Korean J Gastroenterol.
2017 Mar;69(3):191-195. 10.4166/kjg.2017.69.3.191.
Actinomycosis Involving Chronic Pancreatitis: A Case Report with Literature Review
- Affiliations
-
- 1Department of Internal Medicine, Kyungpook National University School of Medicine, Daegu, Korea. cmcho@knu.ac.kr
- 2Department of Radiology, Kyungpook National University School of Medicine, Daegu, Korea.
- 3Department of Pathology, Kyungpook National University School of Medicine, Daegu, Korea.
- KMID: 2383414
- DOI: http://doi.org/10.4166/kjg.2017.69.3.191
Abstract
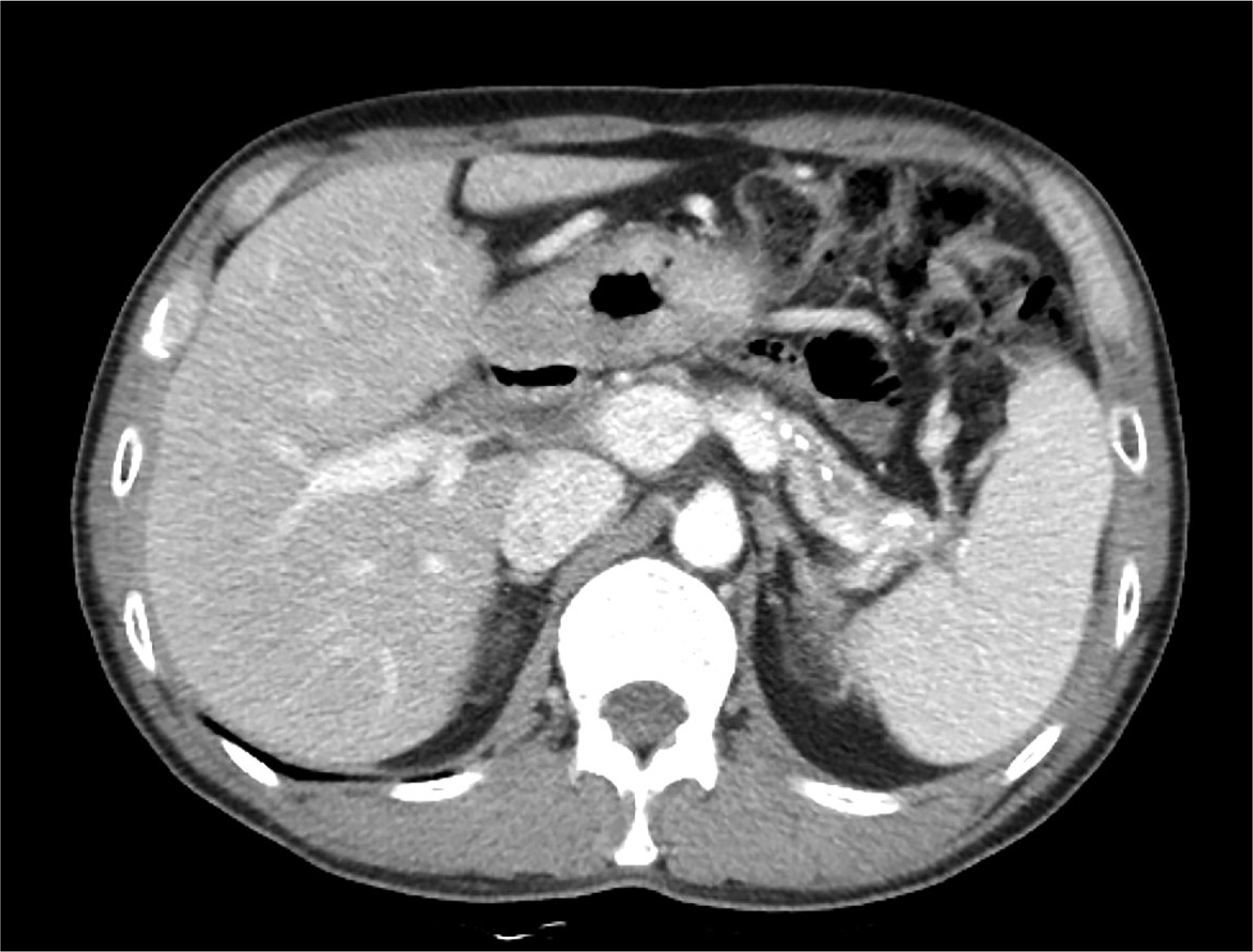
- Actinomycosis is a slowly progressive, chronic infectious disease. It is caused by the genus Actinomyces, which are gram-positive anaerobic bacteria. It presents as a mass-like lesion, composed of bacterial nidus and characteristic granulomatous inflammatory fibrosis. As such, it has frequently been mistaken for a malignancy. Surgical resection is a common procedure in these patients prior to a definite diagnosis. Although actinomycosis can occur in a variety of regions, including oral-cervicofacial, thoracic, and abdominopelvic cavities, the involvement of the pancreas is very rare. We report a case of a 44-year-old male with a symptomatic actinomycosis caused by a mass in the tail of the pancreas. The diagnosis was made using an endoscopic ultrasound-guided fine needle aspiration biopsy without surgical resection. After the treatment with antibiotics, the pancreatic mass was confirmed to be resolved on the follow-up computed tomography.
