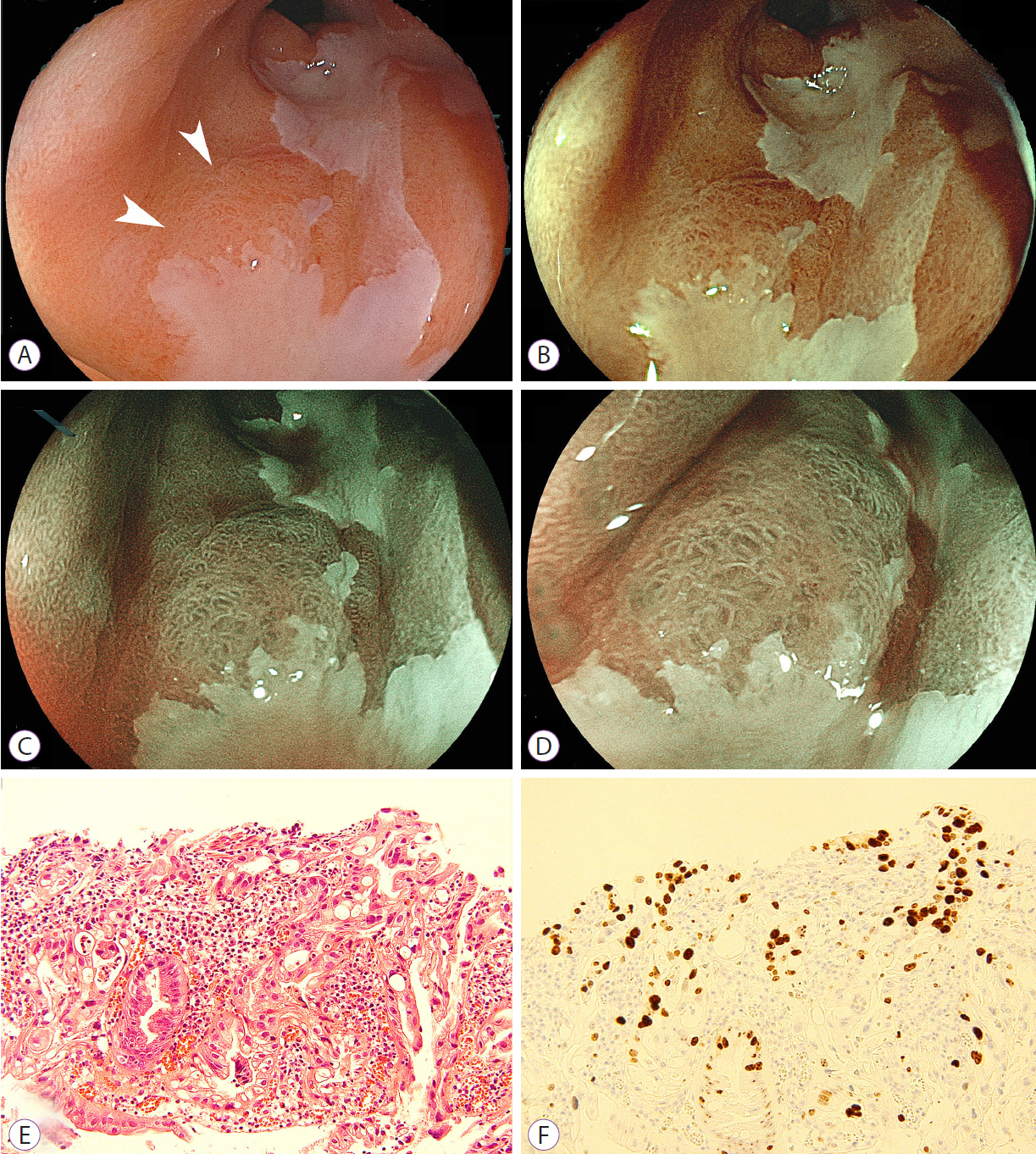
- Barrett's adenocarcinoma may occur in multiple sites, and recurrence and metachronous lesions are the major problems with endoscopic resection. Therefore, early detection of such lesions is ideal to achieve complete resection and obtain improved survival rates with minimally invasive treatment. Laser imaging systems allow multiple modalities of endoscopic imaging by using white light laser, flexible spectral imaging color enhancement (FICE), blue laser imaging (BLI), and linked color imaging even at a distant view. However, the usefulness of these modalities has not been sufficiently reported regarding Barrett's adenocarcinoma. Here, we report on a patient with three synchronous lesions followed by one metachronous lesion in a long segment with changes of Barrett's esophagus, all diagnosed with this new laser endoscopic imaging system and enhanced by using FICE and/or BLI with high contrast compared with the surrounding mucosa. Laser endoscopic imaging may facilitate the detection of malignancies in patients with early Barrett's adenocarcinoma.
