Ann Rehabil Med.
2016 Oct;40(5):851-861. 10.5535/arm.2016.40.5.851.
Analysis of Pulmonary Function Test in Korean Patients With Duchenne Muscular Dystrophy: Comparison of Foreign and Korean Reference Data
- Affiliations
-
- 1Department of Rehabilitation Medicine, Pusan National University Yangsan Hospital, Pusan National University School of Medicine, Yangsan, Korea.
- 2Department of Rehabilitation Medicine, Pusan National University Hospital, Pusan National University School of Medicine, Busan, Korea. yi0314@gmail.com
- 3Biomedical Research Institute, Pusan National University Hospital, Busan, Korea.
- KMID: 2382917
- DOI: http://doi.org/10.5535/arm.2016.40.5.851
Abstract
OBJECTIVE
To determine the abnormal pulmonary function value in Korean Duchenne muscular dystrophy (DMD) patients, we performed a comparative analysis of the patients' pulmonary function value expressed as % of the overseas reference data and Korean healthy children and adolescent reference data.
METHODS
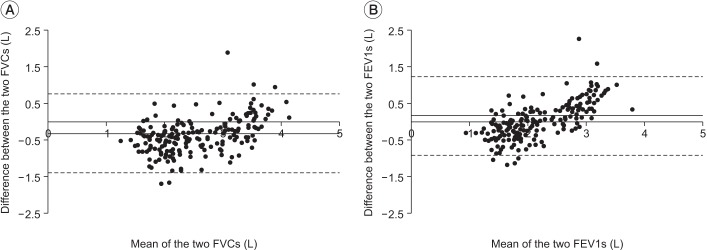
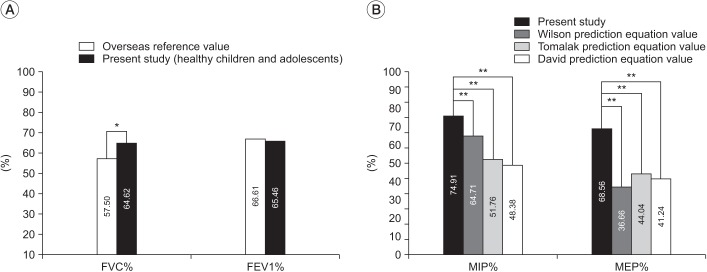
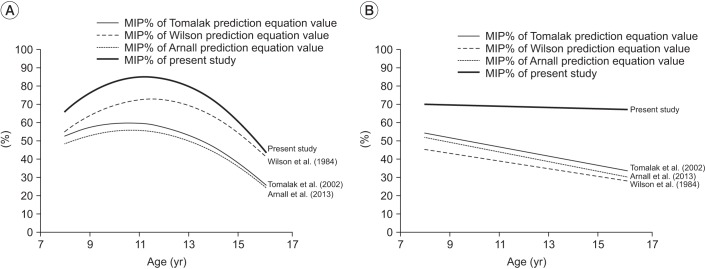
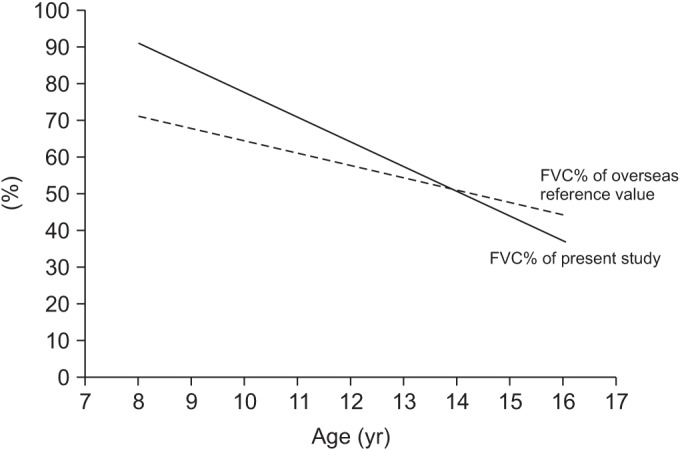
We performed pulmonary function test (PFT) in a total of 27 DMD patients. We compared the patients' FVC% and FEV1% of the overseas reference data with those of the Korean children and adolescent reference data. Also, we compared the patients' MIP% and MEP% of the prediction equation data with those of the Korean children and adolescent reference data.
