J Korean Neurosurg Soc.
2017 May;60(3):375-379. 10.3340/jkns.2014.0808.026.
Endoscopic Treatment of an Adult with Tegmental Astrocytoma Accompanied by Cerebrospinal Fluid Dissemination
- Affiliations
-
- 1Neurosurgical Department, Peking University First Hospital, Beijing, China.
- 2Beijing Neurosurgical Institute, Beijing, China. zyz2004520@yeah.net
- KMID: 2382775
- DOI: http://doi.org/10.3340/jkns.2014.0808.026
Abstract
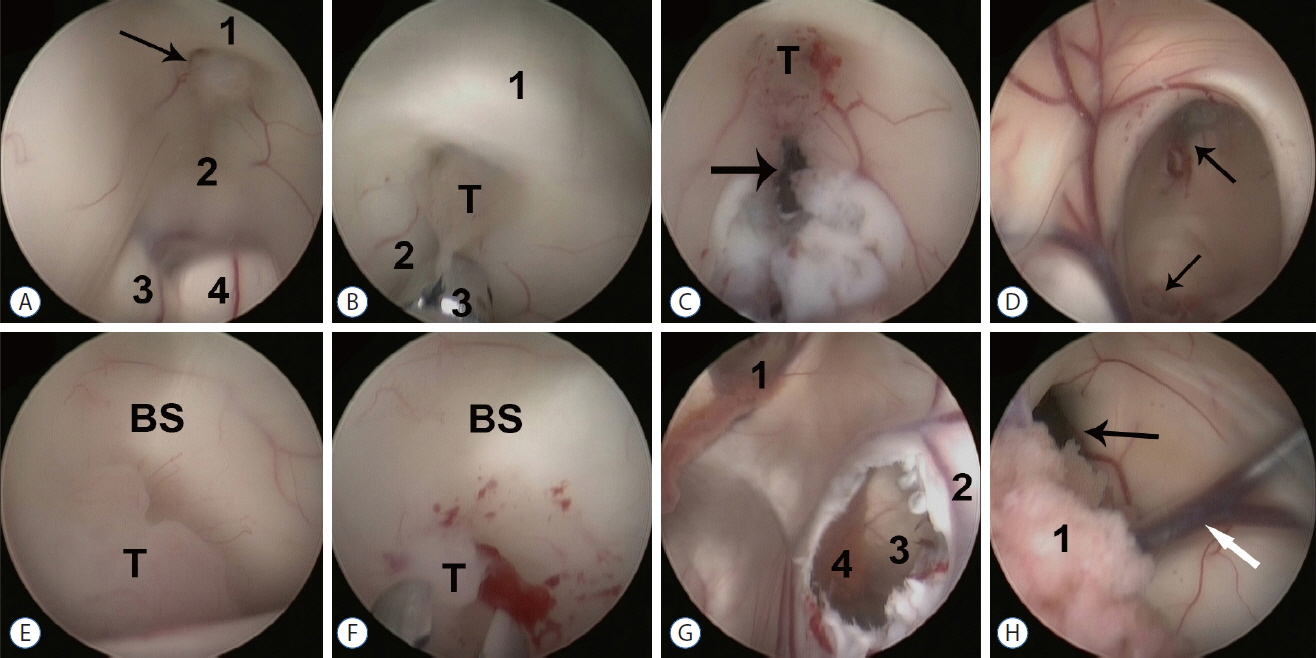
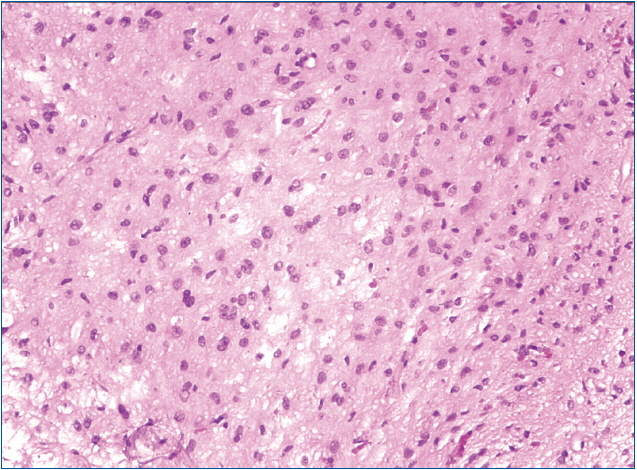
- Midbrain gliomas are relatively rare neoplasms with a generally benign prognosis, with dissemination or metastasis not previously reported. We describe here a woman, in whom magnetic resonance imaging scans showed hydrocephalus and a tegmental lesion in the upper aqueduct. Endoscopic third ventriculostomy and biopsy were performed; during surgery, a second small lesion was observed in the infundibular recess. Histologically, the two lesions had the characteristics of low grade astrocytoma, suggesting that the midbrain astrocytoma may have been disseminated via the cerebral spinal fluid to the infundibular recess. Postoperatively this patient received radiotherapy for nearly one month. Although patients with these tumors are not usually administered adjunctive therapy, radiation and, combined modality therapy, including surgery, radiotherapy, and chemotherapy, may be beneficial in patients with midbrain gliomas with dissemination.
Keyword
MeSH Terms
Figure
Reference
-
References
1. Andrychowski J, Taraszewska A, Czernicki Z, Jurkiewicz J, Netczuk T, Dabrowski P. Ten years observation and treatment of multifocal pilocytic astrocytoma. Folia Neuropathol. 47:362–370. 2009.2. Buschmann U, Gers B, Hildebrandt G. Pilocytic astrocytomas with leptomeningeal dissemination: biological behavior, clinical course, and therapeutical options. Childs Nerv Syst. 19:298–304. 2003.