Keyword
Figure
Cited by 2 articles
-
Blue Laser Imaging with a Small-Caliber Endoscope Facilitates Detection of Early Gastric Cancer
Haruo Takahashi, Yoshimasa Miura, Hiroyuki Osawa, Takahito Takezawa, Yuji Ino, Masahiro Okada, Alan Kawarai Lefor, Hironori Yamamoto
Clin Endosc. 2019;52(3):273-277. doi: 10.5946/ce.2018.100.Linked Color Imaging and Blue Laser Imaging for Upper Gastrointestinal Screening
Hiroyuki Osawa, Yoshimasa Miura, Takahito Takezawa, Yuji Ino, Tsevelnorov Khurelbaatar, Yuichi Sagara, Alan Kawarai Lefor, Hironori Yamamoto
Clin Endosc. 2018;51(6):513-526. doi: 10.5946/ce.2018.132.
Reference
-
1. Bennett C, Vakil N, Bergman J, et al. Consensus statements for management of Barrett’s dysplasia and early-stage esophageal adenocarcinoma, based on a Delphi process. Gastroenterology. 2012; 143:336–346.2. Gill RS, Singh R. Endoscopic imaging in Barrett’s esophagus: current practice and future applications. Ann Gastroenterol. 2012; 25:89–95.3. Pech O, Behrens A, May A, et al. Long-term results and risk factor analysis for recurrence after curative endoscopic therapy in 349 patients with high-grade intraepithelial neoplasia and mucosal adenocarcinoma in Barrett’s oesophagus. Gut. 2008; 57:1200–1206.
Article4. Chennat J, Konda VJ, Ross AS, et al. Complete Barrett’s eradication endoscopic mucosal resection: an effective treatment modality for high-grade dysplasia and intramucosal carcinoma. An American single-center experience. Am J Gastroenterol. 2009; 104:2684–2692.5. Pech O, May A, Manner H, et al. Long-term efficacy and safety of endoscopic resection for patients with mucosal adenocarcinoma of the esophagus. Gastroenterology. 2014; 146:652–660.
Article6. Ikeda K, Isomoto H, Oda H, et al. Endoscopic submucosal dissection of a minute intramucosal adenocarcinoma in Barrett’s esophagus. Dig Endosc. 2009; 21:34–36.
Article7. Osawa H, Yamamoto H. Present and future status of flexible spectral imaging color enhancement and blue laser imaging technology. Dig Endosc. 2014; 26 Suppl 1:105–115.
Article8. Osawa H, Yamamoto H, Miura Y, et al. Blue laser imaging provides excellent endoscopic images of upper gastrointestinal lesions. Video J Encycl GI Endosc. 2014; 1:607–610.
Article9. Falk GW, Rice TW, Goldblum JR, Richter JE. Jumbo biopsy forceps protocol still misses unsuspected cancer in Barrett’s esophagus with high-grade dysplasia. Gastrointest Endosc. 1999; 49:170–176.
Article10. Kim SL, Waring JP, Spechler SJ, et al. Diagnostic inconsistencies in Barrett’s esophagus. Department of veterans affairs gastroesophageal reflux study group. Gastroenterology. 1994; 107:945–949.11. Kara MA, Peters FP, Fockens P, ten Kate FJ, Bergman JJ. Endoscopic video-autofluorescence imaging followed by narrow band imaging for detecting early neoplasia in Barrett’s esophagus. Gastrointest Endosc. 2006; 64:176–185.
Article12. Sharma P, Bansal A, Mathur S, et al. The utility of a novel narrow band imaging endoscopy system in patients with Barrett’s esophagus. Gastrointest Endosc. 2006; 64:167–175.
Article13. Anagnostopoulos GK, Yao K, Kaye P, Hawkey CJ, Ragunath K. Novel endoscopic observation in Barrett’s oesophagus using high resolution magnification endoscopy and narrow band imaging. Aliment Pharmacol Ther. 2007; 26:501–507.
Article14. Curvers WL, Bohmer CJ, Mallant-Hent RC, et al. Mucosal morphology in Barrett’s esophagus: interobserver agreement and role of narrow band imaging. Endoscopy. 2008; 40:799–805.
Article15. Singh R, Anagnostopoulos GK, Yao K, et al. Narrow-band imaging with magnification in Barrett’s esophagus: validation of a simplified grading system of mucosal morphology patterns against histology. Endoscopy. 2008; 40:457–463.
Article16. Fukuda H, Miura Y, Hayashi Y, et al. Linked color imaging technology facilitates early detection of flat gastric cancers. Clin J Gastroenterol. 2015; 8:385–389.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Confocal Laser Endomicroscopy and Molecular Imaging in Barrett Esophagus and Stomach
- Diagnosis of Barrett's Esophagus
- Advanced endoscopic imaging for detection of Barrett’s esophagus
- Epidemiology of Barrett's Esophagus
- Recent Advances in Molecular Imaging of Premalignant Gastrointestinal Lesions and Future Application for Early Detection of Barrett Esophagus