RESULTS
Age of the subjects ranged from 8 to 16 years (12.03±2.27 years). The mean maximal expiratory pressure (MEP), maximal inspiratory pressure (MIP), vital capacity (VC), forced vital capacity (FVC), forced expiratory volume in 1 second (FEV1), and peak cough flow (PCF) were 36.93±9.5 cmHâ‚‚O, 45.79±17.46 cmHâ‚‚O, 1.4±0.43 L, 1.45±0.45 L, 1.40±0.41 L, and 206.25±61.21 L/min, respectively. The MIP%, MEP%, and FVC% of the Korean children and adolescent reference data showed statistically significant higher values than those of the prediction equation data.
CONCLUSION
We observed a clear numeric difference between Korean DMD patients' pulmonary function value expressed as % of the overseas data and inland data. To perform a precise assessment of respiratory function and to determine appropriate respiratory therapy, pulmonary function values of Korean DMD patients should be interpreted taking into account the inland normal pulmonary function test data.
MeSH Terms
Figure
Reference
-
1. Walton JN, Gardner-Medwin D. Progressive muscular dystrophy and the myotonic disorders. In : Walton JN, editor. Disorders of voluntary muscle. 3rd ed. London: Churchill Livingston;1974. p. 561–613.2. Gardner-Medwin D. Clinical features and classification of the muscular dystrophies. Br Med Bull. 1980; 36:109–115. PMID: 7020835.
Article3. Hapke EJ, Meek JC, Jacobs J. Pulmonary function in progressive muscular dystrophy. Chest. 1972; 61:41–47. PMID: 5049500.
Article4. Inkley SR, Oldenburg FC, Vignos PJ Jr. Pulmonary function in Duchenne muscular dystrophy related to stage of disease. Am J Med. 1974; 56:297–306. PMID: 4813648.
Article5. Rideau Y. Prognosis of progressive muscular dystrophy in children. Analysis of early and exact criteria. Union Med Can. 1977; 106:874–882. PMID: 883053.6. Rideau Y, Jankowski LW, Grellet J. Respiratory function in the muscular dystrophies. Muscle Nerve. 1981; 4:155–164. PMID: 7207506.
Article7. Nagai T. Prognostic evaluation of congestive heart failure in patients with Duchenne muscular dystrophy: retrospective study using non-invasive cardiac function tests. Jpn Circ J. 1989; 53:406–415. PMID: 2769928.
Article8. McDonald CM, Abresch RT, Carter GT, Fowler WM Jr, Johnson ER, Kilmer DD, et al. Profiles of neuromuscular diseases. Duchenne muscular dystrophy. Am J Phys Med Rehabil. 1995; 74(5 Suppl):S70–S92. PMID: 7576424.9. Black LF, Hyatt RE. Maximal respiratory pressures: normal values and relationship to age and sex. Am Rev Respir Dis. 1969; 99:696–702. PMID: 5772056.10. Gayraud J, Ramonatxo M, Rivier F, Humberclaude V, Petrof B, Matecki S. Ventilatory parameters and maximal respiratory pressure changes with age in Duchenne muscular dystrophy patients. Pediatr Pulmonol. 2010; 45:552–559. PMID: 20503279.
Article11. Arora NS, Rochester DF. Respiratory muscle strength and maximal voluntary ventilation in undernourished patients. Am Rev Respir Dis. 1982; 126:5–8. PMID: 7091909.12. Celli BR. Clinical and physiologic evaluation of respiratory muscle function. Clin Chest Med. 1989; 10:199–214. PMID: 2661118.
