Intest Res.
2017 Jul;15(3):338-344. 10.5217/ir.2017.15.3.338.
Impact of inflammatory bowel disease on daily life: an online survey by the Korean Association for the Study of Intestinal Diseases
- Affiliations
-
- 1Department of Internal Medicine, Seoul National University Healthcare System Gangnam Center, Seoul, Korea.
- 2Department of Internal Medicine, Ewha Womans University School of Medicine, Seoul, Korea. jassa@ewha.ac.kr
- 3Department of Internal Medicine, St. Vincent's Hospital, The Catholic University of Korea College of Medicine, Suwon, Korea.
- 4Department of Internal Medicine, Yonsei University College of Medicine, Seoul, Korea.
- 5Department of Internal Medicine, Haeundae Paik Hospital, Inje University College of Medicine, Busan, Korea.
- 6Department of Internal Medicine, Chung-Ang University College of Medicine, Seoul, Korea.
- 7Department of Internal Medicine, Soonchunhyang University College of Medicine, Seoul, Korea.
- 8Department of Internal Medicine, Kosin University College of Medicine, Busan, Korea.
- 9Department of Internal Medicine, Jeju National University School of Medicine, Jeju, Korea.
- 10Department of Internal Medicine, University of Ulsan College of Medicine, Seoul, Korea.
- KMID: 2382377
- DOI: http://doi.org/10.5217/ir.2017.15.3.338
Abstract
- BACKGROUND/AIMS
Inflammatory bowel disease (IBD) is a chronic disabling gastrointestinal disorder that diminishes the quality of life of the affected individuals. Limited data are available regarding the impact of IBD on the daily life of Koreans.
METHODS
Self-administered, computer-aided, internet-based questionnaires were distributed to members of a Korean patient organization for IBD from March to April 2013, by the Korean Association for the Study of Intestinal Diseases.
RESULTS
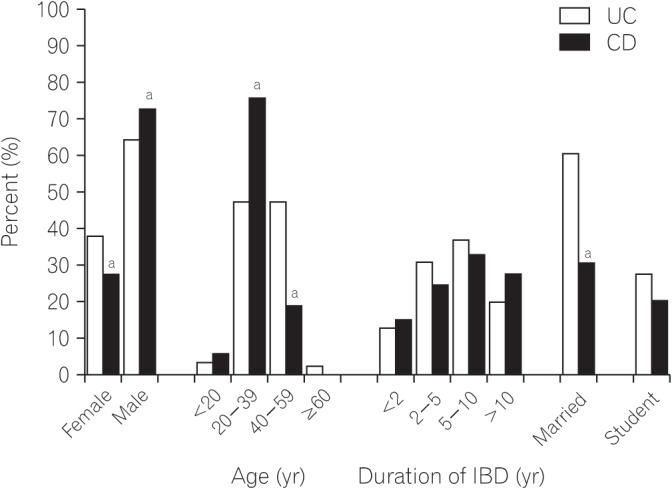
A total of 599 patients with IBD (387 with Crohn's disease [CD] and 212 with ulcerative colitis [UC]) were enrolled. The majority of patients (81%) expressed feelings of fatigue, weakness, and being worn out in their daily lives during times of flare; this percentage was reduced to 61% during remission. Respondents were absent from work or school for an average period of 18 days because of illness, within the first 6 months; the majority of respondents (64%) felt stressed about their absence. Forty-six percent of the respondents reported having received unfair comments at work, or having suffered discrimination. Forty-seven percent of the respondents felt that IBD had negatively affected their income and earnings. Compared with patients with UC, those with CD reported a more frequent negative impact of IBD on work, or more economic burden. More than half of the respondents (61%) reported that IBD had prevented them from making or keeping friends.
CONCLUSIONS
IBD significantly impacts daily life, including work, education, and social relationships. Treatment that addresses the full spectrum of life of a patient would be more effective.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
IBD2020 global forum: results of an international patient survey on quality of care
Peter Irving, Johan Burisch, Richard Driscoll, Mats Olsson, John R Fullarton, Barry S Rodgers-Gray, Simon PL Travis
Intest Res. 2018;16(4):537-545. doi: 10.5217/ir.2018.00041.
Reference
-
1. Yang SK, Yun S, Kim JH, et al. Epidemiology of inflammatory bowel disease in the Songpa-Kangdong district, Seoul, Korea, 1986-2005: a KASID study. Inflamm Bowel Dis. 2008; 14:542–549. PMID: 17941073.
Article2. Lee JW, Im JP, Cheon JH, Kim YS, Kim JS, Han DS. Inflammatory bowel disease cohort studies in Korea: present and future. Intest Res. 2015; 13:213–218. PMID: 26130995.
Article3. Choi JH, Kim ES, Cho KB, et al. Old age at diagnosis is associated with favorable outcomes in Korean patients with inflammatory bowel disease. Intest Res. 2015; 13:60–67. PMID: 25691844.
Article4. Sewell JL, Velayos FS. Systematic review: the role of race and socioeconomic factors on IBD healthcare delivery and effectiveness. Inflamm Bowel Dis. 2013; 19:627–643. PMID: 22623078.5. Peyrin-Biroulet L, Cieza A, Sandborn WJ, et al. Development of the first disability index for inflammatory bowel disease based on the international classification of functioning, disability and health. Gut. 2012; 61:241–247. PMID: 21646246.
Article6. Peyrin-Biroulet L, Billioud V, D'Haens G, et al. Development of the Paris definition of early Crohn's disease for disease-modification trials: results of an international expert opinion process. Am J Gastroenterol. 2012; 107:1770–1776. PMID: 23211844.
