Ann Dermatol.
2016 Oct;28(5):632-636. 10.5021/ad.2016.28.5.632.
Case of Pleomorphic Dermal Sarcoma of the Eyelid Treated with Micrographic Surgery and Secondary Intention Healing
- Affiliations
-
- 1Department of Dermatology, Kangbuk Samsung Hospital, Sungkyunkwan University School of Medicine, Seoul, Korea. susini@naver.com
- 2Department of Pathology, Kangbuk Samsung Hospital, Sungkyunkwan University School of Medicine, Seoul, Korea.
- 3Department of Dermatology, Seoul St. Mary's Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea.
- KMID: 2382890
- DOI: http://doi.org/10.5021/ad.2016.28.5.632
Abstract
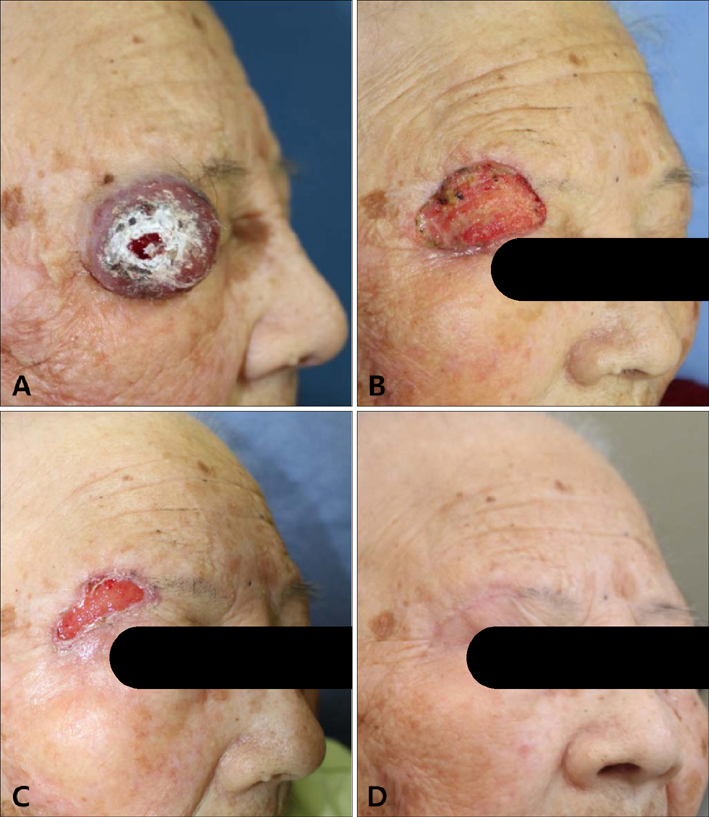
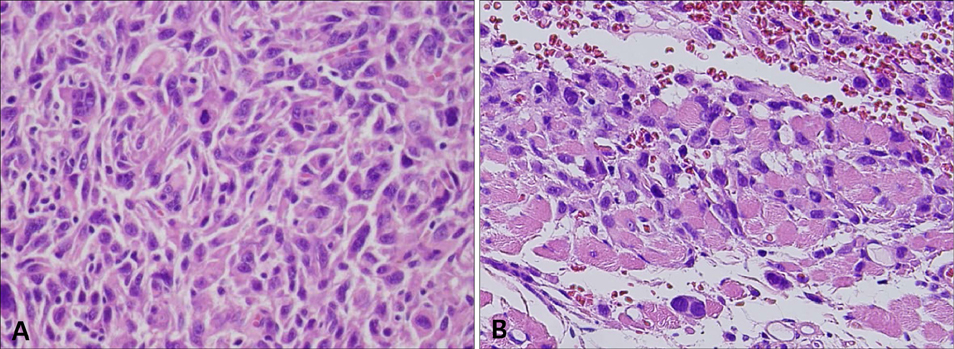
- Pleomorphic dermal sarcoma (PDS) is a rare mesenchymal neoplasm sharing histopathological features with atypical fibroxanthoma (AFX), but has additional features of deep invasion of the superficial subcutis, tumor necrosis and vascular/perineural invasion. It is not well documented in the literature because of its rarity, and its clinical course has been debated due to the lack of homogenous criteria. We describe here the case of a 91-year-old female with a 6-month history of a solitary, asymptomatic, well-defined, 3.4-cm-sized, reddish, hard, protruding mass on the lateral aspect of the right upper eyelid. On the basis of initial punch biopsy results, storiform cellular infiltrate of pleomorphic spindle and polygonal cells with frequent atypical mitoses, the lesion was identified as AFX. Following the initial biopsy, micrographic surgery was performed and a tumor-free margin was confirmed. Considering the conservation of the periocular function and the advanced age of the patient, we planned secondary intention healing rather than primary suturing. After surgery, skeletal muscle infiltration was found and the diagnosis was revised to PDS by a pathologist based on the currently accepted criteria for PDS. There has been no evidence of recurrence or periocular functional defects during a 2-year follow-up without adjuvant therapy. Although the PDS is highly malignant, complete excision under micrographic surgery can prevent recurrence without adjuvant therapy. Also, the secondary intention healing is an effective method for closure of large defects on the face.