Article13. Enright PL, Kronmal RA, Manolio TA, Schenker MB, Hyatt RE. Respiratory muscle strength in the elderly: correlates and reference values. Cardiovascular Health Study Research Group. Am J Respir Crit Care Med. 1994; 149(2 Pt 1):430–438. PMID: 8306041.
Article14. Hautmann H, Hefele S, Schotten K, Huber RM. Maximal inspiratory mouth pressures (PIMAX) in healthy subjects: what is the lower limit of normal? Respir Med. 2000; 94:689–693. PMID: 10926341.15. Arnall DA, Nelson AG, Owens B, CebriaiIranzo MA, Sokell GA, Kanuho V, et al. Maximal respiratory pressure reference values for Navajo children ages 6-14. Pediatr Pulmonol. 2013; 48:804–808. PMID: 23661611.
Article16. Wilson SH, Cooke NT, Edwards RH, Spiro SG. Predicted normal values for maximal respiratory pressures in caucasian adults and children. Thorax. 1984; 39:535–538. PMID: 6463933.
Article17. Tomalak W, Pogorzelski A, Prusak J. Normal values for maximal static inspiratory and expiratory pressures in healthy children. Pediatr Pulmonol. 2002; 34:42–46. PMID: 12112796.
Article18. Yoon KA, Lim HS, Koh YY, Kim H. Normal predicted values of pulmonary function test in Korean school-aged children. J Korean Pediatr Soc. 1993; 36:25–37.19. Hahn A, Bach JR, Delaubier A, Renardel-Irani A, Guillou C, Rideau Y. Clinical implications of maximal respiratory pressure determinations for individuals with Duchenne muscular dystrophy. Arch Phys Med Rehabil. 1997; 78:1–6. PMID: 9014949.
Article20. Bye PT, Ellis ER, Issa FG, Donnelly PM, Sullivan CE. Respiratory failure and sleep in neuromuscular disease. Thorax. 1990; 45:241–247. PMID: 2113317.
Article21. Griggs RC, Donohoe KM, Utell MJ, Goldblatt D, Moxley RT 3rd. Evaluation of pulmonary function in neuromuscular disease. Arch Neurol. 1981; 38:9–12. PMID: 7458733.
Article22. Kang SW, Kang YS, Sohn HS, Park JH, Moon JH. Respiratory muscle strength and cough capacity in patients with Duchenne muscular dystrophy. Yonsei Med J. 2006; 47:184–190. PMID: 16642546.
Article23. Lissoni A. Assessment of the respiratory function in individuals with Duchenne muscular dystrophy. Eura Medicophys. 2001; 37:71–81.24. Bushby K, Finkel R, Birnkrant DJ, Case LE, Clemens PR, Cripe L, et al. Diagnosis and management of Duchenne muscular dystrophy. Part 2: implementation of multidisciplinary care. Lancet Neurol. 2010; 9:177–189. PMID: 19945914.
Article25. Phillips MF, Quinlivan RC, Edwards RH, Calverley PM. Changes in spirometry over time as a prognostic marker in patients with Duchenne muscular dystrophy. Am J Respir Crit Care Med. 2001; 164:2191–2194. PMID: 11751186.
Article26. Gomez-Merino E, Bach JR. Duchenne muscular dystrophy: prolongation of life by noninvasive ventilation and mechanically assisted coughing. Am J Phys Med Rehabil. 2002; 81:411–415. PMID: 12023596.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Clinical Implications of Pulmonary Function Test and Maximum Static Pressure in Duchenne Muscular Dystrophy
- A clinical study on Duchenne muscular dystrophy
- Duchenne Muscular Dystrophy Complicated With Dilated Cardiomyopathy and Cerebral Infarction
- A Clinical Study on Duchenne Muscular Dystrophy in Childhood
- Duchenne Type Muscular Dystrophy: Report of 8 Cases