Keyword
MeSH Terms
Figure
Reference
-
References
1. Wong VK, Turmezei TD, Weston VC. Actinomycosis. BMJ. 2011; 343:d6099.
Article2. Garner JP, Macdonald M, Kumar PK. Abdominal actinomycosis. Int J Surg. 2007; 5:441–448.
Article3. Kim MC, Lee H, Park J, et al. A solitary pancreatic actinomycosis mimicking pancreatic cancer. Korean J Pancreas Biliary Tract. 2015; 20:130–135.
Article4. Lee JH, Lee KG, Oh YH, Park HK, Lee KS. Actinomycosis of the pancreas: a case report and review of the literature. Hepatogastroenterology. 2010; 57:358–361.5. Maestro S, Trujillo R, Geneux K, et al. Pancreatic actinomycosis presenting as pancreatic mass and diagnosed with endoscopic ultrasound fine needle aspiration (EUS-FNA). Endoscopy. 2013; 45(Suppl 2 UCTN):E276–E277.
Article6. Piper MH, Schaberg DR, Ross JM, Shartsis JM, Orzechowski RW. Endoscopic detection and therapy of colonic actinomycosis. Am J Gastroenterol. 1992; 87:1040–1042.7. Harsch IA, Benninger J, Niedobitek G, et al. Abdominal actinomycosis: complication of endoscopic stenting in chronic pancreatitis? Endoscopy. 2001; 33:1065–1069.
Article8. Kuesters S, Timme S, Keck T. Uncommon cause of an inflammatory pancreatic head tumor. Diagnosis: purulent actinomycosis and incidental T1-carcinoid of the pancreatic head. Gastroenterology. 2011; 141:e9–e10.9. Somsouk M, Shergill AK, Grenert JP, Harris H, Cello JP, Shah JN. Actinomycosis mimicking a pancreatic head neoplasm diagnosed by EUS-guided FNA. Gastrointest Endosc. 2008; 68:186–187.
Article10. Hsu JT, Lo HC, Jan YY, Chen HM. Actinomycosis mimicking recurrent carcinoma after whipple's operation. World J Gastroenterol. 2005; 11:1722–1724.
Article11. Harris LA, DeCosse JJ, Dannenberg A. Abdominal actinomycosis: evaluation by computed tomography. Am J Gastroenterol. 1989; 84:198–200.12. Lee IJ, Ha HK, Park CM, et al. Abdominopelvic actinomycosis involving the gastrointestinal tract: CT features. Radiology. 2001; 220:76–80.
Article13. Cintron JR, Del Pino A, Duarte B, Wood D. Abdominal actinomycosis. Dis Colon Rectum. 1996; 39:105–108.
Article14. Ferrari TC, Couto CA, Murta-Oliveira C, Conceição SA, Silva RG. Actinomycosis of the colon: a rare form of presentation. Scand J Gastroenterol. 2000; 35:108–109.15. Weese WC, Smith IM. A study of 57 cases of actinomycosis over a 36-year period. A diagnostic ‘failure’ with good prognosis after treatment. Arch Intern Med. 1975; 135:1562–1568.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Actinomycosis of the Vocal Cord
- Middle Ear Actinomycosis Involving Facial Nerve and Lateral Semicircular Canal
- A Case of Pelvic Actinomycosis Associated with Intrauterine Contraceptive Device
- Acute Pancreatitis Complicating Spontaneous Acute Exacerbation of Chronic Hepatitis B Virus Infection: Case Report and Review of the Literature
- MR Findings of Hepatic Actinomycosis: Case Report