Ann Rehabil Med.
2016 Oct;40(5):862-870. 10.5535/arm.2016.40.5.862.
Effects of Extracorporeal Shockwave Therapy in Chronic Stroke Patients With Knee Osteoarthritis: A Pilot Study
- Affiliations
-
- 1Department of Physical Medicine and Rehabilitation, Veterans Health Service Medical Center, Seoul, Korea. yangmary429@gmail.com
- KMID: 2382918
- DOI: http://doi.org/10.5535/arm.2016.40.5.862
Abstract
OBJECTIVE
To evaluate the effects of extracorporeal shockwave therapy (ESWT) on pain, function, and ultrasonographic features of chronic stroke patients with knee osteoarthritis (OA).
METHODS
A total of 18 chronic stroke patients (33 knee joints) with unilateral or bilateral knee OA (Kellgren-Lawrence grade ≥1) were enrolled in this study. The patients were randomly allocated to an experimental group receiving ESWT (n=9) or a control group receiving sham ESWT (n=9). For the ESWT group, patients received 1,000 pulses weekly for 3 weeks, totaling to an energy dose of 0.05 mJ/mm² on the proximal medial tibia of the affected knee. The assessments were performed before the treatment, immediately after the first treatment, and 1 week after the last treatment using the following: the visual analog scale (VAS) for pain; patient perception of the clinical severity of OA; the Korean version of Modified Barthel Index (ambulation and chair/bed transfer); the Functional Independence Measure scale (FIM; bed/chair/wheelchair transfer, toilet transfer, walking, and stairs); and ultrasonographic features (articular cartilage thickness, Doppler activity, and joint effusion height).
RESULTS
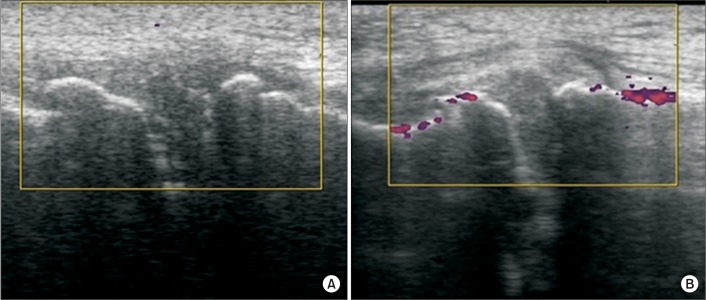
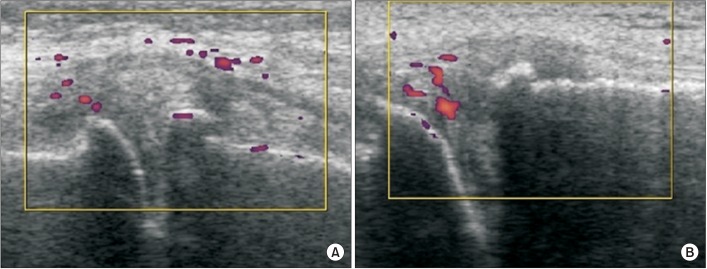
The experimental group showed a significant improvement in VAS score (4.50±1.87 to 2.71±1.38) and patient perception of the clinical severity of OA (1.87±0.83 to 2.75±0.46). The bed/chair/wheelchair transfer components of the FIM score also improved significantly (4.12±1.55 to 4.62±1.30). In terms of the ultrasonographic features, increased Doppler activity was observed in the medial knee in the experimental group immediately following ESWT.
CONCLUSION
It is suggested that ESWT may reduce pain and improve function in chronic stroke patients with OA, and may increase vascular activity at the target site.
MeSH Terms
Figure
Cited by 1 articles
-
Effect of Extracorporeal Shockwave Therapy Versus Intra-articular Injections of Hyaluronic Acid for the Treatment of Knee Osteoarthritis
June-Kyung Lee, Bong-Yeon Lee, Woo-Yong Shin, Min-Ji An, Kwang-Ik Jung, Seo-Ra Yoon
Ann Rehabil Med. 2017;41(5):828-835. doi: 10.5535/arm.2017.41.5.828.
Reference
-
1. Brundtland GH. Reducing risks to health, promoting healthy life. JAMA. 2002; 288:1974. PMID: 12387638.
Article2. Kim I, Kim HA, Seo YI, Song YW, Jeong JY, Kim DH. The prevalence of knee osteoarthritis in elderly community residents in Korea. J Korean Med Sci. 2010; 25:293–298. PMID: 20119586.
Article3. Doruk P. The impact of knee osteoarthritis on rehabilitation outcomes in hemiparetic stroke patients. J Back Musculoskelet Rehabil. 2013; 26:207–211. PMID: 23640323.
Article4. Zhang W, Moskowitz RW, Nuki G, Abramson S, Altman RD, Arden N, et al. OARSI recommendations for the management of hip and knee osteoarthritis. Part II: OARSI evidence-based, expert consensus guidelines. Osteoarthr Cartil. 2008; 16:137–162. PMID: 18279766.