Article7. Hu PJ. Inflammatory bowel disease in Asia: the challenges and opportunities. Intest Res. 2015; 13:188–190. PMID: 26130991.
Article8. Lönnfors S, Vermeire S, Greco M, Hommes D, Bell C, Avedano L. IBD and health-related quality of life: discovering the true impact. J Crohns Colitis. 2014; 8:1281–1286. PMID: 24662394.9. Romberg-Camps MJ, Bol Y, Dagnelie PC, et al. Fatigue and health-related quality of life in inflammatory bowel disease: results from a population-based study in the Netherlands: the IBD-South Limburg cohort. Inflamm Bowel Dis. 2010; 16:2137–2147. PMID: 20848468.
Article10. Haapamäki J, Roine RP, Sintonen H, Turunen U, Färkkilä MA, Arkkila PE. Health-related quality of life in inflammatory bowel disease measured with the generic 15D instrument. Qual Life Res. 2010; 19:919–928. PMID: 20361263.
Article11. Sajadinejad MS, Asgari K, Molavi H, Kalantari M, Adibi P. Psychological issues in inflammatory bowel disease: an overview. Gastroenterol Res Pract. 2012; 2012:106502. PMID: 22778720.
Article12. Hall NJ, Rubin GP, Dougall A, Hungin AP, Neely J. The fight for ‘health-related normality’: a qualitative study of the experiences of individuals living with established inflammatory bowel disease (IBD). J Health Psychol. 2005; 10:443–455. PMID: 15857873.
Article13. Jelsness-Jørgensen LP, Bernklev T, Henriksen M, Torp R, Moum BA. Chronic fatigue is associated with impaired health-related quality of life in inflammatory bowel disease. Aliment Pharmacol Ther. 2011; 33:106–114. PMID: 21083587.
Article14. Yoo S, Jung YS, Park JH, et al. Fatigue severity and factors associated with high fatigue levels in Korean patients with inflammatory bowel disease. Gut Liver. 2014; 8:148–153. PMID: 24672655.
Article15. Thia KT, Sandborn WJ, Harmsen WS, Zinsmeister AR, Loftus EV Jr. Risk factors associated with progression to intestinal complications of Crohn's disease in a population-based cohort. Gastroenterology. 2010; 139:1147–1155. PMID: 20637205.
Article16. Kim YS. What is the important issue to prevent the postoperative Crohn's disease? Intest Res. 2014; 12:85–86. PMID: 25349572.
Article17. Danese S, Fiorino G, Mary JY, et al. Development of red flags index for early referral of adults with symptoms and signs suggestive of Crohn's disease: an IOIBD initiative. J Crohns Colitis. 2015; 9:601–606. PMID: 25908718.
Article18. Kim ES, Kim WH. Inflammatory bowel disease in Korea: epidemiological, genomic, clinical, and therapeutic characteristics. Gut Liver. 2010; 4:1–14. PMID: 20479907.
Article19. Devlen J, Beusterien K, Yen L, Ahmed A, Cheifetz AS, Moss AC. The burden of inflammatory bowel disease: a patient-reported qualitative analysis and development of a conceptual model. Inflamm Bowel Dis. 2014; 20:545–552. PMID: 24407484.20. Dignass A, Van Assche G, Lindsay JO, et al. The second European evidence-based consensus on the diagnosis and management of Crohn's disease: current management. J Crohns Colitis. 2010; 4:28–62. PMID: 21122489.
Article21. Ye BD, Yang SK, Shin SJ, et al. Guidelines for the management of Crohn's disease. Intest Res. 2012; 10:26–66.
Article22. Choi CH, Kim YH, Kim YS, et al. Guidelines for the management of ulcerative colitis. Intest Res. 2012; 10:1–25.
Article23. Walker JR, Ediger JP, Graff LA, et al. The Manitoba IBD cohort study: a population-based study of the prevalence of lifetime and 12-month anxiety and mood disorders. Am J Gastroenterol. 2008; 103:1989–1997. PMID: 18796096.
Article24. Mittermaier C, Dejaco C, Waldhoer T, et al. Impact of depressive mood on relapse in patients with inflammatory bowel disease: a prospective 18-month follow-up study. Psychosom Med. 2004; 66:79–84. PMID: 14747641.
Article25. Addolorato G, Capristo E, Stefanini GF, Gasbarrini G. Inflammatory bowel disease: a study of the association between anxiety and depression, physical morbidity, and nutritional status. Scand J Gastroenterol. 1997; 32:1013–1021. PMID: 9361174.
Article26. Kim ES, Cho KB, Park KS, et al. Predictive factors of impaired quality of life in Korean patients with inactive inflammatory bowel disease: association with functional gastrointestinal disorders and mood disorders. J Clin Gastroenterol. 2013; 47:e38–e44. PMID: 23090047.27. Bernklev T, Jahnsen J, Henriksen M, et al. Relationship between sick leave, unemployment, disability, and health-related quality of life in patients with inflammatory bowel disease. Inflamm Bowel Dis. 2006; 12:402–412. PMID: 16670530.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Musculoskeletal Manifestation in Inflammatory Bowel Disease
- Daily Life Difficulties and Disease Awareness of Patients With Narcolepsy
- First aid with color atlas for the use of intestinal ultrasound for inflammatory bowel disease in daily clinical practice
- Can vitamin D supplementation help control inflammation in inflammatory bowel disease beyond its classical role in bone health?
- Results of the first survey for the current status of inflammatory bowel disease management in Asian countries