Keyword
MeSH Terms
Figure
Reference
-
1. Miller K, Goodlad JR, Brenn T. Pleomorphic dermal sarcoma: adverse histologic features predict aggressive behavior and allow distinction from atypical fibroxanthoma. Am J Surg Pathol. 2012; 36:1317–1326.2. McCalmont TH. Correction and clarification regarding AFX and pleomorphic dermal sarcoma. J Cutan Pathol. 2012; 39:8.
Article3. Tardío JC, Pinedo F, Aramburu JA, Suárez-Massa D, Pampín A, Requena L, et al. Pleomorphic dermal sarcoma: a more aggressive neoplasm than previously estimated. J Cutan Pathol. 2016; 43:101–112.
Article4. Ang GC, Roenigk RK, Otley CC, Kim Phillips P, Weaver AL. More than 2 decades of treating atypical fibroxanthoma at mayo clinic: what have we learned from 91 patients? Dermatol Surg. 2009; 35:765–772.5. Beer TW, Drury P, Heenan PJ. Atypical fibroxanthoma: a histological and immunohistochemical review of 171 cases. Am J Dermatopathol. 2010; 32:533–540.
Article6. Calonje JE, Brenn T, Komminoth P. Atypical fibroxanthoma. 4th ed. Lyon: IARC Press;2013.7. Fletcher CD. The evolving classification of soft tissue tumours-an update based on the new 2013 WHO classification. Histopathology. 2014; 64:2–11.
Article8. McCalmont TH. AFX: what we now know. J Cutan Pathol. 2011; 38:853–856.
Article9. Griewank KG, Schilling B, Murali R, Bielefeld N, Schwamborn M, Sucker A, et al. TERT promoter mutations are frequent in atypical fibroxanthomas and pleomorphic dermal sarcomas. Mod Pathol. 2014; 27:502–508.
Article10. Luzar B, Calonje E. Morphological and immunohistochemical characteristics of atypical fibroxanthoma with a special emphasis on potential diagnostic pitfalls: a review. J Cutan Pathol. 2010; 37:301–309.
Article11. Perez-Montiel MD, Plaza JA, Dominguez-Malagon H, Suster S. Differential expression of smooth muscle myosin, smooth muscle actin, h-caldesmon, and calponin in the diagnosis of myofibroblastic and smooth muscle lesions of skin and soft tissue. Am J Dermatopathol. 2006; 28:105–111.
Article12. Harding-Jackson N, Sangueza M, Mackinnon A, Suster S, Plaza JA. Spindle cell atypical fibroxanthoma: myofibroblastic differentiation represents a diagnostic pitfall in this variant of AFX. Am J Dermatopathol. 2015; 37:509–514. quiz 515-516.13. Kraft S, Fletcher CD. Atypical intradermal smooth muscle neoplasms: clinicopathologic analysis of 84 cases and a reappraisal of cutaneous "leiomyosarcoma". Am J Surg Pathol. 2011; 35:599–607.14. Mansoor A, White CR Jr. Myxofibrosarcoma presenting in the skin: clinicopathological features and differential diagnosis with cutaneous myxoid neoplasms. Am J Dermatopathol. 2003; 25:281–286.
Article15. Merck C, Angervall L, Kindblom LG, Odén A. Myxofibrosarcoma. A malignant soft tissue tumor of fibroblastichistiocytic origin. A clinicopathologic and prognostic study of 110 cases using multivariate analysis. Acta Pathol Microbiol Immunol Scand Suppl. 1983; 282:1–40.16. Zitelli JA. Wound healing by secondary intention. A cosmetic appraisal. J Am Acad Dermatol. 1983; 9:407–415.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Pleomorphic Dermal Sarcoma Showing Characteristics of Myxoinflammatory Fibroblastic Sarcoma
- Secondary Intention Healing of Large Mohs Defects of the Forehead and Temple
- A Case of Pleomorphic Dermal Sarcoma and Literature Review according to World Health Organization Reclassification Guideline
- A Case of Pleomorphic Dermal Sarcoma of the Forearm Treated with Surgical Excision and Postoperative Radiation Therapy
- Pleomorphic Dermal Sarcoma on Burn Scar: A Case Report