Article3. Domínguez-Páez M, Puch-Ramírez M, Rodríguez-Barceló S, Medina-Imbroda JM, Romero-Moreno L, Ibáñez-Botella G, et al. Neuroendoscopic biopsy. Experience in 31 patients and literature review. Neurocirugia (Astur). 22:419–427. discussion 428. 2011.4. Faria AV, Azevedo GC, Zanardi VA, Ghizoni E, Queiroz LS. Dissemination patterns of pilocytic astrocytoma. Clin Neurol Neurosurg. 108:568–572. 2006.
Article5. Figueiredo EG, Matushita H, Machado AG, Plese JP, Rosemberg S, Marino R Jr. Leptomeningeal dissemination of pilocytic astrocytoma at diagnosis in childhood: two cases report. Arq Neuropsiquiatr. 61(3B):842–847. 2003.
Article6. Gajjar A, Bhargava R, Jenkins JJ, Heideman R, Sanford RA, Langston JW, et al. Low-grade astrocytoma with neuraxis dissemination at diagnosis. J Neurosurg. 83:67–71. 1995.
Article7. Hamilton MG, Lauryssen C, Hagen N. Focal midbrain glioma: long term survival in a cohort of 16 patients and the implications for management. Can J Neurol Sci. 23:204–207. 1996.
Article8. Jamjoom AB, Jamjoom ZA, al-Rayess M. Intraventricular and leptomeningeal dissemination of a pilocytic cerebellar astrocytoma in a child with a ventriculoperitoneal shunt: case report. Br J Neurosurg. 12:56–58. 1998.
Article9. Lázaro BC, Landeiro JA. Tectal plate tumors. Arq Neuropsiquiatr. 64(2B):432–436. 2006.
Article10. Li KW, Roonprapunt C, Lawson HC, Abbott IR, Wisoff J, Epstein F, et al. Endoscopic third ventriculostomy for hydrocephalus associated with tectal gliomas. Neurosurg Focus. 18(6A):E2. 2005.
Article11. Moon JH, Jung TY, Jung S, Jang WY. Leptomeningeal dissemination of a low-grade brainstem glioma without local recurrence. J Korean Neurosurg Soc. 51:109–112. 2012.
Article12. Oka K, Kin Y, Go Y, Ueno Y, Hirakawa K, Tomonaga M, et al. Neuroendoscopic approach to tectal tumors: a consecutive series. J Neurosurg. 91:964–970. 1999.
Article13. Oppido PA, Fiorindi A, Benvenuti L, Cattani F, Cipri S, Gangemi M, et al. Neuroendoscopic biopsy of ventricular tumors: a multicentric experience. Neurosurg Focus. 30:E2. 2011.
Article14. Pollack IF, Hurtt M, Pang D, Albright AL. Dissemination of low grade intracranial astrocytomas in children. Cancer. 73:2869–2878. 1994.
Article15. Redhu R, Nadkarni TD. Multicompartmental cerebrospinal fluid dissemination of cerebellar pilocytic astrocytoma at presentation. J Clin Neurosci. 18:1412–1414. 2011.
Article16. Sakai K, Miyahara T, Tsutsumi K, Kaneko T, Fukushima M, Tanaka Y, et al. Spontaneous regression of multicentric pilocytic astrocytoma with CSF dissemination in an adult. Brain Tumor Pathol. 28:151–156. 2011.
Article17. Salvati M, Oppido PA, Artizzu S, Fiorenza F, Puzzilli F, Orlando ER. Multicentric gliomas. Report of seven cases. Tumori. 77:518–522. 1991.
Article18. Selvapandian S, Rajshekhar V, Chandy MJ. Brainstem glioma: comparative study of clinico-radiological presentation, pathology and outcome in children and adults. Acta Neurochir (Wien). 141:721–726. discussion 726–727. 1999.
Article19. Tirakotai W, Hellwig D, Bertalanffy H, Riegel T. The role of neuroendoscopy in the management of solid or solid-cystic intra- and periventricular tumours. Childs Nerv Syst. 23:653–658. 2007.
Article20. Uro-Coste E, Ssi-Yan-Kai G, Guilbeau-Frugier C, Boetto S, Bertozzi AI, Sevely A, et al. Desmoplastic infantile astrocytoma with benign histological phenotype and multiple intracranial localizations at presentation. J Neurooncol. 98:143–149. 2010.
Article21. Wang C, Zhang J, Liu A, Sun B, Zhao Y. Surgical treatment of primary midbrain gliomas. Surg Neurol. 53:41–51. 2000.
Article22. Wellons JC 3rd, Tubbs RS, Banks JT, Grabb B, Blount JP, Oakes WJ, et al. Long-term control of hydrocephalus via endoscopic third ventriculostomy in children with tectal plate gliomas. Neurosurgery. 51:63–67. discussion 67–68. 2002.
Article23. Yeh DD, Warnick RE, Ernst RJ. Management strategy for adult patients with dorsal midbrain gliomas. Neurosurgery. 50:735–738. discussion 738–740. 2002.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Traumatic Cerebrospinal Fluid Rhinorrhea: Successful Closure under the Surgical Microscope
- Endoscopic treatment of iatrogenic cerebrospinal fluid rhinorrhea
- Endoscopic Management of Cerebrospinal Fluid Rhinorrhea
- Management of Cerebrospinal Fluid Rhinorrhea
- Surgical Repair of Cerebrospinal Fluid Rhinorrhea with Mucoperichondrial Free Graft