Article5. Wang CJ. An overview of shock wave therapy in musculoskeletal disorders. Chang Gung Med J. 2003; 26:220–232. PMID: 12846521.6. Frisbie DD, Kawcak CE, McIlwraith CW. Evaluation of the effect of extracorporeal shock wave treatment on experimentally induced osteoarthritis in middle carpal joints of horses. Am J Vet Res. 2009; 70:449–454. PMID: 19335099.
Article7. Revenaugh MS. Extracorporeal shock wave therapy for treatment of osteoarthritis in the horse: clinical applications. Vet Clin North Am Equine Pract. 2005; 21:609–625. PMID: 16297724.
Article8. Mueller M, Bockstahler B, Skalicky M, Mlacnik E, Lorinson D. Effects of radial shockwave therapy on the limb function of dogs with hip osteoarthritis. Vet Rec. 2007; 160:762–765. PMID: 17545646.
Article9. Dahlberg J, Fitch G, Evans RB, McClure SR, Conzemius M. The evaluation of extracorporeal shockwave therapy in naturally occurring osteoarthritis of the stifle joint in dogs. Vet Comp Orthop Traumatol. 2005; 18:147–152. PMID: 16594445.
Article10. Wang CJ, Sun YC, Siu KK, Wu CT. Extracorporeal shockwave therapy shows site-specific effects in osteoarthritis of the knee in rats. J Surg Res. 2013; 183:612–619. PMID: 23472862.
Article11. Wang CJ, Sun YC, Wong T, Hsu SL, Chou WY, Chang HW. Extracorporeal shockwave therapy shows time-dependent chondroprotective effects in osteoarthritis of the knee in rats. J Surg Res. 2012; 178:196–205. PMID: 22608545.
Article12. Zhao Z, Ji H, Jing R, Liu C, Wang M, Zhai L, et al. Extracorporeal shock-wave therapy reduces progression of knee osteoarthritis in rabbits by reducing nitric oxide level and chondrocyte apoptosis. Arch Orthop Trauma Surg. 2012; 132:1547–1553. PMID: 22825641.
Article13. Carlsson AM. Assessment of chronic pain. I: Aspects of the reliability and validity of the visual analogue scale. Pain. 1983; 16:87–101. PMID: 6602967.
Article14. Loyola-Sanchez A, Richardson J, Beattie KA, Otero-Fuentes C, Adachi JD, MacIntyre NJ. Effect of low-intensity pulsed ultrasound on the cartilage repair in people with mild to moderate knee osteoarthritis: a double-blinded, randomized, placebo-controlled pilot study. Arch Phys Med Rehabil. 2012; 93:35–42. PMID: 22200383.15. Jung HY, Park BK, Shin HS, Kang YK, Pyun SB, Paik NJ, et al. Development of the Korean Version of Modified Barthel Index (K-MBI): multi-center study for subjects with stroke. J Korean Acad Rehabil Med. 2007; 31:283–297.16. Hamilton BB, Laughlin JA, Fiedler RC, Granger CV. Interrater reliability of the 7-level functional independence measure (FIM). Scand J Rehabil Med. 1994; 26:115–119. PMID: 7801060.17. Riecke BF, Christensen R, Torp-Pedersen S, Boesen M, Gudbergsen H, Bliddal H. An ultrasound score for knee osteoarthritis: a cross-sectional validation study. Osteoarthr Cartil. 2014; 22:1675–1691. PMID: 25278077.
Article18. Wang CJ. Extracorporeal shockwave therapy in musculoskeletal disorders. J Orthop Surg Res. 2012; 7:11. PMID: 22433113.
Article19. Wang CJ, Hsu SL, Weng LH, Sun YC, Wang FS. Extracorporeal shockwave therapy shows a number of treatment related chondroprotective effect in osteoarthritis of the knee in rats. BMC Musculoskelet Disord. 2013; 14:44. PMID: 23356403.
Article20. Zhao Z, Jing R, Shi Z, Zhao B, Ai Q, Xing G. Efficacy of extracorporeal shockwave therapy for knee osteoarthritis: a randomized controlled trial. J Surg Res. 2013; 185:661–666. PMID: 23953895.
Article21. Kim JH, Kim JY, Choi CM, Lee JK, Kee HS, Jung KI, et al. The dose-related effects of extracorporeal shock wave therapy for knee osteoarthritis. Ann Rehabil Med. 2015; 39:616–623. PMID: 26361599.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Efficacy of Extracorporeal Shock Wave Therapy for Knee Osteoarthritis
- Effect of Extracorporeal Shockwave Therapy Versus Intra-articular Injections of Hyaluronic Acid for the Treatment of Knee Osteoarthritis
- Prevalence of Knee Osteoarthritis and Health-Related Quality of Life in Stroke Patients over 60 Years Old: A Cross-Sectional Study Using Korean National Health and Nutrition Examination Survey V
- Focused Extracorporeal Shockwave Therapy for Postsurgical Achilles Tendon Tightness: A Case Report
- The Clinical Results of Radial and Focused Extracorporeal Shockwave Therapy on Periscapular Myofascial Pain Syndrome